Schematic representation of patient-oriented clinical information system. Data from different sources are accumulated in one central database. A central repository communicates with other CIS outside the organization silo. Pertinent clinical data is consumed by clinicians in human-centered displays or alerts integrated seamlessly into clinical workflow
8.3 Computer-Based Clinical Decision Support (CDS)
8.3.1 Classification
The most recent CDS definition is “The use of information and communication technologies to bring relevant knowledge to bear on the healthcare and well-being of a patient” [18]. This definition comes from the answer to the question, “How do health information systems link knowledge to clinical events,” and demonstrates the pathway toward the translation of better health information into better health [19].
- 1.
To make clinical data easier to access or interpret
- 2.
To foster optimal problem solving, decision-making, and actions
Alerting decision support is an automatic notification of target providers with time-sensitive information. Alerts are based on rules and can be disruptive (requiring immediate action to continue workflow) or non-disruptive (can be dealt with after workflow has been completed) and can be customized with different degrees of urgency.
“Interpretation” decision support gathers, coordination, and analyzes patient data before presenting the result of that interpretation to the clinician. The most classic examples are ECG, ABG, severity scores interpretation, and outcome predictions.
“Assisting” decision support helps providers to make clinical decisions. The kernel of this function is a predictive knowledge database focused on a particular problem or task. Assistance for physician orders is the most common usage of this type of decision support.
“Critiquing” decision support is based on formalized guidelines or conditions; it estimates user’s decision and gives an alternative suggestion or a rating of adequacy within pre-defined set of data. This type of support does not aid in initial clinical decision formulation.
“Diagnostic” decision support provides a hypothesis based on entered patient information and available clinical and paraclinical data; this type of support typically generates a diagnosis, or a list of possible diagnoses ranked probabilistically is generated.
“Management” decision support is oriented toward the total care of the patient. This support suggests the “optimal” decision based upon the information currently known by the system. Computerized clinical practice guidelines are an example of this model of decision support.
While the above attempts to define the various forms of common decision support, there is no commonly accepted CDSS classification. Mentioned above process of CDSS building can provide some ideas about possible classification, based on data acquisition, processing, and usage.
Based on data processing or data transformation, all existing CDSS can be divided into two large groups—knowledge-based driven (rules based so-called “expert systems”) and non-knowledge base driven (machine learning, artificial intelligence, pattern recognition based etc.) [23].
Another classification considers only the timing of support, type of action (passive or active support, disruptive or non-disruptive), and usability [24].
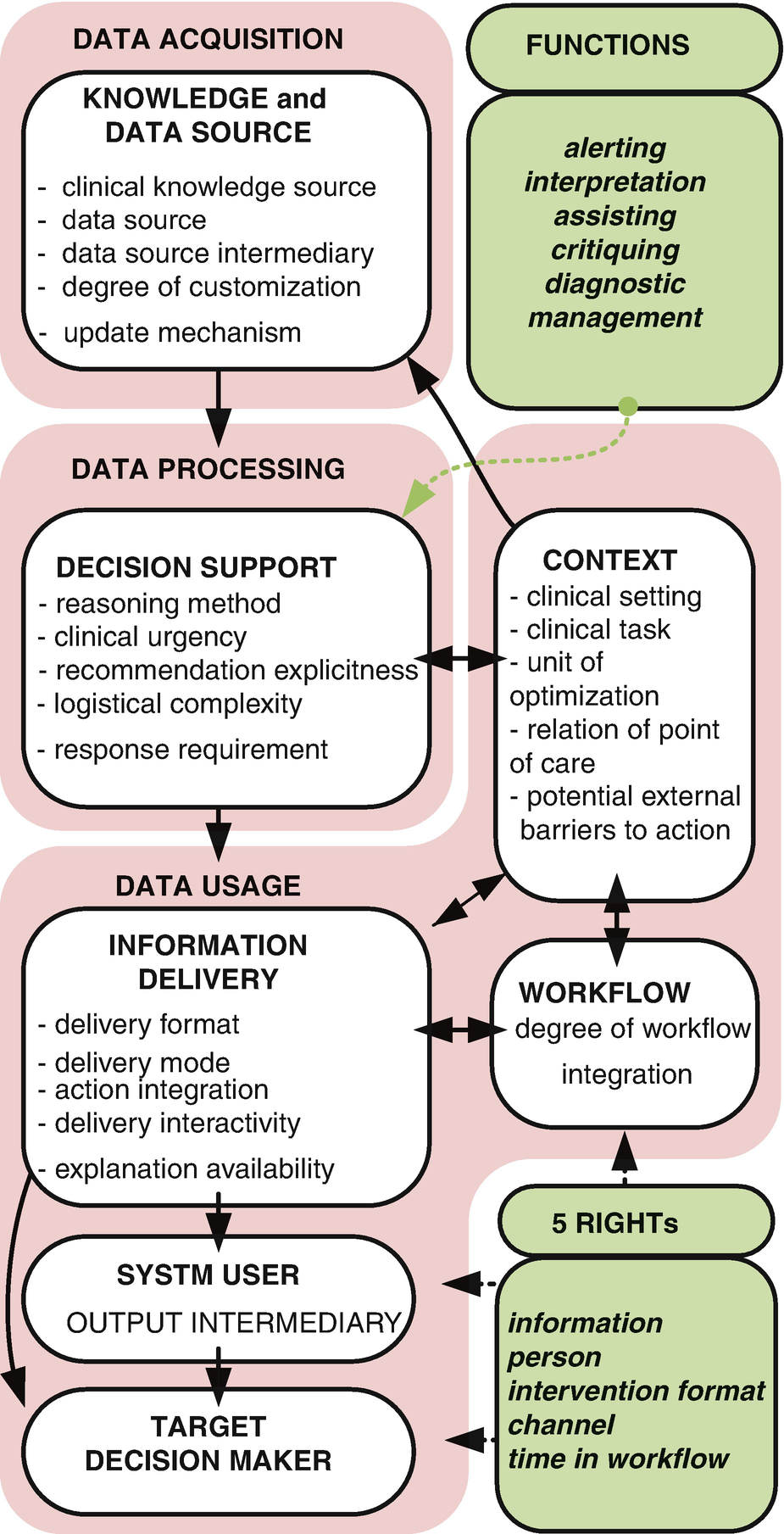
Complexity of interaction in DSS classifications
Consumes the right information
Delivered to the right person
In the right intervention format
Through the right channel
At the right time in workflow
8.3.2 Historical Perspective
The earliest versions of hospital information systems were almost exclusively focused on the financial performance of the institution. The primary function of those systems was to process patients’ demographic data and to merge it with itemized billing data to produce invoices for care provided [27]. The first clinical use cases were developed on top of these systems in the 1970s as a byproduct of the financial information management needs.
With the rapid progression and reduced cost of microchips, computer usage in ICU extended to laboratory and patient management data file [28]. Subsequent generations of microcomputers brought better access to data at lower cost and raised interest in CDS. However, initially CDS was used to improve the efficiency and reliability of production scheduling and financial analysis. It was rarely applied to assist with the day to day practice of clinical medicine [29].
During the 1990s vendors focused on fragmented solutions, and bedside terminals still not developed adequately support needs at point of care. Often system failed to be implemented not considering to balances advance in information technology with advances and needs in clinical practice management [30].
Historically electronic systems in hospitals were designed and focused on improving the operation of a single department [31]. They were developed in departmental silos and largely ignored the impact they had on patient care delivery outside of that silo.
The modern CIS continue to have poor communication tools between clinician themselves in general and patients and their families in particular [32]. Exclusion of patients from active involvement in their own care is a significant problem that increases deficiencies in safety and patient-centered healthcare. Finally, the availability of modern sophisticated equipment or CIS tools at the point of care and extended access to evidence base knowledge do not guarantee by themselves optimal patient care [33].
The current infrastructure nurtures fragmented, provider-oriented care delivery and impedes effective communication, particularly at the time of care transitions (admission, transfer or shift change).
Regardless of all previous efforts today, computer technology could not reliably diagnose patient’s disease or prevent deterioration.
Improve quality, safety, and efficiency and reduce health disparities.
Engage patients and families in their healthcare.
Improve care coordination.
Improve population and public health.
Ensure adequate privacy and security of health information.
8.3.3 CDS in ICU
- 1.
Diagnostic
- 2.
Therapeutic
- 3.
Administrative [36]
Few studies report the clinical information needs of clinicians in ICU [38]. EMRs appear to be inefficient for clinical information presentation in this setting and are not optimized for the collaborative decision-making models prevalent in the ICU [39]. ICU is multidisciplinary and collaborative practice of physicians, nurses, and other clinical providers interpreting the same data from different point of view and mostly different data sources. This can impair communication and development shared mental model that is essential to good outcomes in critical care [40]. A well-designed study by Morrison et al. demonstrates several difficulties the ICU multidisciplinary team have when interacting with each other and using an electronic record compared with a paper record [41].
8.4 Critical Care-Focused CDSS
8.4.1 Ambient Intelligence as a Concept
Information overload with delayed and out-of-context data presentation is one of the most important reasons for the failure of health information technology (HIT) in hospital environments. This problem is particularly acute where the intensity of care necessitates the use of multiple monitors and life-sustaining equipment and interventions that amplify the amount of data for each patient. Rather than directly attending to patients and their families, healthcare providers spend countless hours in front of the computer screen retrieving information and ordering specific patient care actions. Although the critical nature of a patient’s condition requires rapid decision-making, the clinician requires a significant time to retrieve useful information from a vast pool of data, promoting errors and management delays [13].
8.4.1.1 Case Study 1: Situation Awareness Dashboard for Acute Care (AWARE)
Clinical decision-making is often hindered by patient information that is difficult to access and use, which increases the potential for error and delays treatment.
AWARE dashboards (multi-patient and single-patient viewers) reduce information overload by facilitating access to key information needed for timely medical and interventional decision-making at the point of care.
AWARE “sniffers” (rule-based smart alerts) continuously survey both the patient condition and provider actions detecting potential mismatches and preventing potential errors before they occur.
AWARE whiteboard, task-list, readiness for discharge and claim patient functions facilitate communication between team members and during transitions of care, thereby preventing common errors of communication omission.
AWARE checklist and rounding tool assists providers in developing and executing a coordinated daily plan of care. The easy-to-use interface minimizes clerical burden while simultaneously assuring adherence to patient-centered best care practices and regulatory requirements.
AWARE feedback and reporting tool enables easy access to quality improvement metrics and patient outcomes for clinicians and oversight groups, which facilitates rapid-cycle-changes based on continuous feedback.
Applications built according to the AWARE principles will reduce information overload and the potential for error, facilitate adherence to practice guidelines, facilitate clear communication between all members of the ICU team, and provide the patient and family with a patient-centered view of the medical record, to facilitate understanding and collaborative decision-making.
- 1.
Task-specific, concept-oriented views of patient data—the right data, in the right place at the right time. AWARE organizes appropriate data, determined by a systematic review of end user data needs, into appropriate task-oriented information packages (Fig. 8.3).
- 2.
Knowledge translation—real-time evidence-based checklists and smart alerts are incorporated.
- 3.
Collaborative workspace—real-time plan of care with patient-specific tasks, status checks, and reminders which provide a location to communicate clearly the goals of care and their status to all members of the multidisciplinary team including the patient and family.
- 4.
Reports—scheduled and on demand unit/hospital level reports of quality metrics will be available for local and national reporting.
- 5.
User interface—providers interact with the system through secure fixed and mobile computer interfaces. These interfaces are built according to human-centered design principles and are integrated into ICU workflow in a manner that facilitates, rather than disrupts care delivery.

AWARE multi-patient viewer
8.4.1.2 Case Study 2: Electronic Smart Check Lists
The quality of care as well as prevention of errors can be improved by checklist usage. Smart checklists help to support the potential limits of human memory and attention during complex tasks in environments rich with critical events [42].
Checklists are increasingly being used in surgical practice and ICUs after a series of publications demonstrating their potential to improve outcomes and to reduce the healthcare cost in critically ill patients, through reduced errors and increased compliance with evidence-based practice [43–45].
A “to-do list” is the simplest example of checklist; this type shows one of the strongest impact on routine practice, as has been demonstrated with a five-item checklist which reduced dramatically central venous catheter-related infections [46].
At the beginning of 2008, the World Health Organization published a WHO Surgical Safety Checklist for use in the operating theatre environment [47]. The implementation of the WHO SSC was associated with robust reduction in morbidity and length of in-hospital stay and some reduction in mortality [48]. Some European countries have gone so far as to make this checklist mandatory nationwide [49].
The absence of standardization and unpredictable physician attitudes toward checklists make their implementation complicated and can result in failure to produce constant and sustainable compliance [42]. Inconsistent usage of checklists in real patient care leads to poor compliance and therefore compromises the checklist’s effectiveness [50]. On the other side, strict and mandatory application of checklists can result in an “autopilot mentality” and compromise the quality of patient care [51, 52]. Early engagement of stakeholders in the design and development of checklists is key to successful implementation. Such engagement most consistently results in patient safety behavior change [50]. Well-designed and implemented checklists encourage interdisciplinary discussions and support improved compliance with routine process of care issues [53].
An electronic decision support tool combined with daily rounding checklist can significantly reduce workload and diminish errors of routine daycare. A decision support tool provides relevant information for each checklist item. Integration into workflow and the availability of an override feature should be included in the tool.
8.4.1.3 Implementation of Rounding Tool and Integrated Smart Checklist
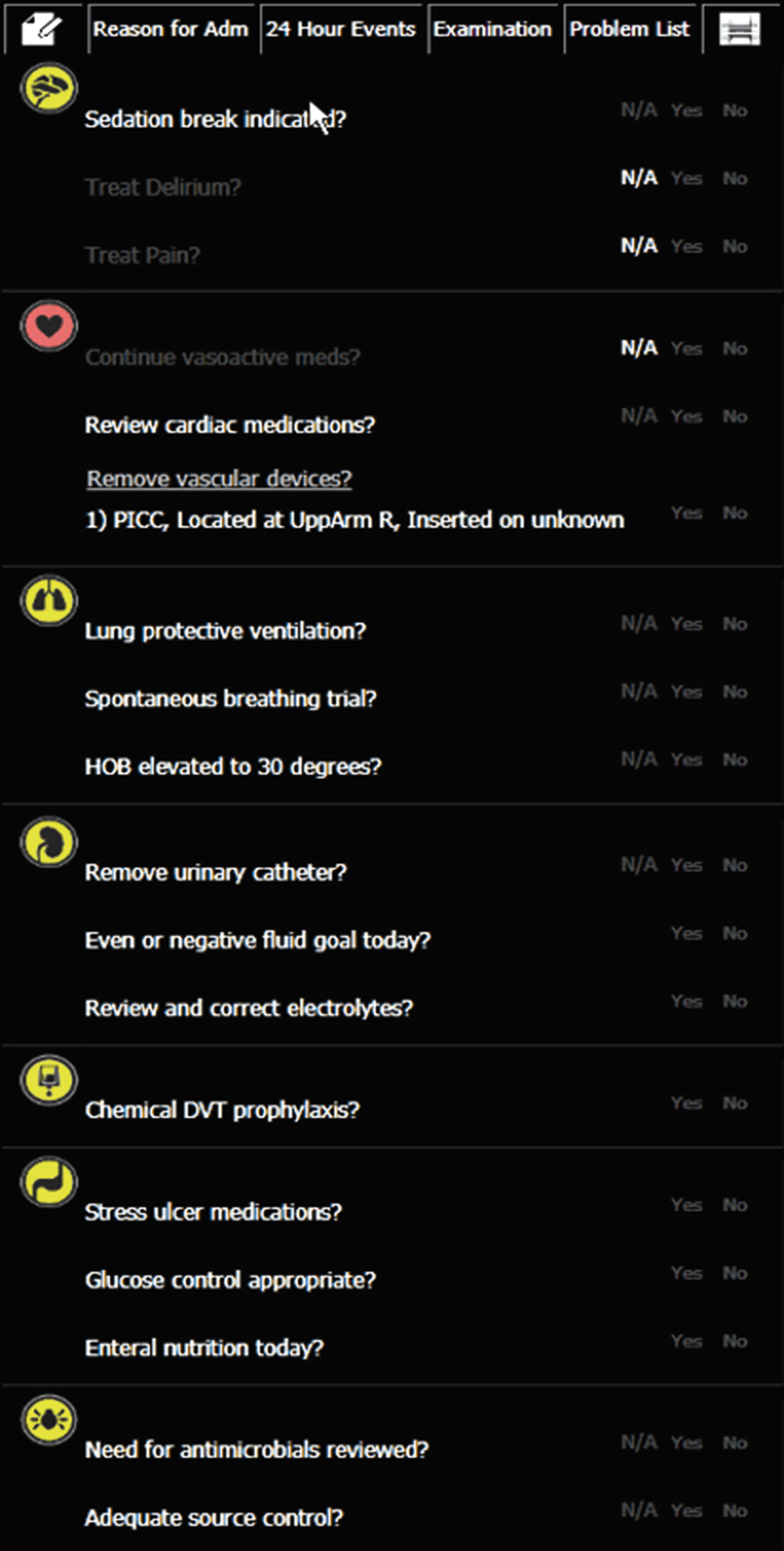
Daily rounding checklist with smart notifications and decision support
Users interaction with the electronic checklist can be incorporated into a general dashboard which provide point of care, administrative, quality improvement, and outcome monitoring functions. Checklist-based information can provide compliance with quality improvement metrics and can be combined with other reporting tools and provide real-time and consistent feedback to key stakeholders.
8.4.2 Smart Alerts
The diagnostic rule-based capabilities of decision support tools can be leveraged and used to support the early detection of common threating critical illness syndromes. Potential harm or potential development of critical situation can be predicted.
The diagnostic performance of decision support tools is affected by multiple factors including heterogeneity of clinical entities and syndromes, heterogeneity of data definitions in sources systems, data organization within the support tool database, logic design of the alert, and community disagreement about the diagnostic criteria [55].
The “smart alert” concept has evolved from the potential diagnostics capabilities of decision support algorithms. The purpose of these alerts is to provide early warning to a clinician that conditions exist that may lead to a critical event. The hypothesis being that early detection will allow the clinician to intervene and potentially prevent the critical event from occurring. Not unrelated to this, Silber and colleagues articulated the notion of “failure to rescue” [56]. The US AHRQ (Agency for Healthcare Research and Quality) Patient Safety Network defines failure to rescue as “shorthand for failure to rescue from a complication of an underlying illness or a complication of medical care” [57]. More clear definition is “a clinician’s inability to save a hospitalized patient’s life in the event of a complication (a condition not present on admission)” [58].
The most common cause of death in the ICU is a multiple organ dysfunction syndrome, caused by sepsis. The most frequently affected organs are the lungs, and the kidneys, followed by the brain and the immune system.
Rule-based clinical decision support tool can serve as an early detector of potential lung injury in ventilated patients (VILI Sniffer) [59, 60] or as an early detector of sepsis (Sepsis Sniffers) [61–63].
A truly intelligent surveillance system may be developed coupling the concept of “smart alerts” and “failure to rescue.” Early recognition and timely intervention of emerging sepsis could significantly reduce sepsis syndrome-related mortality. Having the dual role of syndrome detection and prevention, these tools require a combination of different decision-making algorithms focused on these roles. For this the decision support tools require data from multiple different sources including demographic, laboratory, and vital data, physician’s orders, nursing observations, clinical imaging, as well as knowledge-based data such as that outlined in “survival sepsis campaign bundles.”
8.4.2.1 Case Study 3: Smart Alert for Severe Sepsis Detection and Failure to Rescue
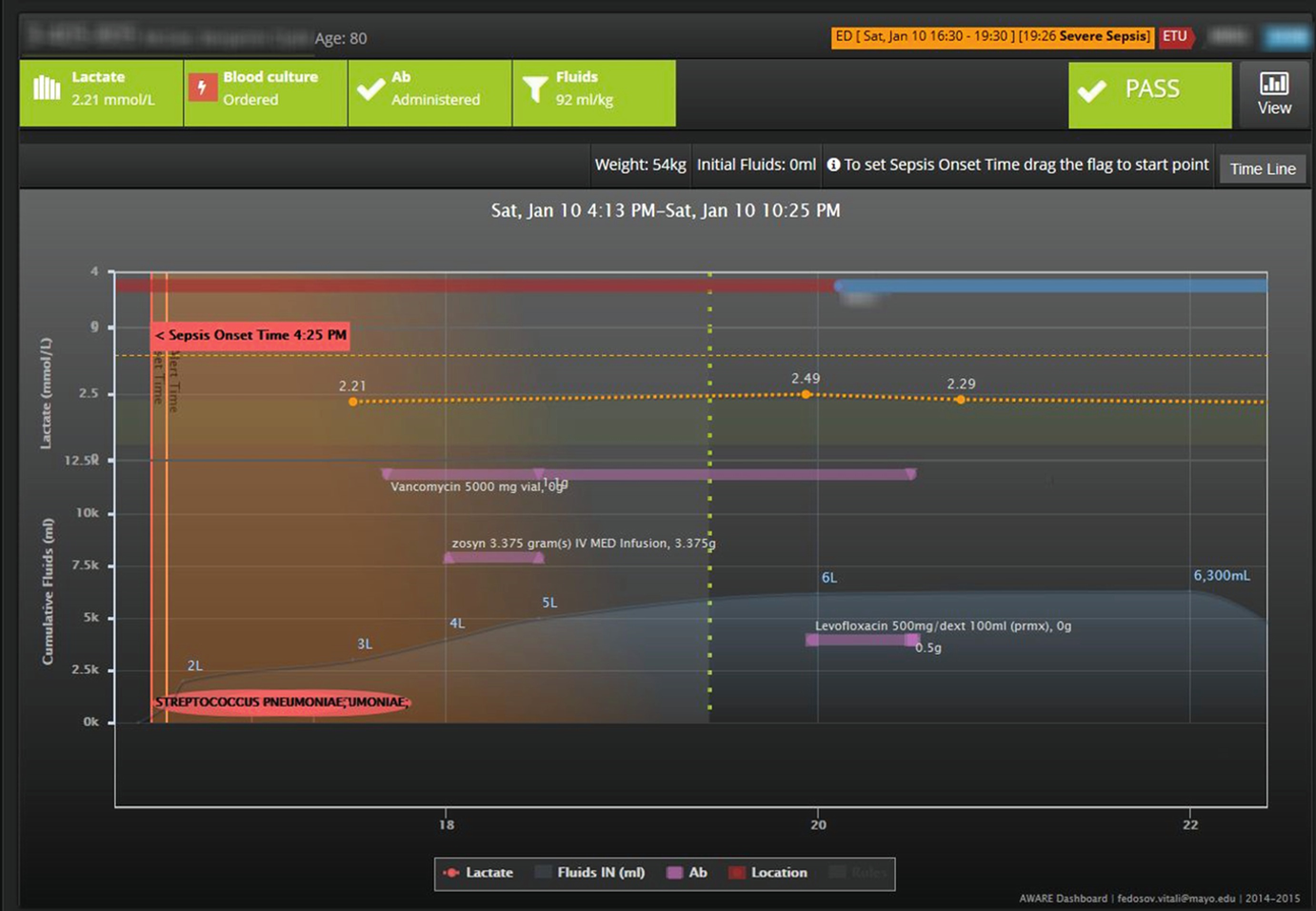
An AWARE-based integrated sepsis sniffer (Sepsis DART – Sepsis Setection And Responce Tool) combines sepsis detection with process of care tracking of sepsis bundle elements in format of “Control Tower”. These can be viewed for individual as well as populations of patients and provide real-time feedback to providers at the bedside. This data can be reused to generate the more traditional quality improvement reports in both static and interactive form
8.5 Modes of Information Delivery
8.5.1 Overview
When EMRs are introduced into practice, a consistent criticism from patients is that, their physicians are less engaged with them as a person and appear very distracted by the computer terminal [64]. Progress in technology must be leveraged to bring clinicians back to the bedside to use their skills as expert communicators and decision-makers. In the ICU, it is not uncommon to see physicians sitting some distance away from the patient and in room providers, pouring over data at their desktop computers. This is not a positive development. The development of high-speed wireless networks (Wi-Fi technology) greatly increases the potential of mobile devices in the ICU setting. A recent survey demonstrated that 40% of physicians in training use a tablet computer. Nearly half of them use a tablet at point of care to access the EMR [65]. Higher bandwidth connection for cellular networks (3G/4G) allows access to patient data off-campus. A recent systematic review of the impact of mobile handheld technology on hospital physicians’ work practices and patient care demonstrates benefits in the areas of efficiency and responsiveness; however, their impact on outcomes and workflow are unclear largely due to a paucity of studies and research in this area [66].
When designing clinical decision support tool notifications, developers have a number of choices to make with respect to how that information is best delivered to the front end user. Should the alert interrupt workflow and demand a response or should it sit passively in a dashboard in the hope that someone form the care team will notice. The correct choice is significantly influenced by complex human cognition factors. In the context of the, ICU mechanisms of notification and/or alert delivery include, face to face communication, written communication, labels, overhead announcements, direct paging, monitor alarms, email, and more recently, EMR-interface notifications and mobile device alerts.
An ideal communication tool would enable bidirectional, rapid, secure, and non-disruptive transmission of content-rich messages [31]. This tool should deliver the right information to the right person, in the right intervention format through the right channel at the right time in workflow [26].
Traditional computerized paging system notifications, widely implemented over 10 years ago, are frequently used today. With this modality of alert, individuals are directly contacted via a disruptive page. Most messages delivered in this way are nonurgent in character and are often cited as key disruptors health provider attention during important patient care activities [67–69]. No immediate feedback is available with traditional alphanumeric paging systems. Newer systems, capable of bidirectional paging and prioritization (SMS like system), have been found to be effective in reducing unnecessary interruptions, increasing daily efficiency, facilitating patient care, decreasing call backs, reducing interruptions of learning activities, and enabling better patient care [70].
E-mails delivered via different pathways such a computer message system or via cellular network on telephones or smartphones have been tested in different settings. Limited studies suggest that when implemented, teams demonstrate an improvement in clinical communication, patient care, and team relationship compared to baseline communication methods. On the downside, email communication has also been demonstrated to increase interruptions, fails to distinguish reliably between urgent and routine tasks, weakens interprofessional relationships, and can promote depersonalization and unprofessional behavior [31, 71].
With recent developments in mobile technology, increasingly push-methods are being utilized to deliver time-critical information to smartphones and tablets (iPad). Initial studies suggest that these might be a reliable mechanism for delivery of alerts with small latencies in response [72, 73]. While face validity and broad use of this method of message delivery in lifestyle applications are encouraging, limited experience and study of in the healthcare setting mean that widespread adoption of mobile alerts may have unanticipated consequences for patient safety and reliability of healthcare delivery.
8.5.2 Telemedicine (Cockpit/Control Tower Concept)
In response to increased demand for critical care expertise and lack of appropriately trained staff in some areas, ICU telemedicine solutions are growing at a rapid rate. The history of telemedicine in critical care dates back to the mid-1980s. Since then, the use of telemedicine as a simple transmission of information and findings from patient or healthcare provider to healthcare experts has spread beyond that initial use case to many areas of medicine. For example, Mayo Clinic, in common with many health systems, has invested heavily in developing a telemedicine projects in order to better serve the needs of its patients. Called, Mayo Clinic Health Connection, this solution uses a HealthSpot Platform(R) kiosk which allows patients with “minor, common health condition” to access healthcare providers [74].
Recent advances in networking technologies have accelerated the case for remote ICU care [75]. Recent meta-analyses have demonstrated that telemedicine in these settings, compared with standard care, is associated with lower ICU and hospital mortality [76]. These are interesting findings, but currently telemedicine in the ICU setting is very expensive, and the studies were not designed to identify which components of the telemedicine infrastructure are critical versus those which are not. Future solutions might include lower cost alternatives which reach more patients but offer fewer features.
Clinical decision support tools coupled with telemedicine in different settings are in use to support first-responders including paramedics and mobile emergency teams in different countries [77–80]. Automatic external defibrillators in public areas trigger an alert to emergency service when activated and are capable of sending ECG readings when used for resuscitation; LifeBot© is an example of an advanced combination of modern hardware technologies, decision support tools, and telemedicine solution. With decreased cost, increased computing power, and more widespread adoption of broadband wireless communication, this type of technology will become more common.
Complex CDSS have been used to triage and provide resolution for non-threating health conditions. In addition to information on the condition and simple advice to the patient, these decision support systems have also been used to prescribe medications [81] and to provide real-time audio and language translation for illiterate patients as they interact with the medical expert system [82]. In these situations, medical experts are contacted if the system fails to find an answer with a high sensitivity and specificity [83, 84]. While this is an advanced use case of the technology, increasingly the combination of CDSS and telemedicine is being deployed in different settings to support clinicians treating patients with both chronic and acute disease [85–87].
8.5.3 Problems to Overcome
The availability of a sophisticated digital data repository and health information technology infrastructure is a prerequisite for many of the decision support and alert systems discussed above. Critical challenges need to be overcome and questions answered before the widespread adoption of this infrastructure occurs. While many large health systems in the USA have been incentivized to adopt HIT, the cost of upgrading and implementing HIT greatly exceeds the budget of many hospital systems. In addition, the benefits in terms of patient-centered outcomes and healthcare cost savings have fallen far short of expectations. In addition, there are multiple case reports and studies which demonstrate that HIT can markedly disrupt established workflows and impede the very patient safety they are intended to improve. These factors can make HIT a tough sell to the frontline providers and impede implementation.
8.5.3.1 Integration
To facilitate transfer and usability of clinically relevant data among different hospitals’ electronic systems, standardized data element definitions are required for electronic intra-operability and clinical system interfaces. However, current data standards and regulation are insufficient to support the reliable exchange and reuse of data collected in the clinical domain of critical care between different healthcare institutions [88–90]. This greatly impedes secondary use of clinical data for population health, big data insights, and comparative effectiveness studies.
Modern ICUs use a wide variety of technologically sophisticated devices to capture the pathophysiological status of patients. Most of that data is aggregated at the level of departmental systems that require further integration into CIS. These systems generally serve specific departments (including ICU), are focused on the department’s clinical functions, and are implemented to optimize departmental activity. One of the most important trends in HIT is advancing the interoperability of hardware and software components (plug-and-play) [91]. HL7 has become the de facto standard for the integration of data within and between healthcare organization CIS. However, current system integrators are focused on improving small sub-processes, which are easier to automate, rather than the entire organization where the greatest problems and potential benefits exist.
Ultimately, the electronic environment will evolve to the point where all clinical data elements are integrated into a central data repository. This repository will provide rapid access to any data element for consumption by dedicated rules engines, dashboards, reports, and research queries. With this approach, bedside providers will be in a position to develop and test tools which facilitate timely, consistent, safe, and effective care.
8.5.3.2 Computer-User Interfaces
CIS usability is poor with little emphasis on end user needs and no consideration of the impact of that design on patient outcomes [92]. The engagement of patients and clinicians in the development and testing of appropriate user interfaces is essential if we are to deliver on the very real promise of improved outcomes with the adoption of CIS.
The user-computer interface can be evaluated along five axes: system response time, time required by users to learn the system, ability of users to remember what they learned, error rate, and subjective user satisfaction. However, user satisfaction often trumps other factors—if users do not “like” the system they will not continue to use it [93].
Previously little attention has been paid in the health informatics community to designing effective user interfaces that are acceptable to healthcare professionals. Different methods are being developed to analyze and predict everyday interactions with the computer system—input type, navigation patterns, eye-tracking, cognitive load, and time-on-task measurement, even “likeability” are increasingly being used to evaluate HIT systems—with a common purpose to support the development and implementation of more human-centered interface designs [13, 94–97].
8.5.3.3 Implementation
Careful consideration must be given to how clinical information will be integrated into the decision-making environment [98]. One of the challenges facing developers of CIS is to design products which enhance rather than disrupt decision-making in a working environment. Developing EMRs away from the final implementation environment potentially result in unintended consequences [99]. Regardless of all the expected positive aspects of information technology, it is essential to identify and prevent any potential negative effects of CIS implementation before they reach the level of the patient [100]. Without that consideration, we have simply replaced one type of medical error with another.
The reasons why systems succeed or fail are complex and are critically dependent on the quality of CIS implementation [101, 102]. Low adoption of CIS in the past was in part explained by a lack of communication between the established software developers and clinicians and remains one of the critical barriers to successful clinical implementation [103, 104]. A lack of common standards is also a failing point for integration [103].
CIS, like any complex human-technological system, is subject to failure and reliability issues. End users should be alert to this possibility and should be trained to deploy “a rescue plan” in an event of system shutdown. When clinical applications and lives are at stake, the immediate availability, preferably on site, of appropriately trained IT staff is essential. Intuitive user interface, non-disruptive integration into workflow, responsive IT, information security, and a low risk of system failure are key to building an EMR—friendly atmosphere among healthcare providers. Even minor issues with software or hardware can produce anecdotic conflicts and refusal to use otherwise excellent computerized tools [105–108].
8.6 Conclusions
We are at the beginning of an information revolution in healthcare with the overwhelming majority of effort focused on establishing the infrastructure required for electronic clinical data management and exchange. This focus quickly needs to shift to the primary healthcare mission—improving patient outcomes, improving system safety and consistency of care, and increasing value. It is vital that hospital information systems evolve from their database centric, accounting function to patient-centered systems which repay the huge investment made in them, in terms of lives saved and reduced healthcare costs. While initial results are mixed, progression toward this goal will be facilitated by improved human-computer interfaces next-generation smart clinical decision support systems; a move toward mobile, low-cost, connected hardware and medical devices; true interoperability and data exchange between silos of care; patient engagement; and secondary use of clinical data for the benefit of populations.

Full access? Get Clinical Tree


