Drug Treatment and Psychiatry
The use of drugs in psychiatry
Many of the original 20th-century drug treatments for psychiatric disorders, including attention-deficit hyperactivity disorder (ADHD), schizophrenia, depression, and bipolar mood disorder, were based on serendipitous findings. In the 21st century, we are able to develop psychiatric drugs in a more logical manner, on the basis of our preclinical or scientific under-standing of these and other disorders from fields as diverse as molecular genetics, lipid neuroscience, and neurospectroscopy.
While this book concentrates on the major types of drug treatment in psychiatry, it should be borne in mind that psychopharmacological inter-ventions constitute just one part of the treatment regimen that is appropriate for most disorders. Other treatments that should be considered, and with which drug treatment can be properly integrated, may include cognitive-behavioural therapy, psychodynamic psychotherapy, group psychotherapy, family therapy, marital therapy, sex therapy, art therapy, music therapy, occupational therapy, psychoeducation, social skills training, rehabilitation, phototherapy, and nutritional supplementation.
When drug therapy is opted for, due regard should be given to the underlying principles of psychopharmacology. These are summarized in Chapter 2.
The nature of psychiatric disorders
In general, most psychiatric disorders can be dichotomized into organic disorders, which are secondary to physical causes, and functional disorders. Clearly, since modern neuroscience does not believe in a mind-body (or mind-brain) duality, there is a sense in which materialist scientists should expect that all functional psychiatric disorders will eventually be discovered to be organic. For now, we may consider the major organic psychiatric disorders to consist of:
The organic disorders proper, including:
mental disorders caused by a medical condition (such as an endocrinopathy or carcinoma)
dementias
organic amnesic syndrome not induced by alcohol or another psychoactive substance
delirium.
Mental and behavioural disorders caused by psychoactive substance use, such as:
alcohol
opioids
amphetamine (amfetamine) or amphetamine-like substances
cannabinoids
sedatives or hypnotics
cocaine
other stimulants such as caffeine
hallucinogens
tobacco or nicotine
volatile solvents.
The functional psychiatric disorders are traditionally divided into:
Psychoses, such as:
schizophrenia
mood (affective) disorders
schizoaffective (schizo-mood) disorders
delusional disorders.
Neuroses, such as:
phobic anxiety disorders
other anxiety disorders
obsessive-compulsive disorder
adjustment disorders
dissociative (conversion) disorders
somatoform disorders.
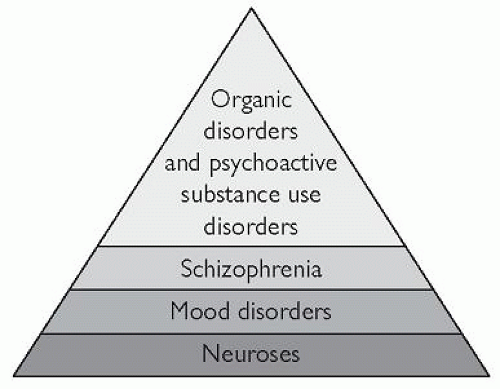
The diagnostic hierarchical model in psychiatry
Fig. 1.1 is a representation of the hierarchical model used in psychiatric diagnosis. When making a diagnosis, the disorder at the higher or highest level takes precedence. For instance, if a patient suffering from chronic schizophrenia suffers from depressive symptoms, the primary diagnosis made is schizophrenia rather than a mood (affective) disorder.
The need for a full assessment
When treating psychiatric disorders, it is important to take a full history, carry out detailed mental state and physical examinations, and perform appropriate investigations. One reason for doing this is to ensure that your working diagnosis is accurate, so that you use the most appropriate treatment. The processes of history taking, mental state examination, physical examination, and investigations also can reveal key pieces of information that can be important when prescribing medication.
History
In the psychiatric history, the family history may reveal the possibility that the patient may be suffering from an inherited disease, such as an inherited liver disease (e.g. haemochromatosis and alpha-1 anti-trypsin deficiency), which in turn might be a contraindication for the drug of first choice. Another example relates to the inherited cytochrome P450 (CYP) 2C9 (CYP2C9) polymorphisms; genes encoding for R144C (*2) and I359L (*3) amino acid substitutions have relatively high population frequencies and may lead to pharmacokinetic effects. Pharmacogenetics-based dose adjustments may have to be made for certain drugs that are metabolized by the affected organ or enzyme isoform.
The occupational history may reveal that the patient operates machinery or has to drive for a living. It may be inadvisable to perform these activities while on certain types of medication, such as tricyclic antidepressants.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree