SECTION VII DISCUSSION OF CASES
CHAPTER 25
Discussion of Cases
As outlined in Chapter 4, the important question, “Where is the lesion?” (or “What is the precise location of the deficit?”), must be followed by the equally important question, “What is the lesion?” (or “What is the nature of the disease?”). The answers should lead to the differential diagnosis and correct diagnosis and should guide therapy.
THE LOCATION OF LESIONS
Where is the lesion?. In thinking about the location of the lesion, it is important to systematically survey the nervous system. Lesions can be located in one or more of the following anatomic sites:
 Muscles. In muscle diseases, one sees weakness, sometimes with muscle atrophy. Deep tendon reflexes are usually depressed. Diseases of muscle include the dystrophies, which have specific genetic patterns and stages of onset and may preferentially involve certain muscle groups; and inflammatory disorders of muscle such as polymyositis. Diagnosis may be aided by measuring the level of enzymes (such as creatine phosphokinase) in the serum because damage to muscle fibers may lead to their release. Electromyography and muscle biopsy may help with diagnosis.
Muscles. In muscle diseases, one sees weakness, sometimes with muscle atrophy. Deep tendon reflexes are usually depressed. Diseases of muscle include the dystrophies, which have specific genetic patterns and stages of onset and may preferentially involve certain muscle groups; and inflammatory disorders of muscle such as polymyositis. Diagnosis may be aided by measuring the level of enzymes (such as creatine phosphokinase) in the serum because damage to muscle fibers may lead to their release. Electromyography and muscle biopsy may help with diagnosis.
 Motor end-plates. Disorders of the motor end-plate include myasthenia gravis and the Lambert-Eaton myasthenic syndrome. In these disorders, there is weakness, sometimes accompanied by abnormal fatigability resulting from abnormal function (eg, decreased effect of acetylcholine [ACh] on the post junctional muscle or decreased release of ACh) at the neuromuscular junction. Weakness may involve the limbs or trunk or muscles involved in chewing, swallowing, or eye movements. In addition to the characteristic clinical pattern, electromyography may be helpful in diagnosis.
Motor end-plates. Disorders of the motor end-plate include myasthenia gravis and the Lambert-Eaton myasthenic syndrome. In these disorders, there is weakness, sometimes accompanied by abnormal fatigability resulting from abnormal function (eg, decreased effect of acetylcholine [ACh] on the post junctional muscle or decreased release of ACh) at the neuromuscular junction. Weakness may involve the limbs or trunk or muscles involved in chewing, swallowing, or eye movements. In addition to the characteristic clinical pattern, electromyography may be helpful in diagnosis.
 Peripheral nerves. Peripheral nerve lesions may be differentiated from lesions of muscle or motor end-plate by clinical criteria, electrical tests, or biopsy. In many disorders of peripheral nerves, both motor (lower motor neuron) and sensory deficits are present, although in some cases motor or sensory function is impaired in a relatively pure way. In most peripheral neuropathies, functions subserved by the longest axons are impaired first, so that there is a “stocking-and-glove” pattern of sensory loss, together with loss of distal reflexes (such as the ankle jerks) and weakness of distal musculature (ie, intrinsic muscles of the feet), which is in severe cases accompanied by muscle atrophy.
Peripheral nerves. Peripheral nerve lesions may be differentiated from lesions of muscle or motor end-plate by clinical criteria, electrical tests, or biopsy. In many disorders of peripheral nerves, both motor (lower motor neuron) and sensory deficits are present, although in some cases motor or sensory function is impaired in a relatively pure way. In most peripheral neuropathies, functions subserved by the longest axons are impaired first, so that there is a “stocking-and-glove” pattern of sensory loss, together with loss of distal reflexes (such as the ankle jerks) and weakness of distal musculature (ie, intrinsic muscles of the feet), which is in severe cases accompanied by muscle atrophy.
 Roots. A motor root lesion results in a precise segmental motor deficit, which in some cases (eg, plexus lesions) is mediated through several nerves. A single sensory deficit may be difficult to diagnose because of the adjacent overlapping dermatomes (see Fig 5–9). When a nerve root carrying axons mediating a deep tendon reflex is affected, the reflex may be depressed (see Table 5–5). Sensory root symptoms may include pain that is worsened with the Valsalva maneuver, the forced expiratory effort caused by laughing, sneezing, or coughing.
Roots. A motor root lesion results in a precise segmental motor deficit, which in some cases (eg, plexus lesions) is mediated through several nerves. A single sensory deficit may be difficult to diagnose because of the adjacent overlapping dermatomes (see Fig 5–9). When a nerve root carrying axons mediating a deep tendon reflex is affected, the reflex may be depressed (see Table 5–5). Sensory root symptoms may include pain that is worsened with the Valsalva maneuver, the forced expiratory effort caused by laughing, sneezing, or coughing.
 Spinal cord. The staggered pattern of decussation of the lateral corticospinal tract, dorsal column-medial lemniscal system, and spinothalamic tracts often permits localization of lesions within the spinal cord. Injury to the spinal cord, at a given level, may result in lower-motor-neuron signs and symptoms at that level, but will result in upper-motor-neuron abnormalities below the level of the lesion. Sensation may be impaired below the lesion; thus, the presence of a sensory level (ie, a dermatomal level below which sensation is impaired) can alert the clinician to the possibility of injury to the spinal cord. The injury may be located at the sensory level or above it.
Spinal cord. The staggered pattern of decussation of the lateral corticospinal tract, dorsal column-medial lemniscal system, and spinothalamic tracts often permits localization of lesions within the spinal cord. Injury to the spinal cord, at a given level, may result in lower-motor-neuron signs and symptoms at that level, but will result in upper-motor-neuron abnormalities below the level of the lesion. Sensation may be impaired below the lesion; thus, the presence of a sensory level (ie, a dermatomal level below which sensation is impaired) can alert the clinician to the possibility of injury to the spinal cord. The injury may be located at the sensory level or above it.
 Brain stem. Functional deficits in the long tracts that pass from the brain to the spinal cord or vice versa, together with cranial nerve signs and symptoms, suggest a lesion in the brain stem. As a result of the crowding of numerous fiber tracts and nuclei within the relatively compact brain stem, lesions at particular sites usually result in characteristic syndromes. Lesions in the medulla involve the last few cranial nerves, whereas lesions in the pons involve nerves V, VI, and VII, and lesions of the midbrain often involve nerve III and possibly nerve IV.
Brain stem. Functional deficits in the long tracts that pass from the brain to the spinal cord or vice versa, together with cranial nerve signs and symptoms, suggest a lesion in the brain stem. As a result of the crowding of numerous fiber tracts and nuclei within the relatively compact brain stem, lesions at particular sites usually result in characteristic syndromes. Lesions in the medulla involve the last few cranial nerves, whereas lesions in the pons involve nerves V, VI, and VII, and lesions of the midbrain often involve nerve III and possibly nerve IV.
 Cerebellum. Lesions in the cerebellum or its peduncles result in characteristic abnormalities of motor integration. There is usually impaired coordination and decreased muscle tone ipsilateral to a lesion in the cerebellar hemisphere.
Cerebellum. Lesions in the cerebellum or its peduncles result in characteristic abnormalities of motor integration. There is usually impaired coordination and decreased muscle tone ipsilateral to a lesion in the cerebellar hemisphere.
 Diencephalon. Hypothalamic lesions can be complex and can cause endocrinologic disturbances as well as visual abnormalities resulting from compression of neighboring optic tracts. Thalamic lesions often cause sensory dysfunction and may produce motor deficits as a result of compression of the neighboring internal capsule. Subthalamic lesions may cause abnormal movements such as hemiballismus. Epithalamic lesions are most frequently pineal region tumors, which can compress the cerebral aqueduct, thereby producing hydrocephalus.
Diencephalon. Hypothalamic lesions can be complex and can cause endocrinologic disturbances as well as visual abnormalities resulting from compression of neighboring optic tracts. Thalamic lesions often cause sensory dysfunction and may produce motor deficits as a result of compression of the neighboring internal capsule. Subthalamic lesions may cause abnormal movements such as hemiballismus. Epithalamic lesions are most frequently pineal region tumors, which can compress the cerebral aqueduct, thereby producing hydrocephalus.
 Subcortical white matter. The presence of abnormal myelin (leukodystrophy, which is more common in infants and children than in adults) or the destruction of normal myelin (which can be caused by inflammatory disorders such as multiple sclerosis) results in abnormal axonal conduction and deficits of function. Disease may be diffuse, focal, or multifocal with a parallel pattern of clinical involvement.
Subcortical white matter. The presence of abnormal myelin (leukodystrophy, which is more common in infants and children than in adults) or the destruction of normal myelin (which can be caused by inflammatory disorders such as multiple sclerosis) results in abnormal axonal conduction and deficits of function. Disease may be diffuse, focal, or multifocal with a parallel pattern of clinical involvement.
 Subcortical gray matter (basal ganglia). A variety of movement disorders, including Parkinson’s disease and Huntington’s disease, involve the basal ganglia. Tremors and other abnormal movements, abnormalities of tone (eg, cogwheel rigidity in Parkinson’s disease), and slowed movements (bradykinesia) are often seen. These disorders often affect the basal ganglia bilaterally, but if there is unilateral disease, the movement disorder will affect the contralateral limbs.
Subcortical gray matter (basal ganglia). A variety of movement disorders, including Parkinson’s disease and Huntington’s disease, involve the basal ganglia. Tremors and other abnormal movements, abnormalities of tone (eg, cogwheel rigidity in Parkinson’s disease), and slowed movements (bradykinesia) are often seen. These disorders often affect the basal ganglia bilaterally, but if there is unilateral disease, the movement disorder will affect the contralateral limbs.
 Cerebral cortex. Focal lesions may produce well-circumscribed deficits such as aphasia, hemi-inattention and neglect syndromes, or Gerstmann’s syndrome (see Chapter 21). In most patients, aphasia is due to the left hemisphere involvement. When the primary motor cortex is involved on one side, for example by a stroke or a tumor, there is usually a “crossed hemiparesis,” that is, upper-motor-neuron weakness of the contralateral limbs. Irritative lesions of the cortex may result in seizures, which can be focal or generalized.
Cerebral cortex. Focal lesions may produce well-circumscribed deficits such as aphasia, hemi-inattention and neglect syndromes, or Gerstmann’s syndrome (see Chapter 21). In most patients, aphasia is due to the left hemisphere involvement. When the primary motor cortex is involved on one side, for example by a stroke or a tumor, there is usually a “crossed hemiparesis,” that is, upper-motor-neuron weakness of the contralateral limbs. Irritative lesions of the cortex may result in seizures, which can be focal or generalized.
 Meninges. Hemorrhages in the subarachnoid, subdural, and epidural spaces have characteristic clinical and neuroradiologic features. Subarachnoid hemorrhage is often accompanied by severe headache (“worse headache of my life”). Subdural hemorrhages may occur acutely or chronically and can follow even trivial head injury, especially in elderly patients and young children. Epidural hemorrhages are often rapidly progressive and can produce sudden herniation of the brain. Infection of the subarachnoid space (meningitis) may present with signs of meningeal irritation (eg, stiff neck) as well as other neurologic deficits, and the diagnosis can often be confirmed by lumbar puncture.
Meninges. Hemorrhages in the subarachnoid, subdural, and epidural spaces have characteristic clinical and neuroradiologic features. Subarachnoid hemorrhage is often accompanied by severe headache (“worse headache of my life”). Subdural hemorrhages may occur acutely or chronically and can follow even trivial head injury, especially in elderly patients and young children. Epidural hemorrhages are often rapidly progressive and can produce sudden herniation of the brain. Infection of the subarachnoid space (meningitis) may present with signs of meningeal irritation (eg, stiff neck) as well as other neurologic deficits, and the diagnosis can often be confirmed by lumbar puncture.
 Skull, vertebral column, and associated structures. Associated structures include the intervertebral disks, ligaments, and articulations. For example, metastatic tumors involving the vertebral column can produce spinal cord compression. Trauma often involves the skull and vertebral column as well as the brain and spinal cord.
Skull, vertebral column, and associated structures. Associated structures include the intervertebral disks, ligaments, and articulations. For example, metastatic tumors involving the vertebral column can produce spinal cord compression. Trauma often involves the skull and vertebral column as well as the brain and spinal cord.
THE NATURE OF LESIONS
What is the lesion?. A variety of pathologic processes can affect the nervous system. The following is a common neuropathologic classification of disorders:
 Vascular disorders. Usually, with a sudden onset of signs and symptoms, cerebrovascular disease often occurs in the setting of hypertension. Stenosis or occlusion of the carotid artery in the neck, or of any of the arteries described in Chapter 12, may be responsible. Embolism, from ulcerated plaques in the carotid or from the heart (eg, in patients with atrial fibrillation or with endocarditis) can occlude more distal vessels such as the middle cerebral. Subarachnoid hemorrhage and intraparenchymal hemorrhage (often involving the basal ganglia, thalamus, pons, or cerebellum) occur in patients with hypertension. Subdural and epidural hemorrhages occur as a result of trauma, which can be trivial (and in many cases is not remembered) in the case of subdural hematoma.
Vascular disorders. Usually, with a sudden onset of signs and symptoms, cerebrovascular disease often occurs in the setting of hypertension. Stenosis or occlusion of the carotid artery in the neck, or of any of the arteries described in Chapter 12, may be responsible. Embolism, from ulcerated plaques in the carotid or from the heart (eg, in patients with atrial fibrillation or with endocarditis) can occlude more distal vessels such as the middle cerebral. Subarachnoid hemorrhage and intraparenchymal hemorrhage (often involving the basal ganglia, thalamus, pons, or cerebellum) occur in patients with hypertension. Subdural and epidural hemorrhages occur as a result of trauma, which can be trivial (and in many cases is not remembered) in the case of subdural hematoma.
 Trauma. As previously noted, epidural and subdural hematomas can develop as a result of head injury. In addition, penetrating injuries can directly destroy brain tissue, produce vascular lesions, or introduce infections. Injury to the spine is a common cause of paraplegia and quadriplegia.
Trauma. As previously noted, epidural and subdural hematomas can develop as a result of head injury. In addition, penetrating injuries can directly destroy brain tissue, produce vascular lesions, or introduce infections. Injury to the spine is a common cause of paraplegia and quadriplegia.
 Tumors. Primary tumors of the brain and spinal cord, as well as metastases (eg, from breast, lung, and prostate tumors) produce symptoms by direct invasion (and destruction) of neural tissue, by compression of the brain and spinal cord, or by compression of the ventricles and cerebral aqueduct, which can lead to hydrocephalus. Classically, tumors of the central nervous system produce subacutely or chronically progressive deterioration, which, in contrast to vascular disorders, progresses over weeks, months, or years. Signs of increased intracranial pressure (eg, papilledema, sixth nerve palsy) may be present, and the patient may complain of increasing headache, which is sometimes worst in the morning.
Tumors. Primary tumors of the brain and spinal cord, as well as metastases (eg, from breast, lung, and prostate tumors) produce symptoms by direct invasion (and destruction) of neural tissue, by compression of the brain and spinal cord, or by compression of the ventricles and cerebral aqueduct, which can lead to hydrocephalus. Classically, tumors of the central nervous system produce subacutely or chronically progressive deterioration, which, in contrast to vascular disorders, progresses over weeks, months, or years. Signs of increased intracranial pressure (eg, papilledema, sixth nerve palsy) may be present, and the patient may complain of increasing headache, which is sometimes worst in the morning.
 Infections and inflammations. These disorders (eg, meningitis, abscess formation, encephalitis, and granulomas) may be accompanied by fever, especially if the onset is acute. Most infections and inflammations have characteristic signs, symptoms, and causes.
Infections and inflammations. These disorders (eg, meningitis, abscess formation, encephalitis, and granulomas) may be accompanied by fever, especially if the onset is acute. Most infections and inflammations have characteristic signs, symptoms, and causes.
 Toxic, deficiency, and metabolic disorders. A variety of intoxications, vitamin deficiencies (eg, B12 deficiency), and enzyme defects leading to abnormal lipid storage in neurons are examples of this heterogeneous group of disorders. Various substances in different amounts (too much or too little) can cause selective lesions involving particular nuclei or tracts. Vitamin B12 deficiency, for example, causes degeneration of axons in the dorsal and lateral columns of the spinal cord.
Toxic, deficiency, and metabolic disorders. A variety of intoxications, vitamin deficiencies (eg, B12 deficiency), and enzyme defects leading to abnormal lipid storage in neurons are examples of this heterogeneous group of disorders. Various substances in different amounts (too much or too little) can cause selective lesions involving particular nuclei or tracts. Vitamin B12 deficiency, for example, causes degeneration of axons in the dorsal and lateral columns of the spinal cord.
 Demyelinating diseases. Multiple sclerosis is the prototype demyelinating disease. As expected for a disorder characterized by multiple lesions in the white matter, examination often provides evidence for involvement of several sites in the central nervous system. The cerebrospinal fluid (CSF) often shows characteristic abnormalities. Magnetic resonance imaging (MRI) scans are very useful in confirming the diagnosis.
Demyelinating diseases. Multiple sclerosis is the prototype demyelinating disease. As expected for a disorder characterized by multiple lesions in the white matter, examination often provides evidence for involvement of several sites in the central nervous system. The cerebrospinal fluid (CSF) often shows characteristic abnormalities. Magnetic resonance imaging (MRI) scans are very useful in confirming the diagnosis.
 Degenerative diseases. This heterogeneous group of diseases for which the cause has not yet been determined includes spinal, cerebellar, subcortical, and cortical degenerative disorders that are often characterized by specific functional deficits. Onset often occurs insidiously, so that the patient cannot determine date of the onset, and progression can continue over months or years.
Degenerative diseases. This heterogeneous group of diseases for which the cause has not yet been determined includes spinal, cerebellar, subcortical, and cortical degenerative disorders that are often characterized by specific functional deficits. Onset often occurs insidiously, so that the patient cannot determine date of the onset, and progression can continue over months or years.
 Congenital malformations and perinatal disorders.
Congenital malformations and perinatal disorders.
Exogenous factors (eg, infection or radiation of the motor cortex) or genetic and chromosomal factors can cause abnormalities of the brain or spinal cord in newborn infants. Hydrocephalus, Chiari malformation, cortical lesions, cerebral palsy, neural tumors, vascular abnormalities, and other syndromes may become apparent after birth.
 Neuromuscular disorders. This group includes muscular dystrophies, congenital myopathies, neuromuscular junction disorders, transmitter deficiencies, and nerve lesions or neuropathies (inflammation, degeneration, and demyelination).
Neuromuscular disorders. This group includes muscular dystrophies, congenital myopathies, neuromuscular junction disorders, transmitter deficiencies, and nerve lesions or neuropathies (inflammation, degeneration, and demyelination).
CASES
Case 1, Chapter 3
Abnormal, gradual tiring of the muscles for eye movement and chewing is suggestive of fatigue at the neuromuscular junction. The healthy neuromuscular junction can transmit at high frequencies so that this type of fatigue does not normally occur. The prominence of muscular fatigue suggested a diagnosis of myasthenia gravis in this patient. The absence of sensory deficits tends to confirm the diagnosis. Electromyography is a useful procedure for confirmation of the diagnosis; the muscle action potential, which provides a measure of the number of muscle cells that are contracting, decreases in size with repetitive stimulation in myasthenia gravis. In addition, antibodies to ACh receptors are often present and can provide a measure of the degree of disease activity. Injection of anticholinesterase drugs, such as neostigmine or edrophonium chloride, may reverse the fatigue and help to confirm the diagnosis. Treatment centers on the use of anticholinesterase drugs and immunosuppressants, including corticosteroids, which decrease the rate of anti-ACh receptor antibody production. In some patients, thymectomy is effective.
Comment: Myasthenia gravis often affects the extraocular and bulbar musculature. Myasthenia gravis should not be confused with the myasthenic syndrome (Lambert-Eaton syndrome), an autoimmune disease seen in the context of systemic neoplasms (especially those affecting the lung and breast). In the myasthenic syndrome, abnormal antibodies directed against presynaptic Ca2+ channels interfere with the release of ACh from the presynaptic ending at the neuromuscular junction.
Case 2, Chapter 5
Shoulder pain radiating into the arm suggests involvement at the C5 or C6 level. Recent weakness in the left extremities, abnormal reflexes in the legs, and decreased reflexes in the left arm suggest a lower-motor-neuron-type lesion close to the left C6 ventral root and an upper-motor-neuron lesion in the corticospinal tract (probably on both sides). The sensory deficits indicate a level of C6, or perhaps C7, bilaterally. The course of the disease shows a slow progression and recent deterioration, a series of events typical of an expanding mass that eventually compresses the spinal cord against the hard wall of the vertebral canal. Imaging studies showed a leftsided, intradural, extramedullary mass compressing and displacing the spinal cord at the C6-7 level.
The differential diagnosis includes a mass associated with spinal roots, meninges, and nerves; a tumor from the arachnoid (meningioma); and a nerve tumor (sometimes called a neuroma). Abscesses may form a mass, but the patient’s history does not suggest an infection.
The diagnosis in this case was a nerve root tumor of the left C6 nerve. During neurosurgery, the tumor was completely removed, and the C6 sensory root was sacrificed. Pathologic studies showed a schwannoma. The patient’s recovery was complete and uneventful; 6 months after surgery, she danced at the junior prom.
Comment: MRI is now usually used to demonstrate such root tumors (Figs 25–1 and 25–2). It is crucial to request the most appropriate imaging tests. In this case, a careful examination permitted the patient’s neurologist to predict the presence of a lesion compressing the spinal cord and to request radiologic examination of the spine.
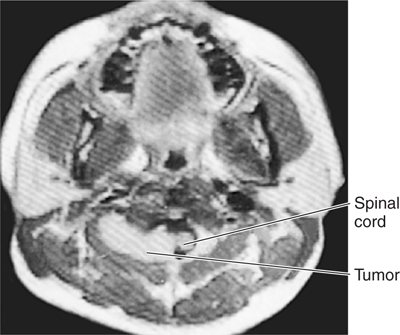
FIGURE 25–1 Magnetic resonance image of horizontal section through the neck and lower face (a different patient). The image shows a dumbbell-shaped tumor growing out of the spinal canal.

FIGURE 25–2 Magnetic resonance image (surface coil technique) of a parasagittal section through the lumbar spine in a patient with a root tumor (arrow).
Case 3, Chapter 5
Weakness, atrophy, cranial motor nerve deficits (difficulty in swallowing and in speaking), and fasciculations indicate extensive involvement of the motor system (see Chapter 23). The distribution of deficits over all the extremities suggests an extensive, generalized motor disorder. The abnormal reflexes suggest both lower- and upper-motor-neuron-type lesions. The absence of any sensory deficit strengthens a diagnosis of a pure motor disorder, and the results of the muscle biopsy confirm this.
The diagnosis is motor neuron disease, also known as amyotrophic lateral sclerosis and popularly called Lou Gehrig’s disease. Motor neurons in the spinal cord, brain stem, and motor cortex are gradually destroyed, resulting in progressive weakness. At this time the cause of motor neuron disease remains enigmatic and there is no cure (Fig 25–3).
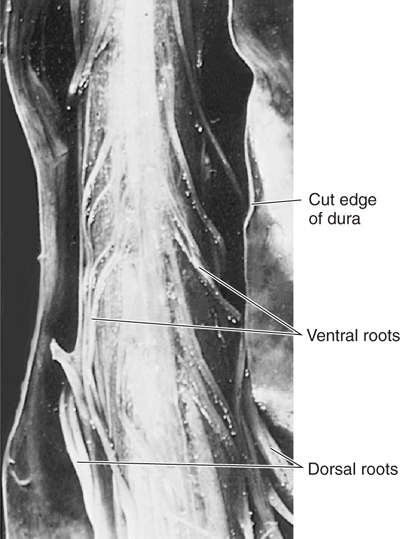
FIGURE 25–3 Ventral view of the spinal cord (with the dura opened) of a patient with motor neuron disease (amyotrophic lateral sclerosis). Notice the reduction in size of the ventral roots (resulting from the degeneration of the axons of motor neurons) compared with the normal dorsal roots.
Case 4, Chapter 6
The cause—trauma—and the location—lower cervical spine—of the lesion are clear in this case. In the acute phase, traumatic involvement of the spinal cord usually produces spinal shock with flaccid paralysis, loss of temperature control, and hypotension. Precise neurologic localization of the extent of the lesion may be difficult. Plain films of the spine or CT scanning can be used to demonstrate the location and extent of the trauma to the bony spine. MRI provides information about the spinal cord itself.
The later neurologic examination showed lesions in the left corticospinal and spinothalamic tracts. There was a left lower-motor-neuron lesion around the C7 area. The lack of sensory deficit in the C7 segment can be explained by the segmental overlapping of dermatomes. Brown-Séquard syndrome was incompletely represented in this case because the dorsal column tract on the affected side was spared (see Figs 5–24 and 5–25).
The diagnosis is a traumatic lesion of the spinal cord at C7. Neurosurgical decompression of the bone fragments prevented further damage to the spinal cord, but the functional deficits caused by local cord destruction could not be corrected.
Case 5, Chapter 6
Trauma to the lower back, followed by pain down the sciatic region, is suggestive of sciatica. One of the underlying causes is herniation of the nucleus pulposus (the soft center of the intervertebral disk), which can cause a compressive radiculopathy (ie, compression of a nearby spinal root). The aggravation of pain by coughing, sneezing, straining, and bending backward (movements that increase abdominal pressure) and the stretching of dural root sleeves by leg raising are highly suggestive of root involvement (right L5 nerve). The location is confirmed by the presence of paresthesia in the patient’s right calf as well as the loss of the Achilles tendon reflex (L5, S1). Spasm of the paravertebral muscles and tenderness along the course of the sciatic nerve are common in this disorder.
Plain radiographs are useful only for showing a decrease in the height of the intervertebral disk space. The precise location of the lesion can best be shown by CT scanning or MRI (Figs 25–4 and 25–5).
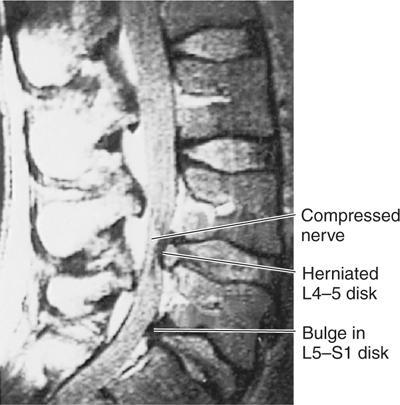
FIGURE 25–4 Magnetic resonance image (surface coil technique) of a sagittal section through the lower lumbar spine of a patient with low back pain. Note the herniation of the nucleus pulposus at L4–5 compressing the cauda equina.
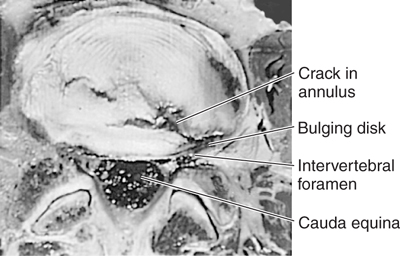
FIGURE 25–5 Photograph of a horizontal section through L4–5 intervertebral disk in a patient with low back pain. Note the lateral herniation of the nucleus pulposus. (Reproduced, with permission, from deGroot J: Correlative Neuroanatomy of Computed Tomography and Magnetic Resonance Imaging. Lea & Febiger, 21st ed. Appleton & Lange, 1991.)
The diagnosis is herniation of the nucleus pulposus at L5-S1. This patient responded well to conservative treatment (anti-inflammatory drugs, bed rest). Many patients show improvement as a result of conservative therapy. In some cases, there is a need for surgery with removal of the protruding disk fragment.
Case 6, Chapter 7
Careful analysis of the signs and symptoms shows that the following systems were involved: the vestibular system (dizziness and nystagmus); the trigeminal system, including the descending spinal tract of V (loss of pain sensation in the right half of the face); the spinothalamic system (contralateral pain deficit); the cerebellum (the inability to execute the right finger-to-nose test or to make rapid alternating movements and the presence of intention tremor and ataxia in the right lower extremity; see Appendix A); and the vagus nerve and ambiguous nucleus (hoarseness). The combination of these findings suggests a location in the posterior cranial fossa, probably in the brain stem. The combination of miosis, ptosis, enophthalmosis, and decreased sweating on one side of the face suggests Horner’s syndrome, caused by interruption of the sympathetic pathway. This pathway can be interrupted in the lateral brain stem fibers that descend from higher centers in the lateral column of the upper thoracic cord, the upper sympathetic ganglia, or the postsynaptic fibers of the carotid plexus (see Fig 20–7).
Because the patient’s disorder had a sudden onset and rapid course, a tumor was unlikely. The most frequent sudden neurologic deficits in the patient’s age group have a vascular basis: occlusion or bleeding. Of these, vascular occlusion (ischemic infarct) is the more common (see Chapter 12).
The only anatomic region where all these systems are contiguous is the lateral portion of the medulla; this is the site of the lesion: lateral medullary syndrome (Wallenberg’s syndrome). Damage to the lateral medulla results from occlusion of small branches of either the posterior inferior cerebellar or the vertebral artery. In 1895, Wallenberg described six patients with similar signs and symptoms and recognized the vascular basis of the disorder (Figs 25–6 and 25–7). Although Wallenberg’s syndrome commonly occurred as a complication of meningovascular compromise due to syphils in the preantibiotic era, this is now rare. Disease of small blood vessels due to hypertension can produce brain stem syndromes such as Wallenberg’s syndrome, and underscores the need for early recognition and textnet of high blood pressure.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








