Chapter 7 Dorsal Root Ganglion Pulsed Radiofrequency Lesioning
Conventional heat radiofrequency lesioning of the dorsal root ganglion (DRG) remains controversial owing to the potential risk of deafferentation pain. For this reason, DRG pulsed radiofrequency lesioning (PRFL), as a nondestructive neuromodulation technique, would be more attractive for chronic pain management [1–6]. Although the results of PRFL for neuropathic pain are anecdotal, the technique can be used as a potential treatment for chronic neuropathic pain [5–7]. There are two theories of the mechanisms of PRFL. One theory is that the electric field coming from the large current density of the cannula tip activates sensory fibers in the DRG and the spinal neurons to which they relay. The other theory is that temporal heat during each pulse might be responsible for the therapeutic effect [3].
Treatment objectives
The main objectives of DRG PRFL are to treat chronic segmental spinal nerve pain [1–6], segmental neuropathic pain, such as postherpetic neuralgia [8,9], and cervicogenic headache [6,10–12].
Contraindications
DRG PRFL should not be performed in patients with the following conditions:
 Coagulopathy (prothrombin time international normalized ratio value > 1.5 or platelet count < 50,000/mm3) or anticoagulant therapy
Coagulopathy (prothrombin time international normalized ratio value > 1.5 or platelet count < 50,000/mm3) or anticoagulant therapyPreoperative preparation
History Taking and Physical Examination
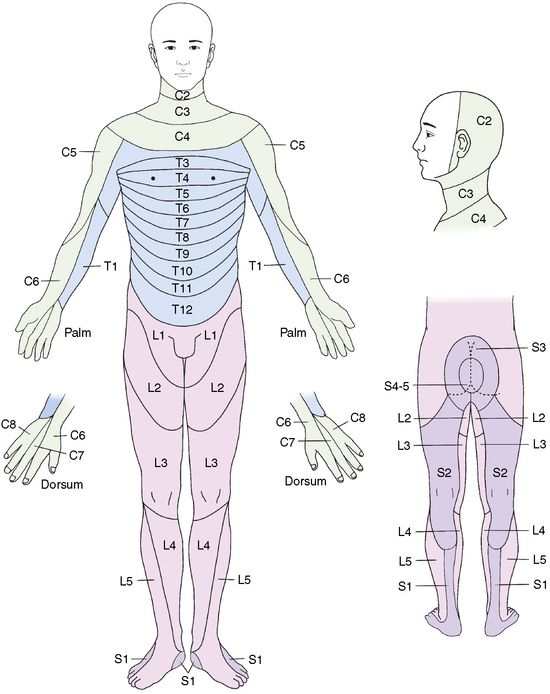
The signs and symptoms of chronic segmental pain of spine origin are as follows [4,13,18–21]:
The signs and symptoms of chronic segmental pain of non-spine origin are as follows:
 Chronic segmental pain (for longer than 3 months at a minimum) originating in areas other than the spine such as postherpetic neuralgia or postthoracotomy pain syndrome.
Chronic segmental pain (for longer than 3 months at a minimum) originating in areas other than the spine such as postherpetic neuralgia or postthoracotomy pain syndrome.The signs and symptoms of cervicogenic headache [10] are as follows:
 Headache induced by neck movements and/or sustained awkward head positioning or by external pressure
Headache induced by neck movements and/or sustained awkward head positioning or by external pressure Neck pain spreading to the ipsilateral shoulder and arm as vague; non-radicular pain appears in a third to half of patients with cervicogenic headache
Neck pain spreading to the ipsilateral shoulder and arm as vague; non-radicular pain appears in a third to half of patients with cervicogenic headacheAnatomy
Cervical Region
The anatomy of the cervical region that is relevant to DRG PRFL can be described as follows [12,21–23]:
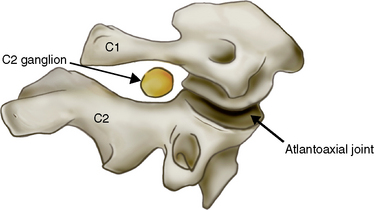
C2 Dorsal Root Ganglion (Fig. 7-2)
 The C2 ganglion is located proximal to the center of the C2 pedicle. It occupies 76% of the foramen height, a feature that may render the C2 ganglion vulnerable to entrapment.
The C2 ganglion is located proximal to the center of the C2 pedicle. It occupies 76% of the foramen height, a feature that may render the C2 ganglion vulnerable to entrapment.C3 through C8 Dorsal Root Ganglia
 The cervical neural foramen is a 4- to 5-mm-long bony canal through which the cervical nerve roots pass anterolaterally (at a 45-degree angle with respect to the coronal plane) and downward (at about a 10-degree angle with respect to the axial plane).
The cervical neural foramen is a 4- to 5-mm-long bony canal through which the cervical nerve roots pass anterolaterally (at a 45-degree angle with respect to the coronal plane) and downward (at about a 10-degree angle with respect to the axial plane). The DRG appears as a prominent oval structure in a small notch on the ventral surface of the superior facet (Figs. 6-1 to 6-4).
The DRG appears as a prominent oval structure in a small notch on the ventral surface of the superior facet (Figs. 6-1 to 6-4). The target points for DRG PRFL from C3 to C7 are posterior in the foramen, at the division between the caudal and middle thirds. The target point for C8 DRG PRFL is posterior in the foramen, at the division between the upper and lower halves (Fig. 6-5).
The target points for DRG PRFL from C3 to C7 are posterior in the foramen, at the division between the caudal and middle thirds. The target point for C8 DRG PRFL is posterior in the foramen, at the division between the upper and lower halves (Fig. 6-5). The blood supply to the DRG is often from a direct vascular branch off of the vertebral artery supplying its ventral aspect. The vertebral artery at the caudal portion of the foramen is immediately anterior and medial to the ganglion (Figs. 6-1 and 6-3).
The blood supply to the DRG is often from a direct vascular branch off of the vertebral artery supplying its ventral aspect. The vertebral artery at the caudal portion of the foramen is immediately anterior and medial to the ganglion (Figs. 6-1 and 6-3). In practice, the target points (red open circles on Fig. 6-5) should lie directly over the dorsal part of the neural foramen so as to avoid vertebral artery injury.
In practice, the target points (red open circles on Fig. 6-5) should lie directly over the dorsal part of the neural foramen so as to avoid vertebral artery injury.Thoracic Region
Most of the thoracic DRGs are located in the mid-cranial portions of the intervertebral foramina. Although the lateral margins of the thoracic DRGs are located in the extraforaminal portion, the medial margins of the DRGs are found in various locations (Table 7.1 and Fig. 7-3) [24,25].
Table 7.1 Localization of Boundaries of Dorsal Root Ganglia in the Intervertebral Foramina
| Direction | Localization | |
|---|---|---|
| Anteroposterior | DRG Anterior | DRG Posterior |
| Anterior 1/3 | 5 (11%) | — |
| Middle 1/3 | 41 (89%) | 4 (9%) |
| Posterior 1/3 | — | 42 (91%) |
| Posterior wall | — | — |
| Total | 46 (100%) | 46 (100%) |
| Mediolateral | DRG Medial | DRG Lateral |
| Foraminal | 27 (59%) | 3 (7%) |
| Extraforaminal | 19 (41%) | 43 (93%) |
| Total | 46 (100%) | 46 (100%) |
| Craniocaudal | DRG Cranial | DRG Caudal |
| Cranial 1/3 | 42 (91%) | 10 (22%) |
| Middle 1/3 | 4 (9%) | 31 (67%) |
| Caudal 1/3 | — | 5 (11%) |
| Total | 46 (100%) | 46 (100%) |
DRG, dorsal root ganglion.
From Stolker RJ, Vervest AC, Ramos LM, et al: Electrode positioning in thoracic percutaneous partial rhizotomy: An anatomical study. Pain 1994;57:241-251.
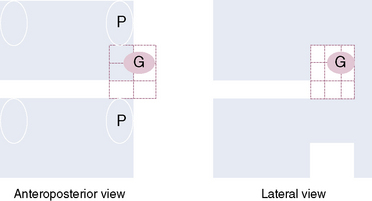
Figure 7–3 Typical location of the thoracic dorsal root ganglion (DRG; labeled G on the figure). Note that the most frequent anteroposterior location of the DRG is from the middle to the posterior third, the most frequent mediolateral location of the DRG is from foraminal to extraforaminal, and the most frequent craniocaudal location of the DRG is from the cranial to the middle third. (See also Table 7.1.) P, pedicle.
The anatomy of the upper thoracic levels (T1-T8)—the shape of the lamina, and the narrow space between the rib and wide base of the transverse process—obstructs the passage of the cannula. This makes accurate positioning of a straight cannula for the DRG procedure impossible. However, use of a 2.5-cm curved needle (Fig. 7-4) makes obtaining an accurate positioning of the cannula possible [22]. Turning the curved needle without slightly withdrawing the needle may cause tissue trauma from rotation of the curved needle-tip. To change its direction, the needle should be turned while being withdrawn slightly and then advanced.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree