Chapter 178 Electrodiagnostic Studies
Key Anatomy for Electrodiagnosis
An understanding of key aspects of peripheral nervous system (PNS) anatomy is required for planning and interpreting the results of an EDX study. The motor division of the PNS begins at the anterior horn cell within the spinal cord, whose axon projects outward into the ventral root. The sensory division begins distally along the dorsal root at the dorsal root ganglion, which is typically found within the ostium of the intervertebral foramen.1 Thus, the dorsal (sensory) roots within the spinal canal are preganglionic. For this reason a lesion within the intraspinal canal (e.g., compression by an intervertebral disc) may damage the sensory fibers and cause clinical sensory symptoms, but the postganglionic fibers remain intact and unaffected for the purposes of sensory NCSs. By contrast, an intraspinal canal injury causing ventral (motor) root axon loss is postganglionic, and thus loss of sufficient motor fibers is measurable by motor NCSs and NEEs. This arrangement is of considerable value in localizing intraspinal canal injury electrodiagnostically.
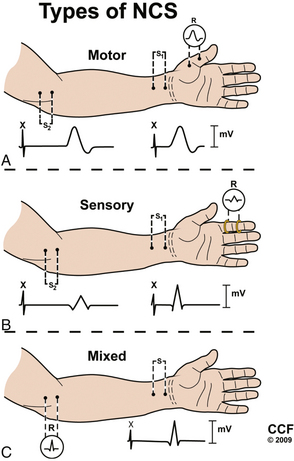
The dorsal and ventral roots merge segmentally to form mixed spinal nerves, including 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal.2 Once the spinal nerves emerge from the intervertebral foramen, they divide into the posterior primary rami, which supply the skin and intrinsic muscles of the posterior neck and back (including the paraspinal muscles) and the anterior primary rami. The anterior primary rami supply the brachial plexus and peripheral nerves of the arm at the cervical segment (Fig. 178-1), the anterolateral aspect of the trunk and the thoracic level, and the lumbosacral plexus and nerves of the leg at the lumbosacral level. Muscles supplied by a given spinal segment are referred to as a myotome, and sensory regions supplied by each spinal segment are referred to as dermatomes.
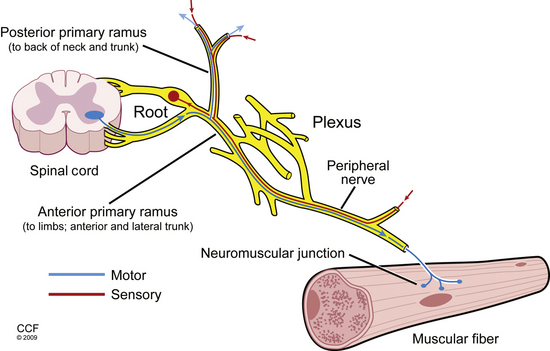
FIGURE 178-1 Basic anatomy of the peripheral nervous system.
(Illustration by David Schumick, BS, CMI. Reprinted with the permission of the Cleveland Clinic Center for Medical Art & Photography © 2009. All rights reserved.)
The motor unit is the basic functional element of the motor PNS. It consists of the anterior horn cell, its axon, and all of the muscle fibers it innervates via neuromuscular junctions. The number of muscles fibers innervated by one motor neuron varies (e.g., 10:1 in the extraocular muscles and 2000:1 in the gastrocnemius muscle) and depends on the degree of fine-motor control required. Muscle is organized into fascicles, with the fibers of a single motor unit distributed randomly over as many as 100 different fascicles. Thus, a skeletal muscle consists of a mosaic fiber from 20 to 50 overlapping motor units.3 Analysis of the electrical activity of the motor units and their muscle fibers is the objective of the NEE.
Nerve Fiber Injury Types and Relevance
The EDX examination tests large myelinated nerve fibers, which can be subject to a range of injury. Regardless of whether nerve fibers are compressed, stretched, mechanically deformed, or lacerated, the damage manifests as either axon loss or demyelination, or a combination of the two. Axon loss produces conduction failure along the affected fibers. Of note, for several days after a focal axon loss lesion (2–3 days for motor fibers and 5–6 days for sensory fibers), the nerve fibers distal to the lesion can conduct an action potential when tested by NCSs, after which wallerian degeneration ultimately results in failure of the entire axon segment distal to the lesion site (5–7 days for motor fibers and 10–11 days for sensory fibers).4 In contrast, focal demyelination remains restricted to the injury site and only affects the largest myelinated nerve fibers, including motor fibers, and sensory fibers mediating vibration and proprioception. Focal demyelinating conduction block thus can only be demonstrated with NCS by stimulation proximal to the area of injury.5
When nerves are injured, the type and degree of axon loss or demyelination affects prognosis. Clinically useful scales rating the degree of nerve injury have been developed by Seddon6 and Sunderland.7 Seddon divides focal nerve injuries into three broad categories by severity: neurapraxia, axonotmesis, and neurotmesis. Neurapraxia, the mildest injury type with the best prognosis, is transient and does not involve loss of nerve continuity. Underlying pathophysiology may include functional conduction block (without demyelination), mild demyelinating lesions, and demyelinating conduction block. Axonotmesis occurs when the nerve axon and myelin sheath are completely interrupted, while the surrounding endoneurium, perineurium, and epineurium remain intact. Prognosis in axonotmesis is better than in neurotmesis (loss of the axon and severance of its supporting connective tissue). Axon regeneration in neurotmesis is limited due to disruption of the conduit through which regenerating axons might extend to reinnervate their target organ. Sunderland’s classification system further divides these injury types, particularly with respect to the degree of supporting structure damage in neurotmesis. EDX testing can differentiate between neurapraxia and axonotmesis, providing useful prognostic information. However, axonotmesis and neurotmesis cannot be differentiated, because they appear identical electrodiagnostically.3
Components of the Electrodiagnostic Examination
Nerve Conduction Studies
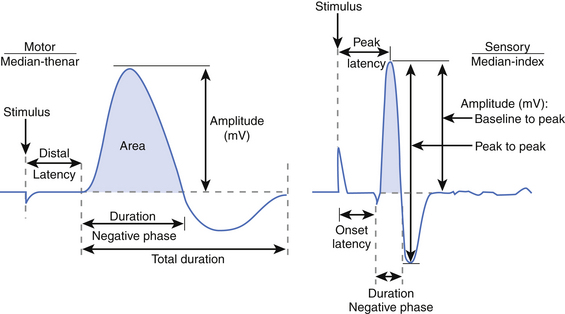
NCSs can be divided into motor, sensory, and mixed studies (Fig. 178-2). Motor and sensory NCSs are considered part of a routine EDX evaluation, whereas mixed studies are typically used only in special situations (e.g., median, ulnar, or tibial nerve entrapment). Although both surface and needle electrodes can be used for stimulating and recording, most EDX laboratories select noninvasive surface electrodes for NCSs.
Motor Conduction Studies
Motor NCSs are typically performed using an “active” recording electrode over the center of a muscle belly and reference electrode distally over the tendon of the muscle (“the belly-tendon montage”). A two-pronged (anode-cathode) stimulator is placed over the nerve supplying the muscle, with the cathode oriented closer to the recording electrode. Current is applied over the nerve to induce an action potential in the underlying nerve fibers. As the current is gradually increased with each subsequent stimulation, action potentials are triggered in more nerve fibers, and in turn more muscle fiber action potentials are generated and recorded distally as a single compound muscle action potential (CMAP). When increases in amperage no longer augment the size of the CMAP (i.e., all axons within the nerve are being stimulated), one final increase in current by 20% is performed to achieve a “supramaximal stimulation,” and the resulting CMAP is recorded for analysis.8
Several key aspects of the CMAP waveform are analyzed (Fig. 178-3). First, the distal latency is measured in milliseconds from the stimulus artifact to the initial baseline deflection. This measurement combines the action potential travel time from the stimulus site to the neuromuscular junction (NMJ), time across the NMJ, and time required for the muscle fibers to depolarize. Note that this measurement only reflects the fastest conducting fibers (i.e., those that reach the recording electrode earliest and produce the initial baseline deflection). Second, the duration of the negative phase is assessed as a measure of muscle fiber discharge synchrony in response to the stimulus. Demyelinating lesions not severe enough to cause conduction block may slow motor fiber conduction to varying degrees within a stimulated nerve, resulting in dyssynchrony or “temporal dispersion,” increasing the CMAP duration. Third, the amplitude and area of the negative phase are measured, providing an index of the number of muscle fibers depolarizing within the range of the recording electrode. Although a reduction in CMAP amplitude (and area) is most often attributed to axon loss, demyelinating conduction block between the stimulus and recording site has the same effect.
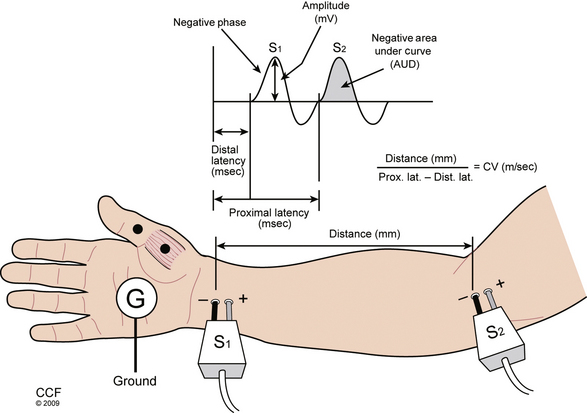
Further analysis of motor nerve conduction requires a second, more proximal stimulus over the nerve recording at the same location, using the technique just described. The more proximal stimulation is performed at a measured distance from the first. The difference between the proximal latency (PL) and distal latency (DL) in milliseconds reflects the conduction time along the fastest nerve fibers between the sites, eliminating the travel time from the distal site and across the NMJ, as well as muscle fiber depolarization time. The distance between the sites in millimeters divided by the nerve conduction time (i.e., PL minus DL) is known as the conduction velocity (Fig. 178-4). The configuration of the CMAP generated by the proximal stimulation is also compared with that of the distal CMAP. Assuming supramaximal stimulus at both sites, the CMAPs should be essentially identical. A proximal stimulation CMAP amplitude less than 50% of the distal CMAP amplitude is consistent with conduction block, or a very early focal axon loss lesion in which wallerian degeneration has not yet occurred.
In most electrodiagnostic laboratories, routine motor NCSs of the arm include median nerve (recording the abductor pollicis brevis muscle) and ulnar nerve (recording the abductor digiti minimi muscle), and in the leg, the tibial nerve (recording the abductor hallucis muscle) and peroneal nerve (recording the extensor digitorum brevis muscle). Proximal stimulation sites can be added to address specific clinical questions (e.g., stimulating the ulnar nerve above and below the elbow, or common peroneal nerve above and below the fibular head to assess for evidence of demyelination). In many cases these routine studies must be supplemented to adequately assess an area of potential injury. In the arm, motor studies of the radial nerve (recording the brachioradialis, extensor digitorum communis, or extensor indicis proprius muscles), ulnar nerve (recording the first dorsal interosseous muscle), musculocutaneous nerve (recording the biceps muscle), or axillary nerve (recording the deltoid muscle) may be indicated.5
Sensory Conduction Studies
Sensory NCSs are performed with the two-pronged stimulator and pair of recording electrodes over the nerve. These studies may performed antidromically (stimulating proximally and recording adjacent to the sensory receptor) or orthodromically (stimulating distally and recording proximally). These responses are relatively small and are measured in microvolts (μV, 1/1000 of the unit used to measure a CMAP). As with motor NCSs, current is applied over the nerve to induce an action potential and is gradually increased with subsequent stimulations. At supramaximal stimulation, the combined action potentials of the sensory fibers are recorded as a sensory nerve action potential (SNAP). SNAP latency, duration, and amplitude are measured. Latency is measured to onset (representing the conduction of the fastest fibers) or, more commonly, to the peak of the negative deflection (see Fig. 178-3).8
Particular advantages of NCSs compared with the NEEs include the ability to perform these studies with minimal patient cooperation (e.g., patients under anesthesia), provide key localizing information with regard to the sensory nerve fibers, and superior potential for identifying demyelinating lesions. It is, however, important to appreciate that NCSs only assess the large myelinated nerve fibers of the PNS, and thus disorders affecting only the smallest nerve fibers (e.g., small sensory fiber peripheral polyneuropathies) will not be demonstrated. NCSs are also relatively insensitive to motor axon loss compared with NEEs, underscoring the complementary nature of NCSs and NEEs.5
Needle Electrode Examination
Next, the examiner assesses for spontaneous electrical activity with the needle electrode at rest within the muscle. Normal muscle should be electrically silent during this phase. Fibrillation potentials are an important electrophysiologic marker of denervation. This form of spontaneous activity is characterized by regularly firing potentials, most commonly of a brief sharp spike configuration, derived from a single denervated muscle fiber. Larger-amplitude potentials are observed in acute disease9 and are present in greater density in more severe disorders. Fibrillation potentials are sensitive to denervation because disruption of a single motor axon results in fibrillation of all muscle fibers within that motor unit. They can thus be seen when motor axon loss is insufficient to cause clinical weakness. Although these potentials are most commonly associated with injury to motor axons, they may also be found in inflammatory myopathies and rarely in other neuromuscular disorders. Importantly, in the setting of denervation, fibrillation potentials require an average of 21 days to appear after injury and persist until reinnervation occurs or the muscle fibers degenerate at around 18 to 24 months after axon loss.10
Other forms of spontaneous activity can be observed during the resting phase. Fasciculation potentials, which are irregularly firing spontaneous discharges of an entire motor unit, are a marker of nerve fiber irritation as opposed to denervation. Complex repetitive discharges, which are recurrent, cyclic discharges of a series of muscle fibers, are a marker of chronicity, typically seen in neurogenic or myopathic disorders of at least 6 months’ duration.3
During the activation phase of the NEE, the muscle is contracted in order to analyze the firing pattern and morphology of voluntarily generated motor unit action potentials (MUAPs). A MUAP represents the summed electrical activity produced by depolarization of the muscle fibers of a single motor unit within the range of the recording electrode. The force generated by a muscle is a function of the number of different MUAPs firing and the rate at which they fire. At minimal contraction, a single MUAP may be observed firing in a semirhythmic pattern at a basal rate of approximately 5 to10 Hz. As the patient is asked to gradually contract the muscle with greater force, a second MUAP is “recruited,” and the firing rates of both MUAPs are increased until a third MUAP is recruited, and so on. A normal ratio of firing frequency to the number of different MUAPs firing is approximately 5:1 (e.g., when the MUAP firing rate reaches 20 Hz, four different MUAPs should be identifiable).8 At maximal contraction, MUAPs overlap and create an interference pattern, in which no single motor unit can be distinguished.
Finally, the morphology of the MUAPs is analyzed. In partial or gradual axon loss disorders, chronic neurogenic changes in the MUAP configuration can be appreciated after a period of 4 to 6 months. These changes occur due to collateral sprouting of the surviving motor axons, resulting in a greater number of muscle fibers belonging to each remaining motor unit. As more adjacent muscle fibers join the motor unit, the MUAP increases in duration and amplitude and appears more complex (polyphasic). Once present, these changes persist indefinitely and may be the sole evidence of a remote neurogenic injury.3
Late Responses
H Reflex
The H response amplitude and latency can be compared contralaterally and to values in normal controls adjusted for age and height, providing evidence of nerve fiber injury within the S1 reflex arc. Although H reflex abnormalities are considered sensitive for root impingement caused by S1 radiculopathy, the finding lacks specificity, also being found in patients with polyneuropathy, proximal tibial or sciatic mononeuropathies, and lumbosacral plexopathy. Absent H reflexes are also commonly observed in patients older than age 65 and in patients with a history of lumbar laminectomy and are thus of unclear clinical significance in this context.11 Overall, the usefulness of an absent H reflex is limited when the remainder of the EDX examination is within normal limits.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree