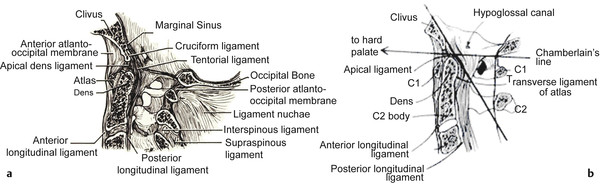
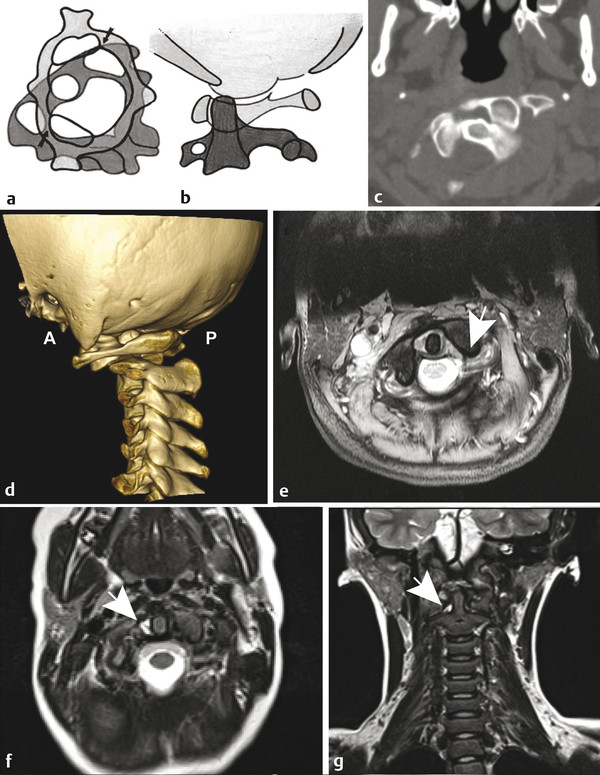
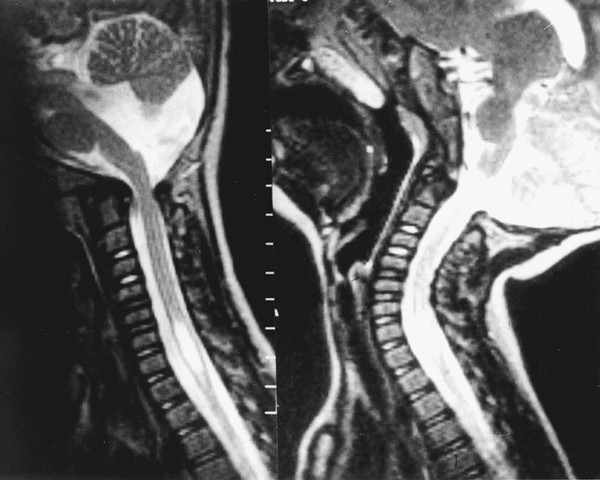
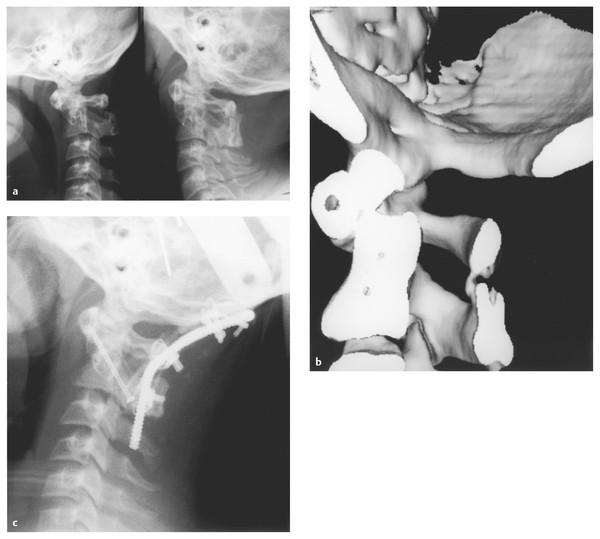
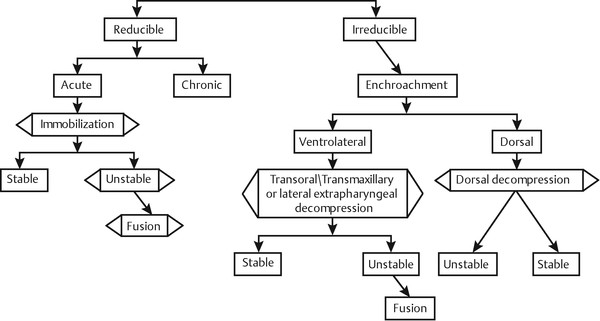
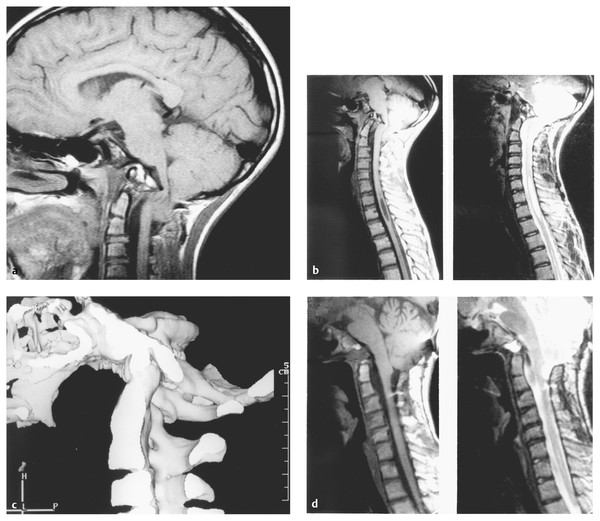
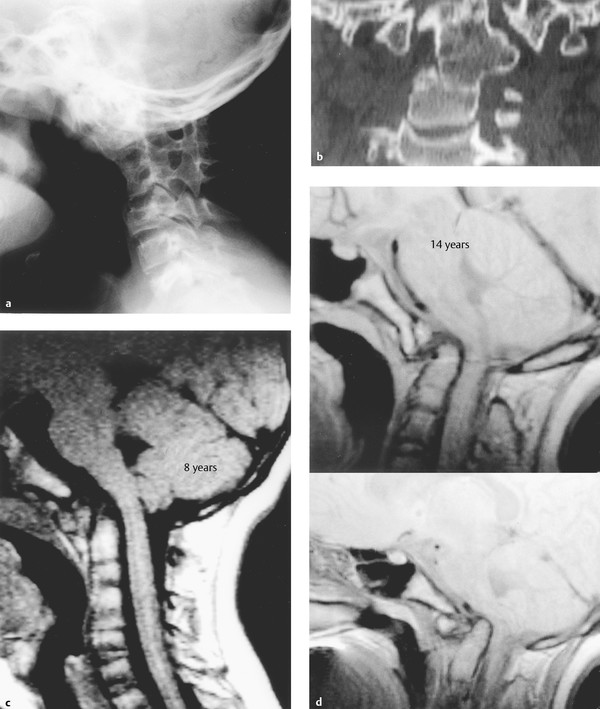
Relevant Anatomy and Biomechanics The occipitoatlantoaxial complex is the most mobile and complex joint of the axial skeleton.2 Flexion and extension occur at the occipitoatlantal and the atlantoaxial articulations (▶ Fig. 27.1a,b). In children, the anteroposterior translation between the anterior arch of atlas and dens, the “predental space,” can be up to 5 mm until the age of 8 years and should be less than 3 mm in adults.2,7,8 Cervical rotation occurs primarily at the atlantoaxial joint. Atlantoaxial rotation beyond 35 degrees is associated with a risk for contralateral vertebral artery injury.4 Further rotation exceeding 45 degrees is associated with facet interlock between the atlas and axis vertebrae (▶ Fig. 27.2 a–g). This has particular significance in atlas assimilation, for children participating in contact sports, and for those who undergo excessive rotation of the head during general anesthesia or forceful head manipulations. The absence of uncovertebral joints as well as the the horizontal orientation of facets in children also raise the risk for upper cervical injury. Fig. 27.1 (a) Craniocervical junction anatomy with ligaments and bursae present. (b) Line drawing depicting the cervicobasilar relationships. Fig. 27.2 (a,b) Rotational changes at atlantoaxial articulation as a result of rotation exceeding 40 degrees with an interlock (arrows). (c) Axial computed tomographic scan showing C1–C2 interlock. (d) Three-dimensional reconstructed image indicates the abnormal bony configuration. A, anterior; P, posterior. (e) Axial T2-weighted image indicates rotation of C1 on axis with a torn cruciate ligament (arrow). (f) Axial T2-weighted image in another patient indicates increased signal intensity within the alar ligament, adjacent to the odontoid (arrow). (g) Coronal T2-weighted image indicates the presence of a torn alar ligament (arrow) in the same patient. The cervical paraspinal musculature and ligamentous complex impart stability to the craniocervical articulation and also form the pathogenic basis of various craniovertebral junction anomalies.2,9 The most critical craniocervical ligament is the transverse ligament, which maintains mechanical stability of the atlantoaxial joint complex.10 It allows atlantoaxial rotation up to 47 degrees while preventing anterior subluxation of C1 on C2. The alar ligaments extend from the basion to the axis and serve to secondarily stabilize the C1–C2 joint and prevent extreme axial lateral rotation beyond 90 degrees.10 Alar ligamentous injury is typically associated with whiplash injuries. With disruption of the cruciate ligament, the load is then placed on the alar and the apical ligaments, which quickly become incompetent.7 Lymphatic drainage of the occipitoatlantoaxial joints is primarily through retropharyngeal nodes into the deep upper cervical lymphatic chain. These nodes also drain the nasopharynx, retropharyngeal area, and paranasal sinuses.2,11–14 Hence, a retrograde inflammatory change may affect the synovial lining of the craniocervical joint complex, with resultant effusion, instability, and subsequent possible neurologic deficit. This has been referred to as Grisel syndrome.11 The atlantoaxial joints are the most vulnerable and affected in majority of patients. In addition, the periodontal venous plexus and suboccipital epidural sinuses communicate with the pharyngovertebral veins. This can result in osteomyelitis of the craniocervical joints due to paravertebral infections.13 The vertebral and the occipital arteries provide blood supply to the craniocervical region.13 The vertebral arteries give rise to anterior and posterior ascending branches that anastomose in an apical arcade and supply small perforating branches to the axis body and odontoid process.15 In addition, ascending anterior branches receive contributions from the carotid arteries. The cartilaginous plate between the dens and axis body prevents the development of a vascular communication between the axis and its odontoid process. This accounts for formation of a sequestrum in type 2 odontoid fractures and the development of os odontoideum.2 Cervicomedullary pathology may also present with false localizing symptoms due to medullary decussation at the foramen magnum and secondary involvement of the lower cervical cord segments due to venous stasis resulting from extramedullary compression of the cervicomedullary junction.5 Craniovertebral anomalies are typically developmental disorders of the cartilaginous neurocranium and adjacent vertebral skeleton.16 In addition, a wide variety of congenital, hereditary, and acquired anomalies may exist either individually or in combination (see box “▶ Classification of Craniovertebral Anomalies”). Classification of Craniovertebral Anomalies Congenital anomalies and malformations Occipital sclerotome malformations: proatlas remnants, clivus segmentations, condylar hypoplasia, atlas assimilation Atlas malformations: bifid atlas, assimilation, fusions, absent arches Axis malformations: segmentation defects, odontoid dysplasias Developmental and acquired abnormalities Foramen magnum abnormalities Foramen stenosis: achondroplasia Secondary invagination: osteogenesis imperfecta, Hadju-Cheney syndrome, renal rickets, Paget disease Atlantoaxial instability Down syndrome Errors of metabolism: Morquio syndrome, Hurler syndrome Infections: Grisel syndrome, tuberculosis Trauma Inflammation: regional ileitis, juvenile rheumatoid arthritis, Reiter syndrome Tumors: osteoblastoma, eosinophilic granuloma, chordoma, neurofibromatosis Miscellaneous: Conradi syndrome, fetal warfarin, syringomyelia Underlying craniovertebral anomalies must be suspected in infants with skeletal dysplasias and syndromic disorders like Goldenhar syndrome and Conradi syndrome.17–20 Children with Down syndrome have a 14 to 20% incidence of atlantoaxial instability.2,21 In Morquio syndrome, a combination of atlantoaxial instability, C2–C3 segmentation failure, os odontoideum, and cervicothoracic abnormalities occurs in 30 to 50% of patients.2,21 With an underlying congenital craniocervical anomaly, secondary developmental and acquired phenomena may supervene, producing basilar invagination.22 Craniovertebral disorders present with a constellation of symptoms and signs that reflect dysfunction of the brainstem, cerebellum, cervical spinal cord, cranial nerves, cervical roots, and their associated vascular supply (see box “▶ Signs and Symptoms of Craniovertebral Anomalies: Insidious or Rapid Onset of Symptoms and Signs”). The onset may be insidious or rapid, and at times patients may present with false localizing signs. Infrequently, a rapid neurologic progression is followed by sudden death. More commonly, an antecedent history of trauma triggers symptoms that may progress rapidly. The authors feel strongly that children with nasopharyngeal infections and neck spasm (“torticollis”) must be suspected of harboring craniocervical instability unless it is proven otherwise. Temporary bracing and close follow-up with flexion–extension X-rays repeated on a weekly basis will aid in the identification of any underlying instability that can sometimes be masked by muscular spasm in acute presentations. Signs and Symptoms of Craniovertebral Anomalies: Insidious or Rapid Onset of Symptoms and Signs Head tilt Short neck, low hairline, limitation of neck motion Web neck Scoliosis Features of skeletal dysplasias Neck pain and posterior occipital headache Basilar migraine Hand or foot isolated weakness Quadriparesis/paraparesis/monoparesis Sensory abnormalities Nystagmus, usually downbeat and lateral gaze Sleep apnea Repeated episodes of aspiration pneumonia, dysphagia Tinnitus and hearing loss Vertigo An abnormal general physical appearance is often seen in children with congenital craniocervical abnormalities. The head may be tilted or cocked to one side in patients with atlantoaxial rotary subluxation or partial segmentation failure. The classic triad of the Klippel-Feil syndrome consists of an abnormally low hairline posteriorly, a short neck, and limitation of neck movement, which may present in conjunction with facial asymmetry and neck webbing.23 Scoliosis is often present. An abnormal stature and elevated scapula are seen with Sprengel deformity. Systemic skeletal anomalies are typically present, with craniovertebral abnormalities secondary to spondyloepiphyseal dysplasia, achondroplasia, and other types of dwarfism.19,24 Cervical and occipital pain occurs in up to 85% of children and is described as originating in the suboccipital region with radiation to the vertex.2,5 “Basilar migraine” occurs in 25% of children affected with basilar invagination and medullary compression and is due to associated compression of the vertebrobasilar vessels. Occipitoatlantoaxial instability may cause repeated trauma to the anterior spinal artery and the perforating vessels of upper cervical cord and medulla, leading to vascular spasm or occlusion and secondary neurologic deficits. The most common neurologic deficit encountered in the 1,700 children in our series was myelopathy. This was equally distributed with motor deficits involving monoparesis, hemiparesis, paraparesis, and quadriparesis. Myelopathy mimicking the “central cord syndrome” was frequently encountered in children with basilar invagination. Similarly, posterior column dysfunction was the most common sensory abnormality. Occasionally, children described an abnormal sensation in their hands or feet. In infants and toddlers, this may be recognized by constant rubbing of the affected limbs. Brainstem and cranial nerve deficits are usually evident by dysphagia and repeated episodes of aspiration pneumonia and sleep apnea. Not uncommonly, internuclear ophthalmoplegia is present, leading to a misdiagnosis of mesencephalic and upper pontine disturbance. Downbeat nystagmus was present more often in patients with an associated Chiari 1 malformation. Unilateral or bilateral paralysis or dysfunction of the soft palate and pharynx leads to repeated bouts of aspiration pneumonia as well as poor feeding and inability to gain weight. The most common cranial nerve dysfunction was hearing loss in 23% of children and is most commonly associated with Klippel-Feil syndrome. Vascular symptoms, such as intermittent attacks of altered consciousness, transient visual loss, vertigo, and confusion, occurred in 20% of children. At times, this was provoked by cervical extension or rotation or by manipulation of the head and neck. Plain radiographs of the cervical spine in lateral and anteroposterior views are supplemented by open-mouth and anteroposterior projection views of the foramen magnum.8 If instability is suspected, lateral extension and flexion views should be obtained.2,5 Several lines of reference have been described to correlate the position of neural structures with the associated osseous abnormality (▶ Fig. 27.1b).3,8 The Chamberlain palato-occipital line joins the hard palate to the posterior edge of the foramen magnum. In a normal individual, the tip of the dens should lie below this line or at most 3 to 5 mm above it.3 When the odontoid process ascends above this line, basilar invagination has occurred. We believe that the Wackenheim clivus–canal line (drawn along the clivus and extrapolated into the cervical spinal canal) is of great significance. The odontoid process must be ventral or tangential to this line under normal conditions, and it transects this line in basilar invagination, atlantoaxial dislocation, and anterior occipitoatlantal dislocation. The McRae foramen magnum line joins the anterior and posterior edges of the foramen magnum, and the tips of the dens must be below this line.1 A sagittal diameter of less than 20 mm at the cervicomedullary junction is associated with neurologic compromise.22 Magnetic resonance (MR) imaging aids in an ideal identification of the underlying neural abnormalities and associated osseous compression.8,24 Computed tomography (CT) with rapid-acquisition spiral technique and three-dimensional reconstruction is necessary to recognize the presence or absence of epiphyseal growth plates, the extent of fusion, segmentation defects, and “missing” osseous components, especially in infants with torticollis.8 In all the techniques of investigation, dynamic flexion–extension studies are necessary for assessing stability and the angular osseous relationships with underlying neural structures (▶ Fig. 27.3). This also provides information regarding reducibility and the optimal position of fixation if needed.2,5 Because of their routine availability, MR imaging and CT angiography have supplanted traditional angiography to identify obstruction or potential occlusion with dynamic positional changes.2 Fig. 27.3 Composite of magnetic resonance imaging of the craniocervical junction in the T2 mode. The flexed position is seen on the left and the extended position on the right. Note the instability at the craniocervical junction. A syrinx is seen in the lower cervical spinal cord. Factors that influence specific treatment are the following: (1) the etiology of the pathologic process (i.e., type of bony abnormality and the presence of Chiari malformation, syrinx, or vascular abnormalities); (2) the reducibility of the bony lesion (ability to restore normal anatomical alignment and relieve compression of the cervicomedullary junction); (3) the mechanics of compression and direction of encroachment; and (4) the presence of abnormal ossification centers and epiphyseal growth plates.2,6 The primary goal underlying surgical treatment is to relieve compression at the craniocervical junction (▶ Fig. 27.4a–c). In a reducible lesion, stabilization is paramount to maintain neural decompression. Irreducible lesions require decompression at the encroachment site. Ventral lesions require operative approaches through a transpalatopharyngeal decompression, a Le Fort drop-down maxillotomy, or the lateral extrapharyngeal route. Posterior or posterolateral decompression is required for dorsal lesions (▶ Fig. 27.5). If instability is present after decompression, a posterior fixation is mandatory for stability (▶ Fig. 27.6a–d). Fig. 27.4 (a) Composite of a lateral craniocervical radiograph in the flexed (left) and extended (right) position in an 11-year-old child with Down syndrome. A previous attempt at dorsal atlantoaxial arthrodesis failed. Instability and an os odontoideum are present. (b) Three-dimensional computed tomography of the craniocervical junction demonstrates the failed dorsal interspinous fusion between C1 and C2. An os odontoideum is present. (c) Postoperative lateral cervical spine and craniocervical radiograph. The halo vest is in place. A dorsal occipitoatlantoaxial arthrodesis is made with titanium loop instrumentation and a rib graft. Because of the gross instability at the occipitoatlantoaxial articulation, a transarticular screw between C2 and C1 completed the stabilization. Fig. 27.5 The treatment of craniovertebral abnormalities. Fig. 27.6 (a) Lateral magnetic resonance (MR) imaging in T1 mode in a 12-year-old girl with palsies of cranial nerves IX, X, and XII bilaterally. There is a ventral indentation into the inferior medulla by a bony mass proceeding from the inferior clivus. A hindbrain herniation is visualized. (b) MR imaging in T1 (left) and T2 (right) mode shows the ventral medullary and basilar artery compression. A hindbrain herniation and a cervicothoracic syrinx are visualized. (c) Three-dimensional computed tomography of the craniocervical junction viewed from within. A proatlas segmentation defect is seen. A protrusion from the inferior clivus extends into the ventral foramen magnum. There is basilar invagination present and atlas assimilation laterally. (d) Postoperative MR imaging in T1 (left) and T2 (right) mode visualizing the posterior fossa and cervical spine. The patient underwent a transpalatopharyngeal resection of the inferior clivus, proatlas segmentation bony abnormality, and odontoid process. Note the decompression and absence of the syrinx. The management of craniocervical instability in young infants secondary to conditions such as Goldenhar syndrome and osteogenesis imperfecta deserves special mention.2 It is essential to determine the potential for osseous development by identifying developing epiphyseal growth plates on thin-section CT. In these instances, we use custom-built cervical orthoses to impart occipitocervical stability while skeletal growth is allowed to occur. During follow-up, the cervical orthoses are replaced periodically and diagnostic studies repeated to monitor the craniocervical region. After adequate bone growth is achieved by 3 to 4 years of age, surgery is undertaken, as described above, if osseous stability has not yet occurred. Skeletal traction is applied with an MR imaging–compatible crown halo device.25,26 In children between 2 and 4 years of age, eight-point fixation is utilized with finger pressure that limits pin pressure to 1 to 1.5 lb of torque. At 5 years of age, 4 lb of maximum pin pressure is utilized. Traction is initiated at 3 to 4 lb and does not exceed 7 lb. Reducible lesions that are the result of inflammatory states or recent trauma will respond to conservative treatment with external immobilization once reduction is achieved. If this does not occur or if the condition is not the result of trauma or infection, surgical fixation is mandated. In children, traction is applied in the operating room under general anesthesia. A cervical collar is used for protection during intubation maneuvers. After the initial use of general mask anesthesia, fiber-optic intubation is undertaken through the mask. Halo ring traction is then applied during pharmacologic muscle relaxation with general anesthesia. Neurophysiologic monitoring (somatosensory evoked potentials) is maintained during these maneuvers, in addition to image documentation with intraoperative computed tomography with three-dimensional display.27 This is a recent technique developed in the last 4 years. Basilar invagination, craniovertebral junction dislocation, and other irreducible states warrant this attempt at “reduction.” It has proved successful in 36 of 52 patients whose abnormalities were felt to be “irreducible.” These patients will not require ventral decompression, but posterior decompression and stabilization. If surgical fixation is planned simultaneously, an interim clinical assessment is made after reversal of anesthesia while intubation is maintained. In the case of a grossly unstable but reducible state, a crown halo vest is placed under general anesthesia, and the child is then turned prone on the operating table. The posterior struts are removed to enable dorsal fixation while the ventral struts are maintained for immobilization and to aid postoperative reapplication of the halo vest. In addition to the traditional transoral transpharyngeal surgical approaches, transnasal and transcervical endoscopic techniques have evolved to establish surgical access for the management of irreducible ventral craniocervical lesions.28,29 The transoral transpharyngeal route offers excellent surgical exposure to address a wide range of ventral craniovertebral junction lesions,30 but it is associated with the surgical morbidity of postoperative dysphagia and the need for postoperative intubation after surgical dissection through the palate and pharynx. The endonasal approach enables access to the rostral craniocervical junction, and it avoids prolonged postoperative intubation and the risk for oropharyngeal dysfunction associated with transoral procedures. Conversely, the surgical access corridor is restricted in the lateral and inferior limits of the exposure, and endoscopic pharyngeal closure is not made. The endoscopic transcervical route circumvents the need for oropharyngeal dissection, and it offers a sterile operative field while enabling adequate exposure.29 Spinal deformity, obesity, or ventral chest wall constraints, however, limit its application. It is also associated with a risk for airway swelling and dysphagia. An endoscopic transoral approach has also been proposed that obviates the need for resection through the hard palate while improving surgical access and endoscopic visualization.31 Although these evolving techniques may potentially improve patient outcomes, long-term studies with a direct comparison of outcomes are needed to better address the role of these emerging techniques. Atlantoaxial osseous fusion requires immobilization for at least 3 months. We utilize custom brace/vest immobilization for 5 to 6 months when only a bony fusion is made. The rate of failure of fusion reaches 50% when immobilization is inadequate. Dorsal wire fixation should be avoided because skeletal growth will cause stress fatigue, with resultant wire fracture or disruption and possible injury to spinal cord.2,32,33 In the management of pediatric craniocervical fusions, the age of the patient, the occipitoatlantoaxial dimensions, and the ability to achieve screw purchase for an instrumented fusion must be taken into consideration. The senior author (A.H.M) has used full-thickness rib to span the dorsal structures in children younger than 5 to 6 years of age; an attempt at instrumentation is made in children past that age.25,34 The treatment guidelines outlined above have yielded excellent surgical results, with no mortality or gross morbidity, in more than 1,700 children treated via anterior, lateral, or posterior surgical routes. Grisel syndrome is defined as spontaneous atlantoaxial subluxation following parapharyngeal infection.2,11–13,15 This inflammatory subluxation is attributed to metastatic inflammation causing ligamentous stretching, subluxation, muscle spasm, and regional hyperemia with decalcification of ligamentous attachments. Thus, these children may present with torticollis, stiff neck with neck pain, or neurologic deficit. This may be after a case of tonsillitis, mastoiditis, retropharyngeal abscess, or otitis media or after a surgical procedure to correct one of these states. Children younger than 12 years of age are most commonly affected because of their relative ligamentous laxity and atlas vascularity. Treatment involves CT and MR imaging. These identify the underlying abnormal anatomy and infection. It is critical that the source of infection be eliminated. Stabilization is achieved with a sterno-occipital mandibular immobilizing brace or a halo vest. In the acute phase, a Philadelphia collar may be applied to allow careful monitoring of respiratory function. Once the infection is under control, it is important that the craniocervical dynamics be carefully assessed. In the author’s own series of 52 children, a fusion procedure was required in 2 patients.2 A delayed diagnosis of torticollis and ligamentous instability following an upper respiratory infection in infants often confounds effective treatment. Atlas assimilation is defined as segmentation failure between the fourth occipital and first spinal sclerotome. This occurs in 0.25% of the population; it may be unilateral, bilateral, segmental, or focal and in most instances occurs in conjunction with other abnormalities. Atlas assimilation was present in 380 of 3,300 patients with craniocervical abnormalities evaluated in an initial series of the senior author.22 A Chiari 1 malformation is typically present in more than one-third of such individuals.35 Associated segmentation failure of the second and third cervical vertebrae leads to atlantoaxial instability that often progresses to a reducible basilar invagination (▶ Fig. 27.7a–d). This is more common in children younger than 14 years of age, after which irreducible basilar invagination occurs. During the phase of reducibility, prolific granulation tissue crowning the odontoid process aggravates cervicomedullary compression. In irreducible basilar invagination, an associated horizontally oriented clivus and abnormal grooving occur behind the occipital condyles as a result of upward migration of the axis vertebra onto the assimilated atlas, leading to irreducibility (▶ Fig. 27.8a,b). Hence, atlantoaxial dislocation or basilar invagination is more likely to be reducible in children younger than 16 years. This is especially pertinent in the surgical management of hindbrain herniation syndromes because posterior decompression alone does not address the underlying craniocervical instability. Fig. 27.7 (a) Lateral cervical spine and skull radiograph in a 14-year-old with neck pain following a football incident. The patient presented with weakness in the upper limbs and a diminished gag reflex with mirror hand movements. Note the segmentation failure at C2 and C3. (b) Frontal two-dimensional computed tomographic reconstruction of the craniocervical region identifies atlas assimilation and an abnormal position of the odontoid process in a 14-year-old. (c) This child had previously undergone magnetic resonance (MR) imaging for neck pain at 8 years of age. There is a mild atlantoaxial dislocation with probable atlas assimilation. However, the cervicomedullary junction is not compressed. (d) Composite of T2-weighted MR imaging in the midline (left) and paramedian (right) locations. The MR imaging at the age of 14 years now shows gross atlantoaxial dislocation with basilar invagination of the odontoid process into the foramen magnum, compressing the inferior medulla.
27.2 Classification of Craniovertebral Junction Abnormalities
27.3 Epidemiology
27.4 Signs and Symptoms
27.5 Imaging
27.6 Surgery
27.7 Specific Conditions Affecting Children
27.7.1 Grisel Syndrome
27.7.2 Assimilation of the Atlas and the Klippel-Feil Syndrome
Craniovertebral Junction
Only gold members can continue reading. Log In or Register to continue

Full access? Get Clinical Tree








