A motor unit is shown with a recording electrode in proximity. Individual muscle fiber potentials are recorded in sum as the motor unit action potential (MUAP)
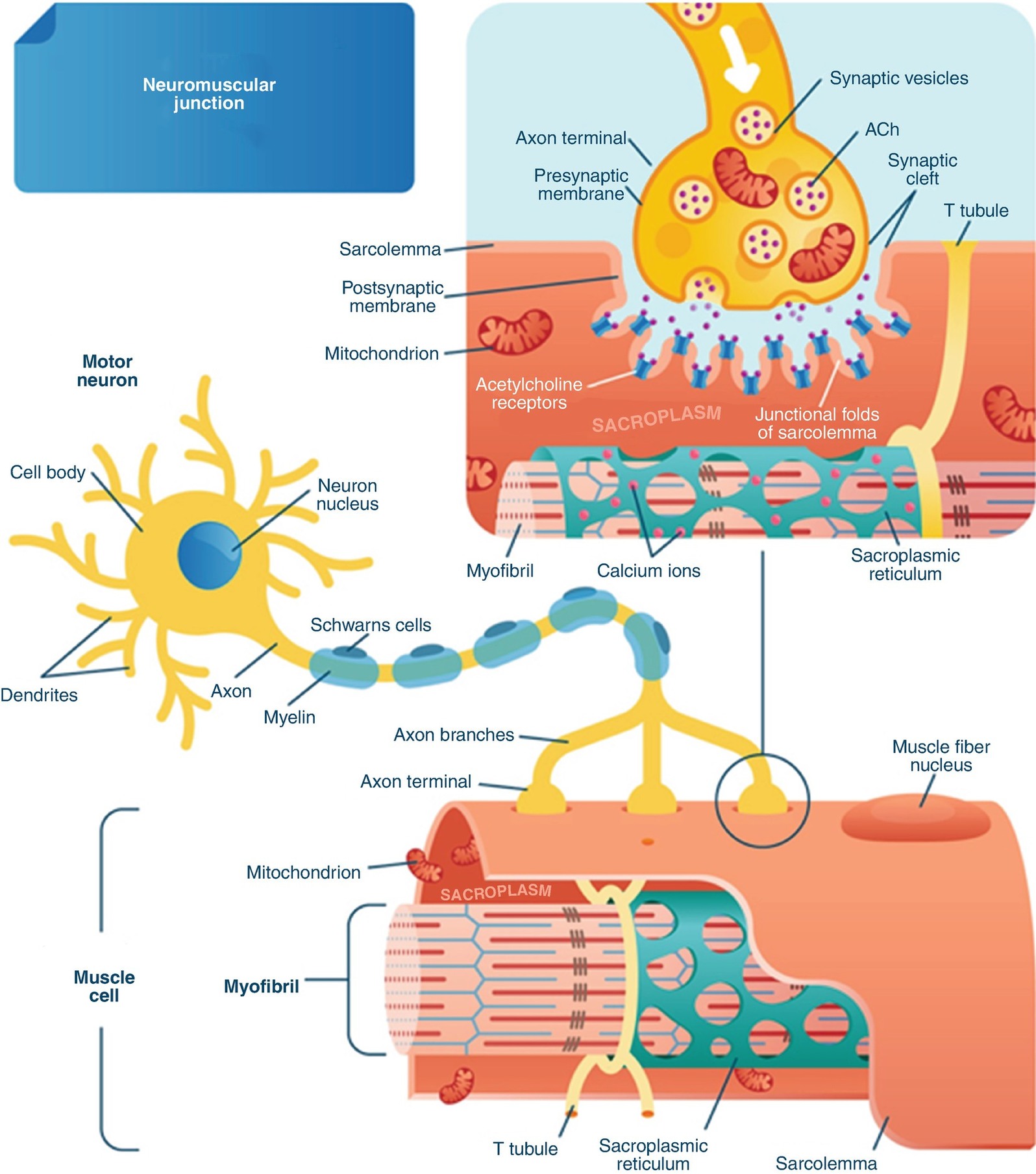
The neuromuscular junction. (1) Action potential travels down from the axon to the endplate. (2) Calcium enters the endplate. (3) Acetylcholine is released. (4) Acetylcholine travels down the synaptic cleft. (5) Acetylcholine attaches to ligand-gated receptor. (6–7) © VectorMine|Dreamstime.com
Muscles used for nerve root monitoring by region
Region | Nerve root | Muscle monitored |
|---|---|---|
| C3 | Trapezius |
C4 | Trapezius | |
C5 | Deltoid | |
C6 | Biceps | |
C7 | Triceps | |
C8/T1 | Abductor pollicis brevis/flexor carpi ulnaris | |
| T2–6 | Intercostals |
T7–9 | Upper rectus abdominis | |
T10–12 | Lower rectus abdominis | |
| L1 | Sartorius, iliopsoas |
L2 | Rectus femoris, vastus lateralis | |
L3 | Rectus femoris, vastus lateralis | |
L4 | Tibialis anterior, rectus femoris | |
L5 | Tibialis anterior, biceps femoris | |
| S1 | Gastrocnemius, biceps femoris |
S2 | Gastrocnemius | |
S3 | Anal sphincter | |
S4 | Anal sphincter |
Recording parameters for EMG monitoring
Bandwidth | Sensitivity | Time base |
|---|---|---|
5 Hz–5 kHz | 50–100 mV | 50 ms |
Spontaneous EMG
Spontaneous EMG (s-EMG) is used as a means of monitoring cranial and spinal nerves during surgery. The premise is that impending injury to these structures by stretch, compression, or other forms of mechanical irritation will cause them to increase firing which is detectable as CMAPs in the monitored muscle groups [9–13]. Rare firing may occur from heat/cold exposure, while ischemia usually does not induce action potential firing and thus is poorly detected by EMG. Proper selection of muscles to monitor is key to the success of S-EMG monitoring (see Table 8.1).
Many of the cranial nerves that are routinely monitored with EMG have sensory or autonomic components in addition to the monitorable motor component. In these cases, EMG is used as a sentinel for function of the entire nerve, even if the motor component is the smallest functional component of the nerve. If the motor division of the cranial nerve includes branches, it is appropriate to monitor the muscles innervated by each branch whenever possible (review Table 2.1 in Chap. 2).
Spinal nerves are mixed (sensory and motor) nerves that may be monitored for irritation with spontaneous EMG [9, 11, 13]. Spontaneous EMG monitoring differs from other intraoperative neuromuscular monitoring modalities in that the expected or normal state is the lack of response due to the absence of any muscle activity [11]. This indicates that a normal healthy nerve has not become activated as a result of surgical stimulation. Hence, reporting s-EMG to the surgeon is considered a neurological event or change.
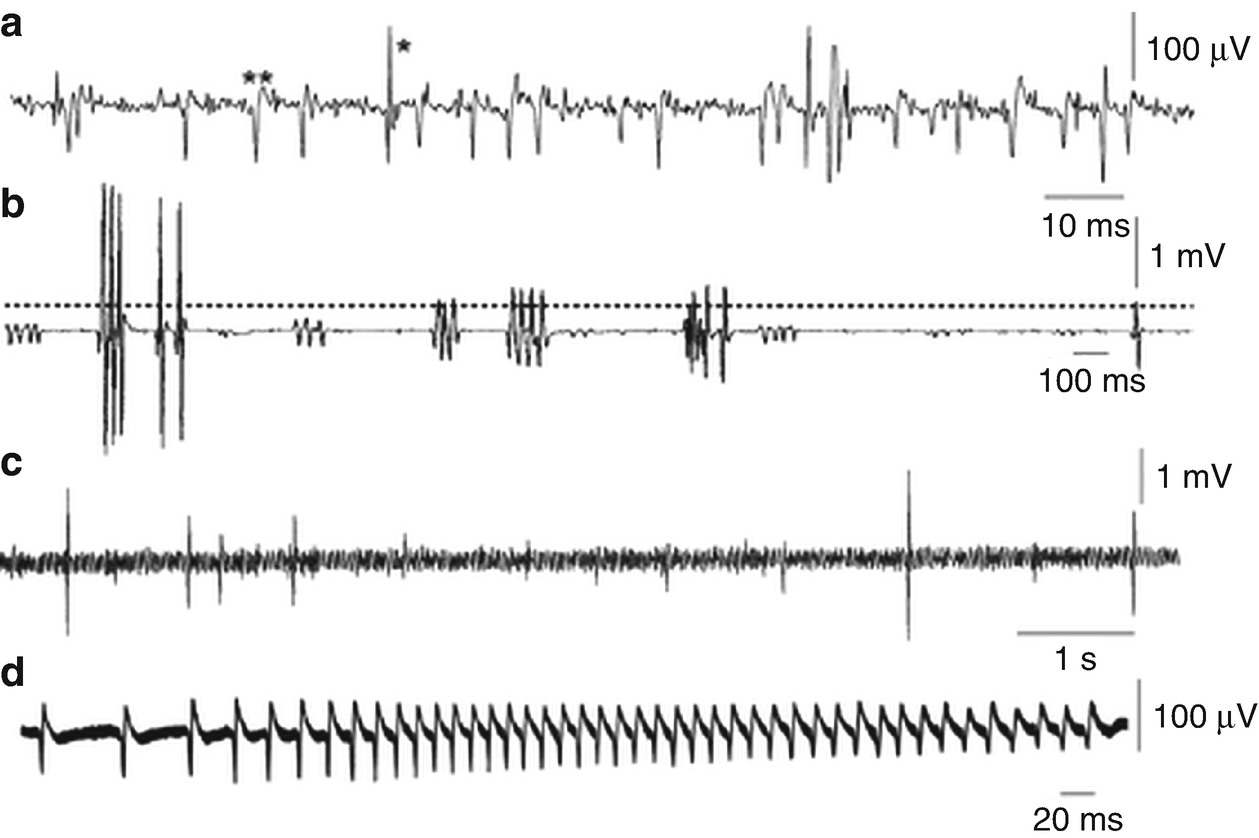
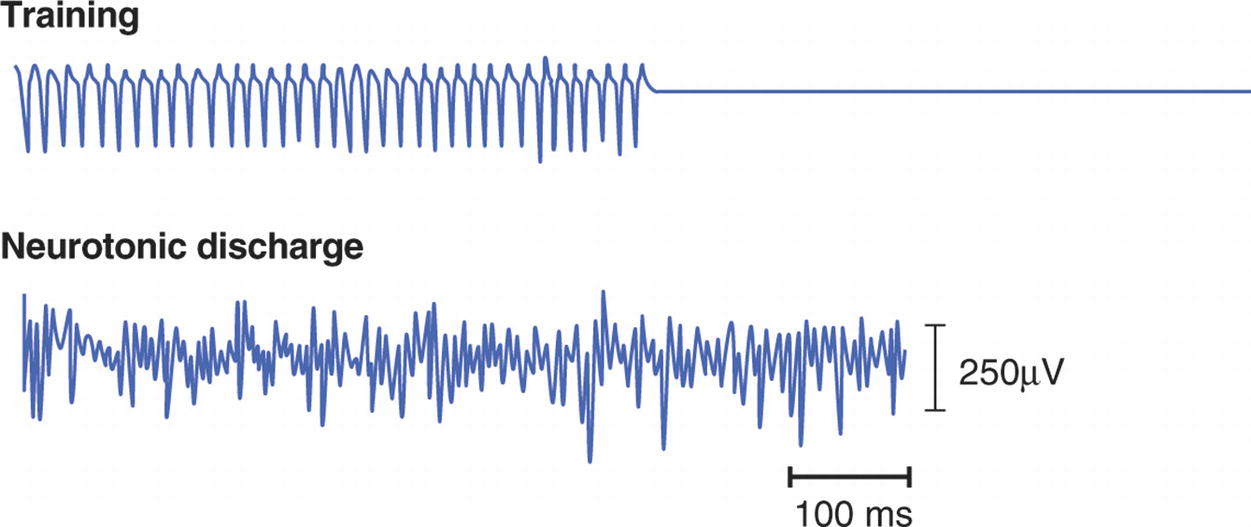
Abnormal spontaneous activity . (A) Fibrillations (∗) and positive sharp waves (∗∗) in an acutely denervated hand muscle. (B) Single, doublet, triplet, and multiplet motor unit neuromyotonic discharges. Bursts of discharge are irregular in frequency and the intra-burst frequency of discharge is up to 200 Hz. (C) Fasciculations in the tongue in a patient with amyotrophic lateral sclerosis. The single discharges are irregular and occur on a background of ongoing EMG activity caused by poor relaxation. (D) Myotonic discharges in a patient with dystrophia myotonica . There is a characteristic waxing and waning in frequency. (Reproduced from Journal of Neurology, Neurosurgery & Psychiatry, Mills K, 76, ii32–ii35, Copyright 2005, with permission from BMJ Publishing Group Ltd)
The clinical significance of the EMG firing pattern can be generally considered proportional to the frequency, amplitude , and persistence of the firing. Waveforms occurring at high frequency and amplitude indicate multiple motor units involved and a higher likelihood that the firing pattern is a warning of an impending injury. The correlation of EMG activity with a surgical event (such as retractor placement or hardware insertion) suggests a causative event, and reversal or cessation of the event should result in a return to the baseline EMG pattern. Persistence of EMG firing beyond cessation of the causative event is worrisome and suggests that injury to the nerve may have already occurred.
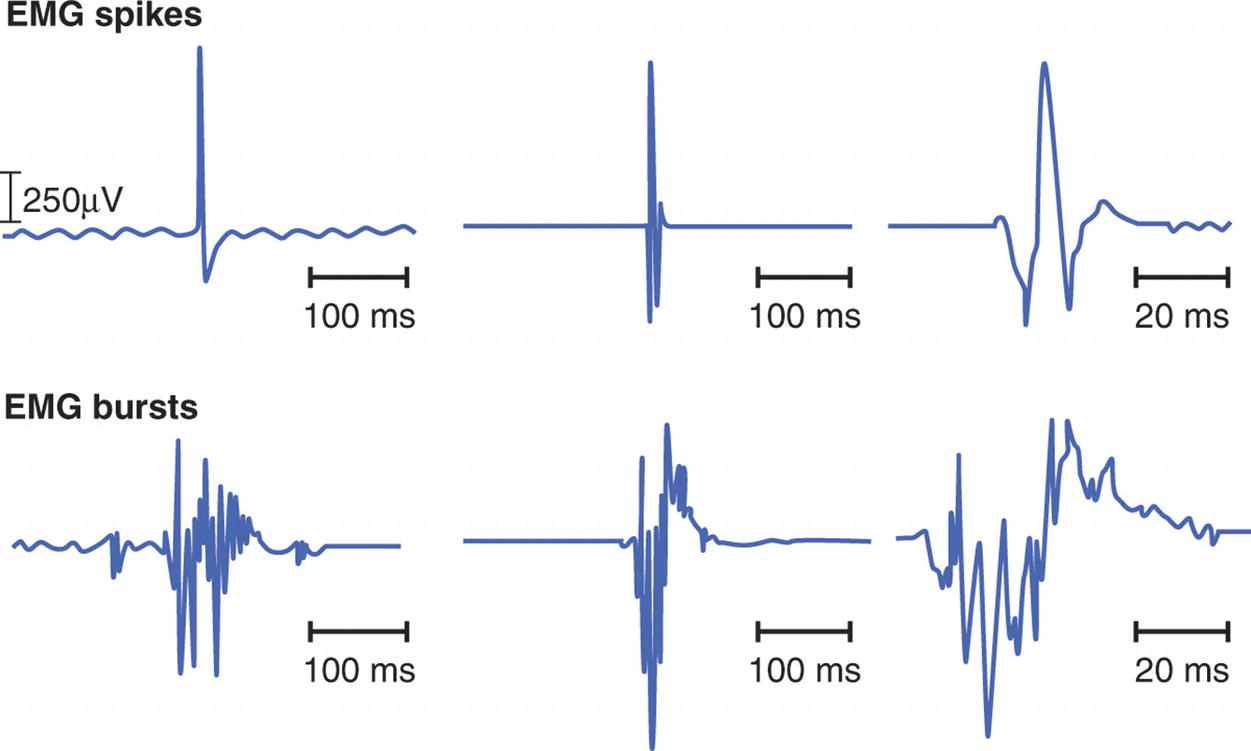
An example of EMG spikes (upper panels) and bursts (lower panels)

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree











