The thyroid gland and surrounding structures
Thyroidectomy
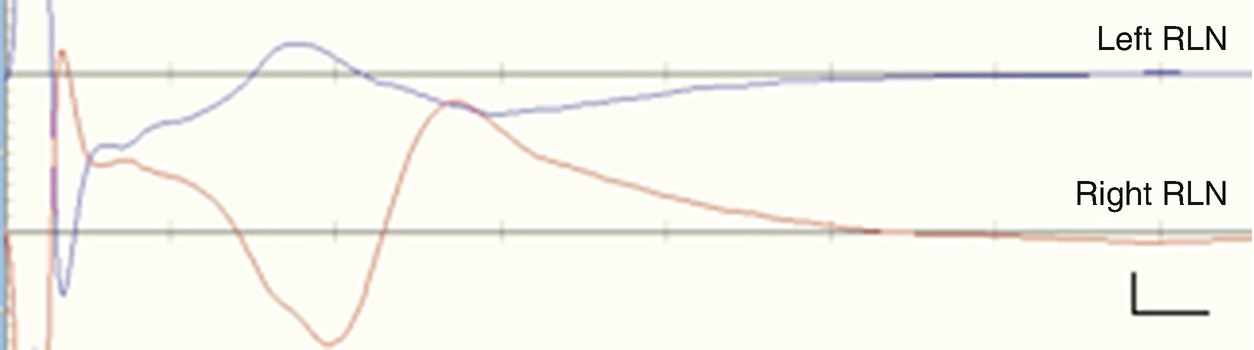
Removal of the thyroid gland is indicated for a variety of conditions including tumor, goiter , or hyperthyroidism among others. Depending on the pathology, one (hemithyroidectomy) or both (total thyroidectomy) lobes may be removed. To access the thyroid and/or parathyroid glands, a horizontal incision is made across the front of the neck followed by a longitudinal incision through the strap muscles. Division of the local vasculature follows division of the musculature so that the lobes of the thyroid can be mobilized. RLN identification is the first goal of IOM for thyroidectomy and is essential for the purposes of avoiding the nerve during the procedure. Identification of the RLN is only assured when electrical stimulation results in a recorded compound muscle action potential (CMAP) from the vocalis muscle on the EMG recording.
The Recurrent Laryngeal Nerve
The RLN is a branch of the vagus nerve (CNX) that supplies motor function and sensation to the larynx. It innervates all of the intrinsic muscles of the larynx except the cricothyroid muscle, which is innervated by the superior laryngeal nerve (SLN) . The RLN branches from the vagus nerve at the level of the subclavian artery on the right and the aortic arch on the left. After looping under the respective artery, the RLN ascends along the tracheoesophageal groove. The paired nerves are named “recurrent” because after branching, they turn back or run in a direction opposite to the vagus nerve. A minority of patients have a nonrecurrent laryngeal nerve branching off the vagus nerve at the level of the cricoid. During surgery, the RLN can be injured in a number of ways: complete or partial transection, traction, compression, misplaced ligature, thermal injury, or ischemia [3]. If the RLN is injured, it can result in temporary or permanent nerve paralysis. If the damage is unilateral, the patient may wake up with hoarseness. If there is bilateral nerve palsy, the airway may be compromised, resulting in dyspnea and in severe cases the need for a tracheostomy. The RLN also provides sensory innervation to the glottis, and a deficit may result in problems swallowing. Rates of injury range from 1% to 8%, with significantly increased risk to the RLN when surgery is for re-exploration, thyroid carcinoma, and total thyroidectomy [3–5]. In addition to thyroid and parathyroid procedures, the RLN is often monitored during ACDF, aortic arch procedures, carotid endarterectomy, and posterior fossa surgeries in order to avoid potential injury due to traction or nerve entrapment between the cuff of the ET tube and the retractor blades [6–8]. The SLN can also be injured during surgery [9, 10]. To monitor the SLN, the surgeon must place electrodes/needles in the cricothyroid muscle [9, 10]. Damage to the SLN results in a monotone voice or inability to change pitch.
RLN Monitoring
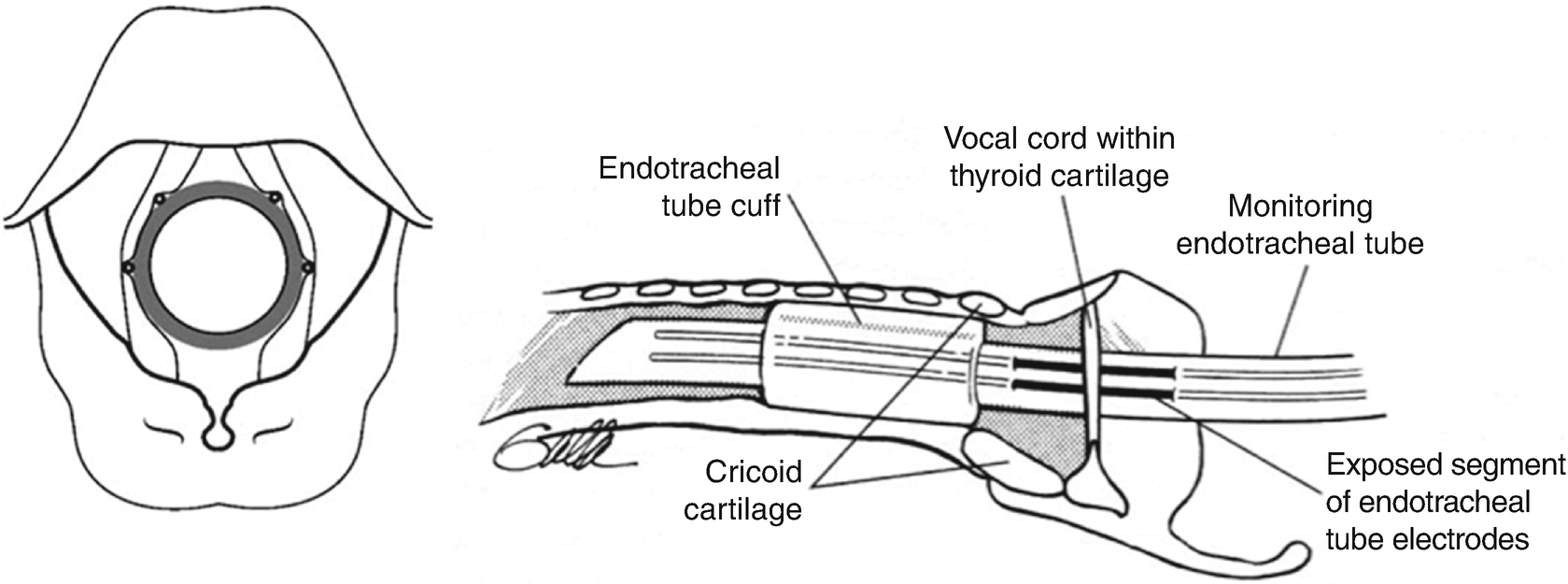
Proper placement of endotracheal tube electrodes
Unlike EMG from spinal nerve myotomes, baseline EMG recorded from the vocal cords should exhibit baseline activity. Baseline EMG amplitudes of 25–50 μV are most commonly observed with proper electrode placement because the presence of baseline activity is because the vocal cords are contracted at rest and relaxed when speaking. Failure to record baseline activity may be due to a number of factors including misplaced tube, the use of lidocaine, or residual neuromuscular blockade. Asymmetric baseline activity may indicate that the ET tube and electrodes are rotated and not in contact with one side of the vocal cords. Inadequate baseline recordings will prevent proper monitoring during the case and could result in false-negative results. It is important to correct electrode placement if necessary. This is accomplished by asking the anesthesiologist to move the endotracheal tube while the monitorist views the live EMG recording. As the electrodes move into proper position, the amplitude of recorded activity on the screen will increase. The tube depth showing maximal EMG activity should be marked where the tube meets the teeth, and the tube should then be secured. It is not unusual for baseline activity to decrease in amplitude during the procedure as a result of changes in electrode impedance resulting from secretions.
Identification of the RLN is one of the first steps in the thyroidectomy procedure. One technique, called sweeping, is used to aid the surgeon in initial dissection. Monopolar stimulation is used for the sweeping technique. The surgeon is given a handheld monopolar probe and the monitorist will stimulate continuously (at approximately 2 mA) while the surgeon sweeps the field in search of the nerve. The presence of a CMAP response indicates that the nerve is in proximity. There are technical considerations that the monitorist should be aware of during sweeping. The presence of blood or irrigation in the surgical field may shunt current away from the nerve and prevent a response from being seen despite proximity of the nerve to the stimulator [2]. It is therefore important that the surgical field remain dry when stimulating.
The stimulation parameters for sweeping are different than for direct nerve stimulation. The first difference is the use of a monopolar stimulator versus a bipolar stimulator used for direct nerve stimulation. Monopolar stimulation induces a larger current field and is said to be more sensitive than bipolar stimulation. Bipolar stimulation (having the cathode and anode in close proximity) has a smaller current field and while less sensitive is more specific. The stimulation intensity used for sweeping is higher than for direct nerve stimulation. Continuous stimulation up to 3 mA (pulse width not to exceed 50–100 μs) is performed until a response is seen. Once a response is recorded at supramaximal intensity, the intensity is reduced and the threshold for response determined. If there is no current shunting, the stimulation threshold can be used as an indicator of the distance to the nerve. The response should likewise increase in amplitude as the stimulator approaches the nerve.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







