CHAPTER 323 Epidemiology of Traumatic Brain Injury
Traumatic brain injury (TBI) constitutes a critical public health and socioeconomic problem throughout the world.1–3 It is the leading cause of mortality and disability among young individuals in high-income countries. Worldwide, the incidence of TBI is rising sharply, mainly because of increasing motor vehicle use in low- and middle-income countries.
TBI will surpass many diseases as the major cause of death and disability by the year 2020.4 It is often referred to as a silent epidemic5—silent because patients are not vociferous as a consequence of the nature of the disease and its sequelae, as well as because society in general is largely unaware of the magnitude of the problem.
Definitions
Epidemiology
The prevalence of TBI is the total volume of TBI (existing plus new cases) at a given point (point prevalence) or in a given period (period prevalence). It should encompass all persons living with the sequelae of TBI, such as handicaps, impairments, disabilities, and complaints, together with all new TBIs. Unfortunately, very few longitudinal studies exist, follow-up is often short, and loss to follow-up is frequent in TBI cohorts.6
For these reasons, the use of a standardized mortality rate is generally accepted in many fields of medicine. Standardized mortality rates compare the number of expected deaths with the number of observed deaths. This indirect standardization method adjusts for differences in baseline characteristics to permit comparisons over time or between different settings. Standardized mortality rates are generally adjusted for age and sex. In intensive care medicine, standardized mortality rates are adjusted for baseline characteristics and based on scoring systems such as the Acute Physiology, Age, and Chronic Health Evaluation (APACHE) II; the Trauma and Injury Severity Score (TRISS); or the Simplified Acute Physiology Score (SAPS) 2/3. These prognostic scores, however, have not been developed specifically for TBI, and their applicability to TBI is doubtful. We see a clear need for developing a system to calculate standardized mortality rates in the field of TBI that adjusts for baseline characteristics, is available on admission, and uses prognostic models.7
Limitations and Gaps in Our Knowledge of the Epidemiology of Traumatic Brain Injury
Ongoing efforts to quantify the magnitude of the problem posed by TBI are limited by many factors.
We recently proposed the following definition for TBI: “brain damage resulting from external forces, as a consequence of direct impact, rapid acceleration or deceleration, a penetrating object (e.g., gunshot) or blast waves from an explosion. The nature, intensity, direction and duration of these forces determine the pattern and extent of damage.”8 Other definitions also include patients with subtle behavioral or neuropsychological changes reported at some time after possibly trivial injury. In addition, it has been suggested that patients who at the time of injury have an alteration in mental state (e.g., confusion, disorientation, slowed thinking) be included in the definition of TBI.
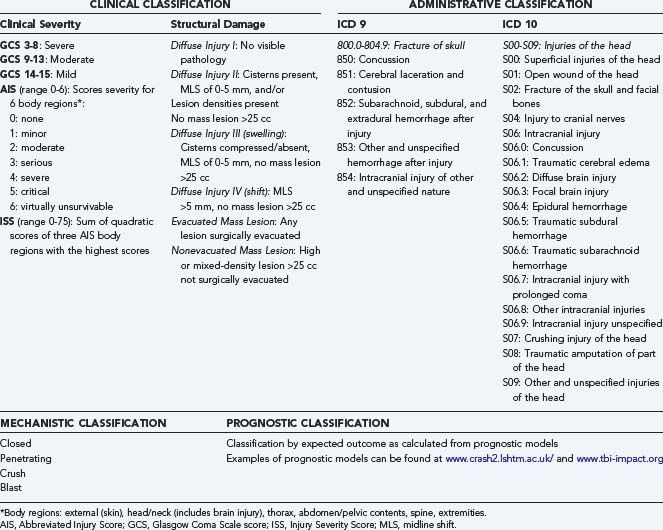
Fourth, when data are collected, they are often identified by codes of the International Classification of Diseases (ICD), which were more pathologically based in the ICD 9 classification (Table 323-1), whereas the newest ICD 10 classification is more clinically oriented. Neither of these two classification systems, however, capture reliable information on the severity of injury. Both the ICD 9 and ICD 10 classification systems are primarily intended for administrative use and therefore have substantial limitations.
Classification of Traumatic Brain Injury
Epidemiologic studies on TBI are more or less based exclusively on the administrative classification of the ICD 9 or ICD 10 codes. In ICD 9, different codes are not mutually exclusive, which results in problems and variability in coding, and the coding in no way reflects the actual clinical severity of injury.9 Similar criticism is applicable to the ICD 10 codes. High agreement (96.5%) between the ICD 9 and ICD 10 codes in identifying TBI has been reported.10
In clinical medicine, scoring systems are frequently used to classify the severity of injury (see Table 323-1). The clinical severity of intracranial injuries is commonly assessed according to the degree of depression of the level of consciousness as assessed by the GCS.11 The GCS consists of the sum score (range, 3 to 15) of three components (eye, motor, and verbal scales), each assessing different aspects of reactivity. The motor component provides more discrimination in patients with severe injuries, whereas the eye and verbal scales are more discriminative in patients with moderate and mild injuries. For assessment of severity in individual patients, the three components should be reported separately. For purposes of classification, however, calculation of the sum score is useful. Severe TBI is defined as a GCS score of 3 to 8, moderate TBI as a GCS score of 9 to 13, and mild TBI as a GCS score of 14 to 15. A limitation of classifying clinical severity with the GCS is that accurate assessment may be confounded by the prehospital use of sedation and paralysis.12,13 The severity of extracranial injuries is commonly scored according to the Abbreviated Injury Score (AIS)14 or the Injury Severity Score (ISS).15 TBI is associated with extracranial injuries (limb fractures, thoracic or abdominal injuries) in about 35% of patients.16 Extracranial injuries increase the risk for secondary damage as a result of hypoxia, hypotension, pyrexia, and coagulopathy. In the assessment of overall injury severity, therefore, recording of the severity of extracranial injuries is highly relevant.
Assessment of the extent of structural damage is commonly performed according to the Marshall CT classification. This classification was proposed by Marshall and colleagues in 1991 as a descriptive system that focused on the presence or absence of a mass lesion.17 The scale further differentiates diffuse injuries by signs of increased intracranial pressure (e.g., compression of the basal cisterns, midline shift). This classification has limitations, however, such as broad differentiation between diffuse injuries and mass lesions and lack of specification. For purposes of prognosis, better discrimination can be obtained by combining information available from individual CT characteristics into a prognostic model. A score chart for applying such a score has been proposed by Maas and associates.18 A different approach to classifying patients is by prognostic risk. Recently, well-validated models developed from large patient samples have become available to facilitate this approach.19,20 Prognostic classification can serve various purposes, including comparison of different TBI series, quality assessment for the delivery of health care, and support of the analysis of clinical trials. All these approaches to classification are characterized by some form of scoring of severity.
The Impact of Traumatic Brain Injury from A Global Perspective
TBI is a major health and socioeconomic problem that affects all societies around the world. Globally, in excess of 10 million people suffer TBI serious enough to result in death or hospitalization each year.21 In 2003, in the United States alone there were an estimated 1,565,000 TBIs resulting in 1,224,000 emergency department visits, 290,000 hospital admissions, and 51,000 deaths.22 The prevalence of TBI in the United States has been estimated at approximately 5.3 million. In the European Union with 330 million inhabitants, approximately 7,775,000 new TBI cases occur each year. Worldwide, TBI will surpass many diseases as the major cause of death and disability by the year 2020.4 It has been estimated that TBI accounts for 9% of global mortality and is a threat to health in every country in the world. For every death there are dozens of hospitalizations, hundreds of emergency department visits, and thousands of doctor appointments. A large proportion of people surviving their injuries incur temporary or permanent disability. Brain trauma accounts for approximately a third of all injury-related deaths and the majority of permanent disability. Despite the success of preventive measures, injuries, including unintentional injuries, homicide, and suicide, are the leading cause of death in the United States and Europe in individuals younger than 45 years. In low- and middle-income countries, the incidence of TBI is rising sharply because of increasing motorization. Most patients with TBI have milder injuries, but residual deficits are common.23 TBI occurs more frequently in young adults, particularly males, and has a high cost to society because of life years lost as a result of death and disability. The financial burden of TBI has been estimated to be greater than $60 billion per year in the United States alone.24 The true cost is even higher in that this figure does not address the indirect effects on families or other caregivers. These numbers stand in stark contrast to the amount of funding for TBI research, which has one of the highest unmet needs within the already severely underfunded field of brain research.
Incidence
Given the gaps and limitations in our knowledge of the epidemiology of TBI described previously, the epidemiologic data reported in the literature need to be interpreted with great caution. Table 323-2 presents a summary overview of reported incidence rates across the world.6,10,25–40
TABLE 323-2 Incidence of Traumatic Brain Injury across the World
| REGION | INCIDENCE/100.000 | REFERENCE |
|---|---|---|
| United States | 103 | Kelly and Becker,25 2001; Thurman et al.,26 1999; Langlois et al.,10 2006 |
| European Union | 235 | Tagliaferri et al.,6 2006 |
| Germany | 340 | Firsching and Woischneck,27 2001 |
| Italy | 212-372 | Servadei et al., 1988,28 200229; Baldo, et al.,30 2003 |
| Denmark | 157-265 | Engberg and Teasdale,31 2001 |
| Finland | 101 | Koskinen and Alaranta,32 2008 |
| Norway | 83-229 | Ingebrigtsen et al.,33 1998; Andelic et al.,34 2008 |
| Sweden | 354-546 | Andersson et al.,35 2003; Styrke et al.,36 2007 |
| Brazil | 360 | Maset et al.,37 1993 |
| China | 55-64 | Zhao and Wang,38 2001 |
| Pakistan | 50 | Raja et al.,39 2001 |
| South Africa | 316 | Nell and Brown,40 1991 |
This table illustrates the large variation in reported incidence rates, which is primarily due to varying definitions of injury, different inclusion criteria in addition to actual differences, and sampling errors.41 The approximate incidence of 103 per 100,000 for the United States represents the best estimate from CDC data.10 Kelly and Becker reported a range of 132 to 367 per 100,000 with an estimate of around 100 per 100,000 at the time of the study in 2001.25 Thurman and colleagues reported a decrease in incidence of 234 per 100,000 in 1975 to 90 per 100,000 in 1994.26
The overall incidence of 235 per 100,000 reported by Tagliaferri and colleagues in 2006 is derived from a systematic review of 23 reports on national and regional epidemiologic studies carried out on TBI in Europe.6 Wide variation in reported incidence ranging from 20 (only neurosurgical cases) to 546 (including emergency department visits, hospital discharge, and coroner reports) was noted. This latter figure is very consistent with the 538 per 100,000 reported for the United States in a nationwide survey, including emergency department visits, hospitalizations, and deaths.22 A number of studies from Italy show relatively limited variability, with reported incidence figures of 212 to 372 per 100,000 per year, but in these studies inclusion criteria are also different. Some include tourists in a population-based analysis; others were performed in relatively small regions, which results in a referral bias because of transport of severe cases within the region.28,29,30,42 A number of studies have shown important regional variations. Population-based studies from Norway report an incidence of 229 per 100,000 in more rural areas33 and 83.3 per 100,000 in the Oslo area.34 Styrke and coworkers found an incidence of 354 per 100,000 in northern Sweden in 2007,36 as opposed to 546 per 100,000 in western Sweden.35 In Taiwan, the incidence in Taipei is approximately 218 per 100,000 versus 417 per 100,000 in more rural areas.43,44 Similar differences have also been reported in Australia.45
TBI is generally thought to occur predominantly in young adult males with a male-to-female ratio of 3:1.46 Recent studies from the International Mission for Prognosis And Clinical Trial (IMPACT) study group, however, have shown that the male preponderance decreases at lower and higher age groups and that in children, as well as in the elderly older than 65 to 70 years, there is no clear gender difference in the incidence of TBI (Fig. 323-1).
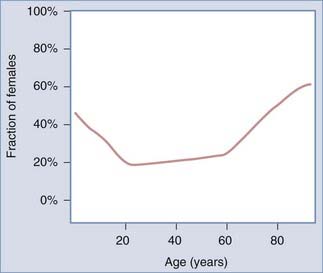
FIGURE 323-1 Male preponderance in traumatic brain injury is limited to those aged 20 to 60 years.
(From Mushkudiani NA, Engel DC, Steyerberg EW, et al. Prognostic value of demographic characteristics in traumatic brain injury: results from the IMPACT study.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree