10 The hallmark feature of neurofibromatosis 2 (NF2) is a slow-growing tumor on the eighth cranial nerve in both ears. This nerve has two branches. The acoustic nerve enables people to hear by transmitting sound sensation to the brain. The vestibular nerve function is related to balance. The tumors are known as vestibular schwannomas because they originate in Schwann cells that help to form the myelin sheath around nerves in the central nervous system. People with NF2 are at increased risk of developing other types of nervous system tumors as well. These include spinal schwannomas that tend to grow within the spinal cord and between the vertebrae. People with NF2 may also develop ependymomas and meningiomas, tumors that grow along the membranes covering the brain and spinal cord. Others may develop a typical type of cataract (juvenile posterior subcapsular lenticular opacity) or, more rarely, orbital meningiomas. These typical features of NF2 are discussed in detail later in this chapter. The current diagnostic criteria for NF2 are listed in Table 10–1. These criteria are based on those originally developed in the same 1987 National Institutes of Health (NIH) Consensus Conference that established criteria for an NF1 diagnosis,1 which, in 1990, were updated.2 The original criteria establish bilateral tumors of the eighth cranial (auditory) nerve as a hallmark feature of NF2. Additional criteria were proposed by Evans and colleagues3 in 1992 so that physicians could recognize rare cases of NF2 that do not present the hallmark feature of bilateral tumors of the eighth cranial nerve. The most current criteria are those established by the Clinical Care Advisory Board of the National Neurofibromatosis Foundation, which, in 1997, proposed further refinements of the diagnostic criteria.4
Diagnosis and Overall
Management of
Neurofibromatosis 2
| Individuals with the Following Clinical Features Have Confirmed (Definite) NF2 | Individuals with the Following Clinical Features Should Be Evaluated for NF2 (Presumptive or Probable NF2) |
| Bilateral vestibular schwannomas or | Unilateral vestibular schwannoma before age 30 plus at least one of the following: |
| Family history of NF2 (first-degree relative) plus |
|
| Unilateral vestibular schwannoma before age 30 or |
|
Any two of the following:
| Multiple meningiomas (two or more) plus unilateral vestibular schwannomas before age 30 or one of the following:
|
Adapted from Gutmann DH, Aylsworth A, Carey JC, et al. The diagnostic evaluation and multidisciplinary management of neurofibromatosis 1 and neurofibromatosis 2. JAMA 1997;278:54, with permission.
First, the NF Foundation committee recommended that the hallmark feature, bilateral eighth-nerve masses, be described as “bilateral vestibular schwannomas,” to reflect advancements in knowledge about the pathology and origin of these tumors. The committee also sought to make the diagnostic criteria more flexible, so that physicians could distinguish between people who definitely have NF2 (whose manifestations match the NIH criteria) and those who might have the disorder because their manifestations more closely match the Evans criteria. To accomplish this, the committee proposed a new category of manifestations that provide a “presumptive” diagnosis of NF2.
In most cases, physicians can diagnose NF2 on the basis of the consensus criteria described in Table 10–1. Diagnosis of NF2 is straightforward in individuals who have bilateral vestibular schwannomas, tumors located on the eighth cranial nerve leading from the inner ear to the brain, causing changes in balance and hearing. A diagnosis may be more challenging in two groups of people: individuals with a family history of the disorder who do not yet show manifestations, and individuals with no family history who develop one or more manifestations suggestive of the disorder but who do not yet have bilateral vestibular schwannomas. Both groups should be considered at risk for NF2 and undergo follow-up evaluations until a diagnosis can be confirmed or ruled out.
Given the complexities and rarity of NF2, if the disorder is suspected, an individual should be referred to a specialty treatment center for diagnosis, evaluation, and treatment. These centers not only have physicians and staff who are experienced in managing NF2, but also use teams of specialists to manage the disorder.
♦ Natural History of Neurofibromatosis 2
Because NF2 is so rare, few studies have been done about the development and natural progression of the disorder over the life span. Clinical experience indicates, however, that the course of NF2 varies greatly in the population but tends to be more or less the same within a given family. Although diagnosis of NF2 usually takes place in adulthood, signs of the disease may be present in childhood but are so subtle that they are missed, particularly in children without a family history of the disorder. In fact, studies of the natural history of NF2 have reported a consistent and significant delay between onset of symptoms and accurate diagnosis, emphasizing the need for better surveillance, especially for children with a family history of the disorder.
Typically, symptoms of NF2 are first noticed between 18 and 22 years of age,3,5 although one in 10 people with the disorder will become symptomatic before they are 10 years old.4(p55) In some unusual individuals symptoms first appear after 35 years of age.6 (p304) The most frequent presenting symptom is hearing loss and/or ringing in the ears (tinnitus). Less often a visit to the doctor is prompted by changes in balance sensory powers, or vision, or by limb weakness, seizures, skin tumors.3,5 In children suspected of having NF2 because of a family history of the disorder, the first manifestations may be a posterior capsular opacity or a skin schwannoma.
NF2 is a progressive disorder, but the rate of progression varies greatly, perhaps because of the influence of other genes and biological factors as yet unknown. Vestibular schwannomas generally grow slowly, but the rate of growth varies among individuals, even those within one family.7,8 Losses in balance and hearing usually develop insidiously, causing a slow deterioration over a period of years. Less often, hearing loss occurs suddenly or hearing worsens and then improves for a time. These situations are thought to occur because the tumor is compressing blood vessels.9 If vestibular schwannomas are detected early enough, it is now possible to preserve hearing in some individuals with NF2.
Most people with NF2 develop other types of tumors, yet these seldom become malignant. Because these tumors associated with NF2 originate in the brain and spinal cord, they can result in significant disability and even death. One of these tumors may cause the individual to experience a deterioration or loss of sight, have trouble walking, and be subjected to chronic pain. Some people experience such slow tumor growth that disability is minimal; others experience rapid tumor growth and loss of function. In the most severe cases—fortunately, quite rare—tumors compress the brainstem, causing death.
It is important to note several caveats, however. Because of the strong genotype-phenotype correlation in NF2, the disorder tends to manifest the same way in members of the same family. As a result the general rules may not apply; it is best for patients and physicians to use family history as a guide to what symptoms will develop, and when, in a person with NF2. Improvements in imaging and surgical techniques in the past decade have also enabled clinicians to detect tumors when they are small, sometimes even before they cause symptoms, which in many cases improves outcome.
Some studies have reported that the average life span for someone with NF2 is significantly shorter than for a person in the general population. These conclusions were largely based on old data and may not be relevant now that imaging and surgical techniques have improved. Many people with NF2 live a long time. One often-cited study3 published in 1992 found that the mean life span in people with NF2 was 62 years—meaning that half died before age 62 and half afterward. Those who died before age 62 tended to die young; the mean age at death for this group in the study was 36. Most early deaths resulted from complications related to NF2.
The same team recently conducted another analysis and probed the issue further.7 They found that these three clinical factors increased risk of early death: age at diagnosis; where treatment takes place; and presence of meningiomas, a type of brain tumor (see below). The younger a person was at time of diagnosis, the greater the risk of mortality, possibly because earlier age of onset is associated with faster tumor growth. Intracranial meningiomas may pose challenges because they require complicated surgical treatment and proper postoperative care. The authors speculate that patients with NF2 who are treated at specialty clinics are less likely to die because practice and experience are vitally important in surgery. Patients treated at such specialty centers tend to have better treatment outcomes and fewer postoperative complications.
♦ Clinical Features
A brief description of the types of tumors and other manifestations associated with NF2 is provided below. An estimated timetable of when they are most likely to occur is listed in Table 10–2. Information on management of such manifestations is provided in Chapter 11.
Vestibular Schwannomas
Tumors of the eighth cranial nerve occur in 95% of adults who have NF2 and usually develop on nerves on both sides of the head.3,5,10 Originally known as acoustic neuromas, these hallmark tumors of NF2 have since been designated “vestibular schwannomas” to reflect a better understanding of their origin and pathology.
| Childhood: |
| Schwannomas visible on skin (subtle) |
| Eye problems: |
|
| Adulthood: |
|
A vestibular schwannoma originates along the vestibular branch of the eighth cranial nerve, which helps people to maintain balance, and therefore may cause symptoms such as dizziness and stumbling. In many cases these initial symptoms escape notice. One exceedingly worrisome and potentially fatal early symptom is that a person who has NF2 may become disoriented while under water (see Chapter 11). As the tumor continues to grow, it places pressure on and sometimes engulfs the other segment of the eighth cranial nerve, the auditory branch. This causes the symptoms that most often prompt people to seek medical attention—ringing in the ears and increasing difficulty with hearing—and explains why these tumors were originally known as acoustic neuromas.
Pathologically the tumors that define NF2 are schwannomas, benign tumors that develop from the Schwann cells that help to form the protective myelin sheath around nerve cells in the central nervous system. Unlike neurofibromas in NF1, which consist of multiple cell types and sometimes infiltrate and become entwined with nerve fibers, schwannomas consist mainly of one cell type and grow within a fibrous capsule that prevents them from growing into the nerve fiber itself. Schwannomas cause symptoms once they grow large enough to compress the nerves and adjacent blood vessels.
Schwannomas Located Elsewhere
Spinal Schwannomas
These tumors are the most common type of spinal tumor seen in NF2, developing in as many as four in five people with the disorder. Most spinal schwannomas are small, do not cause symptoms, and do not require surgery.11 Spinal schwannomas that develop in the topmost (cervical) and middle (thoracic) portions of the spine may take on a dumbbell shape as they grow, making them indistinguishable in imaging scans from neurofibromas seen in NF1. Multiple small spinal schwannomas may dot the cauda equina, the bundle of nerves located at the lower end of the spinal cord. Although on imaging studies this may resemble metastatic cancer, most spinal schwannomas are benign and do not cause medical complications.
Cranial Schwannomas
One in four people with NF2 will also develop schwannomas on other cranial nerves.3,5 The fifth cranial (trigeminal) nerve is most often the site. This is the largest cranial nerve, with three branches; it conveys sensory information in the head and face, and one nerve branch helps to control the muscles used in chewing and eating. Tumors on this nerve may grow into the cavernous sinus, a cavity at the base of the skull. Tumors of the third cranial nerve (oculomotor) may cause double vision (diplopia) and lazy eye (amblyopia). When tumors attach to the lower cranial nerves they may cause difficulty in swallowing and cause fluid to enter the lung during an intake of breath (aspiration).
Peripheral Schwannomas
Although NF2 primarily produces tumors in the brain and spinal cord, schwannomas sometimes develop on peripheral nerves that emanate from the spinal cord. Tumors on the major deep nerves in the arms and legs are most likely to cause pain, weakness, and other symptoms. About half of all people with NF2 develop nodular schwannomas in the limbs and trunk that become painful after a minor trauma,10 such as banging an arm or leg.
Dermal Schwannomas
About half of people with NF2 develop these tumors on the surface of the skin,3,5,12 although they are usually so subtle that they may be missed. They form as slightly elevated areas of skin, sometimes rough in texture. Skin schwannomas cause no physical effects.
Meningiomas
Meningiomas are tumors that develop in the membrane that covers the surface of the brain and spinal cord. These tumors occur in about half of all people with NF2, more often in the brain than in the spine.3,5 In most cases, meningiomas are slow growing and may not cause symptoms for years or even decades. When symptoms do occur, they are usually caused by increased pressure within the skull. Pressure results either because the tumor has grown, or because it prevents proper drainage of cerebrospinal fluid from the ventricles, causing fluid to build up in the brain (hydrocephalus). The exact symptoms experienced depend on the tumor’s location, but generally they include headaches, nausea, vomiting, and vision complications. Depending on their location, meningiomas may cause changes in mood, personality, speech, coordination, and memory.
Astrocytomas and Ependymomas
Astrocytomas and ependymomas are both tumors that develop from the glial cells that support nerve cells in the brain and spinal cord. Astrocytomas develop from cells known as astrocytes, and usually occur in the brain. Ependymomas develop from ependymal cells that are found in the internal canal of the spinal cord and the ventricles of the brain. Astrocytomas and ependymomas occur less frequently than the other tumors associated with NF2, but it is not known exactly how often they occur. Some studies have estimated that as many as one in three people with NF2 develop such tumors,11 but only a small percentage of these cause symptoms.
As with any type of brain tumor, symptoms of astrocytomas and ependymomas may include headache, vomiting, and altered vision because of increased pressure inside the skull. Depending on the location of the tumor, there may be changes in mood, personality, speech, writing, coordination, and memory. Symptoms specific to ependymomas include neck pain, optic nerve swelling, and jerky eye movements.
♦ Eye Conditions
Vision complaints are common in people with NF2. Various studies report that some type of visual impairment is a consequence in anywhere from 33 to 75% of people with the disorder.10,13,14 Because these eye conditions tend to develop before vestibular schwannomas do, they can help establish a diagnosis early on, especially in someone with a family history of NF2.
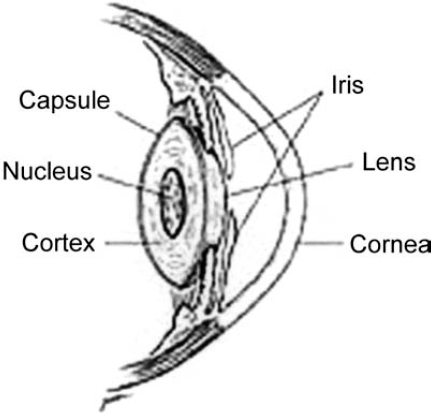
Cataracts (Fig. 10–1), cloudy areas that occur in the lens of the eye, are the most frequent ocular complication of NF2. Although cataracts occur in many people with NF2, they impair vision in only one in five individuals.6 (p306) When cataracts develop, vision may become cloudy and blurred, and the person may have difficulty dealing with bright lights or glare. Such symptoms develop because the cataract interferes with the focus of light on the retina, the part of the eye that sends visual signals to the brain. The most common types of cataract seen in NF2 are juvenile posterior subcapsular lenticular opacity, a lesion that occurs near the lens cortex and adjacent to the lens capsule, and cortical cataracts, opacities of the lens cortex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








