| 157 | Encephaloduroarteriosynangiosis |
♦ Preoperative
- Preoperative management of moyamoya patients is critical to success of the surgery.
- Strategy is based on the utilization of appropriate imaging and the maintenance of hypervolemia, normocarbia, and prevention of thrombosis.
Imaging
- Full diagnostic angiogram is critical to the planning of the procedure, including imaging of the external carotid circulation for:
- Identification of transdural collaterals so that they may be preserved during surgery.
- Confirmation of the presence of a suitable donor scalp vessel (usually the parietal branch of the superficial temporal artery [STA]).
- Identification of transdural collaterals so that they may be preserved during surgery.
- Dehydration is a significant risk given the hyoperfused intracranial circulation.
- Admission to the hospital on the evening prior to surgery is performed for intravenous hydration.
- Isotonic fluids are run at 1.5 times maintenance rate.
Preoperative Medication
- Barring medical contraindication, patients are treated with daily aspirin therapy from the time of their diagnosis of moyamoya.
- Dosing is continued up to and including the day prior to surgery.
♦ Special Considerations
- Sickle cell patients must undergo exchange transfusions within 1 week prior to surgery (or as indicated by their hematology team).
- Pain and anxiety must be aggressively managed, especially with children, since hyperventilation (as occurs with crying) can induce cerebral vasoconstriction, leading to stroke.
Special Equipment
- Electroencephalogram (EEG) is employed during surgery to identify focal slowing, indicative of compromised cerebral blood flow, so that immediate compensatory measures can be instituted by the operative team. Hand-held “pencil” Doppler probes are necessary for mapping the STA.
- Intraoperative microscope
- Microdissection instruments (including jeweler’s forceps, microtying instruments, Vannas ophthalmic scissors, and a disposable arachnoid knife)
- Colorado tip electrocautery
- Multiple no. 15 blades (for STA dissection)
- Papaverine
Operating Room Set-up
- Electroencephalogram tech is in the room, with EEG monitors available for viewing.
- Microscope set for an assistant on the right side of the surgeon (assuming a right-handed surgeon).
- Scrub is also on the surgeon’s right
- Immediate equipment on Mayo stands over the patient’s torso
- Microscope is positioned with the base to the left of the surgeon.
- Anesthesia team is to the surgeon’s left as well.
Anesthetic Issues
- Anesthetic management is critical to the success of the operation.
- Hypotension, hyperthermia, and hypercarbia are to be avoided at all times, especially during induction.
- Electroencephalogram technicians must communicate changes in the EEG to allow the team to respond immediately, with appropriate changes in blood pressure, partial pressure of carbon dioxide, and anesthetic agents.
♦ Intraoperative
Positioning
- Electroencephalogram electrodes are affixed and the scalp is shaved over the expected course of the STA based on the angiogram.
- The STA is mapped out using the Doppler probe, and the skin is carefully marked to outline its course from the distal end near the vertex to the root of the zygoma.
- The head is placed in pin fixation and the patient is positioned supine with the head turned parallel to the floor, such that the STA site is level.
- Rolls are used as needed to reduce tension on the neck, and the head is translated superior to the torso to facilitate venous drainage.
- The STA site is prepped, usually leaving the ear and face out of the field (Fig. 157.1A).
Description of Technique
- Prior to incision, intravenous antibiotics are given.
- Microscope is employed from the onset of the case.
Vessel Dissection
- Using high magnification, a no. 15 blade is used to score the dermis at the distal end of the STA (Fig. 157.1A).
- A thin, curved pediatric hemostat and toothed Adson pickups are used by the surgeon (with suction and a second pickups by the assistant) to identify the STA under the skin.
- Using a repeated technique of subcutaneous dissection with the hemostat over the STA, followed by elevation of the skin by the hemostat and an incision over the hemostat by the assistant, the STA is dissected close to the root of the zygoma.
- Care must be taken to avoid tearing the vessel, particularly at tortuous bends or side branches.
- Irrigating bipolar (usually set at 25 with fine tips) is employed for hemostasis of small scalp vessels
- A Cottonoid is often useful to cover the distal opening as proximal dissection continues.
- A longer length of STA dissection is preferable (10 cm is optimal).
- A Colorado needle (Stryker) electrocautery device (at low settings) is used in conjunction with the bipolar and microscissors to divide the galea and soft tissue on either side of the STA down to the temporalis fascia, leaving
- One to 2 mm of cuff on either side of the vessel
- Two self retaining retractors are used: one proximal, one distal
- One to 2 mm of cuff on either side of the vessel
- Dissection often terminates at the takeoff of the frontal branch which should be preserved if possible; if its takeoff is high, prohibiting mobilization of the STA, it often must be divided.
- The preoperative arteriogram will indicate whether the frontal branch provides any significant intracerebral collateral.
- A vessel loop is placed under the distal end of the STA and used to elevate the dissected portion of the vessel from the temporalis. The electrocautery is used to free up connective tissue around and beneath the vascular pedicle.
< div class='tao-gold-member'>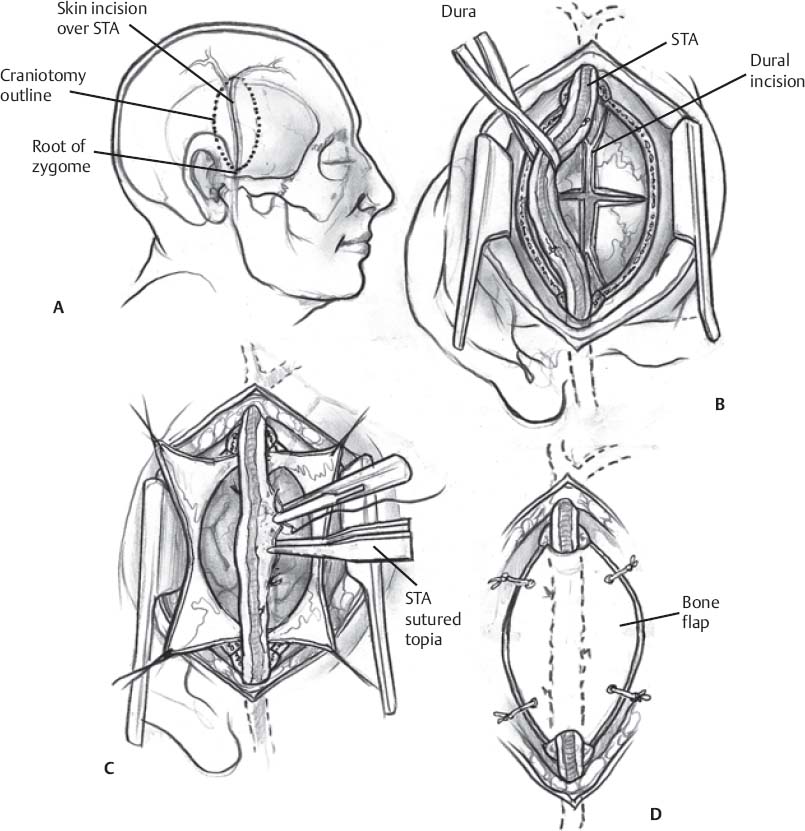
Fig. 157.1 Schematic of encephaloduroarteriosynangiosis. (A) Patient preparation and positioning. (B) Opening of the dura. (C) Microsurgical arachnoid opening and pial synangiosis. (D) Closure. STA, superficial temporal artery.
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







