Fig. 1
Angiographic pseudo-occlusion criteria of the ICA. (a) Severe stenosis of the ICA with a collapsed distal ICA. (b) Back filling of the ipsilateral carotid siphon via the ophthalmic artery. (c) Delayed antegrade flow of the patent ICA in the late arterial phase
Surgical Procedure and Postoperative Evaluation
Standard CEA techniques were utilized under general anesthesia. After the carotid bifurcation was exposed, the external carotid artery and common carotid artery were temporarily occluded, using clamps. The ICA was occluded as high as possible at the distal part and a longitudinal arteriotomy was done. Shunt use was based on the diameter of the collapsed distal ICA. Dissection and removal of the plaques and closure of the arteriotomy were performed under microtechniques. During the operation, a direct Doppler ultrasound scan was performed to detect pre- and postoperative blood flow volume. Perioperative management followed a protocol stipulated by Kyusyu Medical Center [3].
Atherosclerotic Plaque Analysis
The plaques were dissected from the bifurcation of the internal and external carotid arteries with CEA and fixed in 10 % buffered formalin. The specimens were transversely dissected into 3-mm-thick segments. Microscopic sections were cut from the paraffin-embedded tissue segments and stained with Hematoxylin and Eosin (H&E), elastica van Gieson (EVG), and Masson-trichrome (MT) for light microscopic examination. We observed the histological sections from all segments under a light microscope. To characterize the plaques, the lesion with the maximum degree of stenosis was subjected to histological evaluations. The percentage of atheromatous core of the total plaque area was visually estimated, with a division in three overall phenotypes: fibrous with a core of less than 25 %, fibroatheromatous with a core of 25–75 %, and atheromatous with a core exceeding 75 %. Plaque rupture, intraplaque hemorrhage, and fresh luminal thrombi were recorded as absent or present. Old organized thrombi were classified into absent, non-occlusive, or occlusive. Plaque analysis was performed by two pathologists (Y.H. and N.S.) who were blinded to the patient’s clinical information. Both pathologists independently performed semiquantitative analysis and the mean numerical values obtained from them was used for plaque analysis. Discrepancies were rare in the semiquantitative data between pathologists.
Postoperative Evaluations and Follow-up
Computed tomographic (CT) and magnetic resonance imaging (MRI) scans were performed in all patients within 1 week of surgery to evaluate the ischemic or hemorrhagic lesions related to the revascularization. In addition, DSA was performed 2 weeks after surgery in all patients. At follow-up periods, all patients were advised to undergo MRI and ultrasound 3 months after surgery and every year thereafter. Clinical data, including the atherosclerotic risk factors, neurological presentations, angiographic findings, and surgical outcomes, were derived from hospital records. This study was performed in compliance with protocols stipulated by the Fukuoka University Faculty of Medicine, Human Research Subject Committee, and Kyusyu Medical Center Research Committee.
Results
Characteristics of Study Population
Of the 345 patients, 17 (4.9 %) satisfied the diagnostic criteria for PO of the ICA. The mean age of patients was 70.5 years, and 2 of the patients were women. Sixteen patients had hypertension, 7 had diabetes mellitus, 9 had hyperlipidemia, 2 had peripheral arterial disease, and 5 had ischemic heart disease. Four patients (23.5 %) were neurologically asymptomatic, 7 (41.2 %) had suffered a transient ischemic attack, and 6 (35.3 %) had had a minor stroke. Angiographically, ACoA-PCoA collateral flow pattern developed in 7 patients (41.2 %), ACoA/PCoA pattern in 7 patients (41.2 %), and leptomeningeal pattern in 3 patients (17.6 %). The mean time interval between the latest ischemic event and surgery in symptomatic patients was 2.2 months. Complete follow-up data (mean 20.2 months) were available for all 17 patients.
Intraoperative Findings
All atheromatous lesions were located at the origin of the ICA. Using a Doppler ultrasound microprobe during surgery, direct blood flow of the collapsed distal ICA could be detected in all patients. After arteriotomy, all atherosclerotic plaques were not extended more distally and could be exposed clearly. Retrograde sufficient blood flow was detected and a temporary intraluminal shunting was used in all procedures. A direct suture of the ICA, without patch technique, was performed in each patient. A direct Doppler ultrasound signal was registered at the end of surgery, and postoperative sufficient blood flow was detected in all patients. All procedures were successfully done with standard CEA techniques and there were no surgical complications.
Histopathological Findings
The plaques obtained from the PO patient demonstrated more fibrous sclerotic phenotypes. Of all 17 patients, the fibrous or fibroatheromatous plaques were present in 14 patients (82.4 %). The incidence of plaque rupture was high in PO patients (64.7 %). Nine patients (52.9 %) had intraplaque hemorrhage, 8 (47.1 %) had fresh luminal thrombi, and all had old organized thrombus. Of all 17 old organized thrombus, nonocclusive thrombus was found in 9 patients (52.9 %) and occlusive thrombus was in 8 plaques (47.1 %). In other words, PO had two different histological features, the presence or absence of the true lumen. Plaques of total occlusion with recanalization (8 patients) were thrombotic occlusion with lumen recanalization by large neovascular channels (Fig. 2a, b), while those of severe stenosis (9 patients) were fibrous or fibroatheromatous with severe stenosis of the original lumen (Fig. 2c, d).
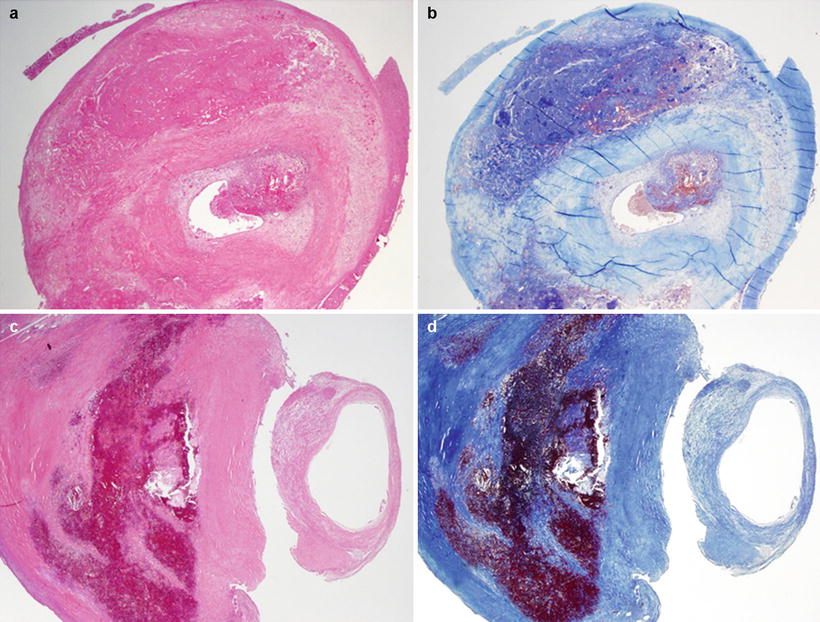
Fig. 2
Representative photographs of carotid artery pseudo-occlusion plaques showing two different features. (a, b) A patient with pseudo-occlusion without true lumen has thrombotic organized total occlusion of the ICA with recanalization by neovascular channels. (c, d) A patient with pseudo-occlusion with true lumen has hard plaque with severe stenosis consisting mainly of fibrous tissue accompanied by intraplaque hemorrhage. H&E (a, c) and MT (b, d)
Surgical Outcome and Follow-up
No new ischemic or hemorrhagic lesions were found on CT or DWI MRI within 1 week of surgery. Of all 17 patients who underwent DSA 2 weeks after CEA, 16 patients (94.1 %) were successfully treated, and we observed satisfactory dilatation of the ICA. In one case (5.9 %), (symptom free), we noted complete occlusion of the ICA and underwent superficial temporal artery-middle cerebral artery anastomosis. During the follow-up periods, 2 patients (11.8 %) showed restenosis of the ICA. One patient had suffered transient monocular blindness 8 months after surgery and an immediate DSA demonstrated moderate stenosis of the ICA. Another patient was symptom-free and restenosis was detected on MRA and ultrasound 12 months after surgery. Both patients were treated with carotid artery stenting, resulting in satisfactory dilatation. Three patients with complete occlusion or restenosis of the ICA had histologically more fibrous sclerotic plaques.
Discussion
The aim of this study was to discuss the pathogenesis of PO and whether CEA could be an effective treatment for PO, based on the clinicopathological results. Our findings indicate that the PO plaque compositions may be one of the factors, causing reduction of the flood flow and collapsed distal portion. Alternatively, PO is a lesion treatable by CEA with minimum risk and a high success rate, and the plaque histology can be related to the surgical outcome. It is widely accepted that primary carotid artery stenotic lesions are caused by advanced atherosclerosis [8, 16]. The rupture of unstable plaques, characterized as having a large atheromatous core, thin fibrous cap, and infiltration of inflammatory cells, causes thrombotic events and is followed by plaque stabilization, including reorganization and fibrosis, over time [12]. In our group, plaque rupture and intraplaque hemorrhage were detected in approximately 50 % or more, which was compatible with other reports [8, 16], although fibrous or fibroatheromatous plaques were prevalent, and old organized thrombi were frequently found in the PO patients. These findings indicate that considerable time had passed since the initial thrombotic events. PO plaques had two subtypes of old organized thrombi, occlusive or non-occlusive of the original lumen; in other words, PO had two different histological features. Plaques of the total occlusion with recanalization (8 patients, 47.1 %) were composed of thrombotic total occlusion and lumen recanalization by large neovascular channels, whereas those of severe stenosis (9 patients, 52.9 %) were fibrous sclerotic plaque with severe stenosis of the original lumen. It is interesting to speculate as to why the PO falls into collapse and not into complete occlusion, despite severe stenosis. The abrupt increase in the degree of stenosis, reducing blood flow and collapse of the distal ICA, could be explained by either disrupted intraplaque hemorrhages with some connection to the arterial lumen or expanded intraplaque hemorrhages without plaque disruption or luminal extension [1, 16]. Plaques of the total occlusion with recanalization could be structured by the luminal thrombi arising from intraplaque hemorrhage with plaque disruption. On the other hand, plaques of severe stenosis might be formed by subluminal hemorrhages without plaque disruption or luminal extension. However, various clinicopathological features may occur, depending on the degree of stenosis, the site, and the plaque compositions [1, 13]. The angiographic appearance of PO may be caused not only by the severity of stenosis but also by plaque compositions. Changes in plaque compositions from atheromatous to fibrotic may reduce the intraluminal pressure and collapse the ICA distal portion. Symptomatology, acute occlusive thrombosis of the carotid arteries may be either asymptomatic or present with only mild symptoms if the Circle of Willis or other intracranial collateral circulation is adequate, as in our cases. This finding suggests that the adequate collateral flow plays an important role in maintaining the intraluminal blood pressure and delayed anterograde flow of the patent ICA. The natural history of PO of the ICA is obscure. A success rate of revascularization for PO was reported from 75.0 to 100 % in previous literature [5]. Several authors have described that CEA for PO is less beneficial. However, Morgenstern et al. reported that surgery for PO was indeed of benefit and resulted in a reduction of the stroke rate [10]. In our series, of all 17 patients, 16 (94.1 %) were successfully treated without perioperative complications. Our surgical results were also favorable compared with other previous reports. Of all 17 patients, 1 (5.9 %) showed occlusion of the ICA on DSA 2 weeks after surgery. Greiner et al. pointed out that frequent causes for failure of reconstruction are hypoplastic or fibrotic vessels, chronic subtotal thrombosis, or simply too long an interval between the initial diagnosis and intra-operative evaluation [5]. The present case involved a histologically fibrous plaque with severe stenosis, indicating that progression of atherosclerosis extended to the distal ICA and the fibrotic vessel wall could prevent satisfactory dilatation of the ICA. During the follow-up periods, restenosis was encountered in two patients (11.8 %), and they were successfully treated with CAS. Hellings et al. described that plaque composition is an independent predictor of restenosis after CEA and a lipid-rich, inflammatory plaque is associated with a reduced risk of restenosis [6]. In our study, two plaques with ICA restenosis were fibrous, indicating that the plaque compositions might be useful to identify a patient with restenosis after surgery. Recently, CAS has been developed as an alternative treatment to CEA in carotid atherosclerotic disease, and the advantages and disadvantages of each procedure are currently under discussion. Terada et al. described that CAS for PO under embolic protection was beneficial and resulted in a reduction of the stroke rate [15]. The indications for carotid artery revascularization have been basically determined by the degree of stenosis, but it is important to evaluate the plaque compositions. We demonstrated that PO plaques had two different histological features, including the thrombotic occlusion with recanalization or severe stenosis. Plaques of severe stenosis could be treatable with CEA or CAS; in contrast, those with total occlusion with recanalization, in the absence of true lumen, could be suitable for CEA because it seemed to be difficult for endovascular devices to pass through the arterial lumen.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








