Introduction
Episodic dyscontrol (ED) is a rare but severe form of human aggressive behavior. The following case report illustrates the phenomenology of such troubling paroxysmal behaviors.
A.E. was a 33-year-old white carpenter who was one participant of our study into episodic dyscontrol or intermittent explosive disorder in epilepsy at the Institute of Neurology.77 A.E. was completely healthy and did not suffer from any major medical, neurologic, or psychiatric condition up to the age of 28 years, when he developed herpes encephalitis and subsequently suffered from temporal lobe epilepsy (TLE). He presented to the Chalfont Centre with complex partial seizures with a frequency of two to three clusters of up to six seizures a day. On these occasions, he would feel agitated somewhat 2 to 3 hours prior to the seizure. He then typically would feel odd; both sides of his face would start twitching, followed by salivation. During these seizures, which lasted 2 to 3 minutes, he would be awake but unresponsive to other people, with eyes wide open. Once to twice a month, a classic secondary–generalized tonic–clonic seizure evolved out of such a complex partial seizure. Neuropsychiatric assessment revealed a normal interictal electroencephalogram (EEG) with no ictal EEG available at time of presentation. Structural magnetic resonance imaging (MRI) displayed bilateral hippocampal and amygdala volume loss and increased hippocampal signal in T2 images. On psychiatric assessment, there was no formal diagnosis, and in particular no evidence for any affective, psychotic, or personality disorder or attention-deficit hyperactivity disorder (ADHD) apart from episodic dyscontrol.
With a frequency of two to three episodes a year and a duration of 30 to 60 minutes, A.E. could behave in a very aggressive and violent way. Typically, there were no adequate triggers and a sudden onset of severe arousal, anger, and rage. The patient then became physically aggressive, attacking people and objects. The attack did not follow any obvious premeditated plan, and the behavior was poorly organized, with A.E. attacking every person or object at hand.
On one such occasion at the tertiary referral center, A.E. was queuing for his medication when suddenly he gripped a nearby billiard stick, hitting the nurses and fellow patients at hand. He then left the ward and destroyed three cars before he could be restricted by the police. During this episode, there was no obvious evidence for an epileptic seizure and no evidence for hallucinations or persecutory delusions. The day before the attack, the he had had a pint of lager beer; apart from that, however, there was no evidence for any other drug abuse. The day after the attack, the patient felt extremely ashamed for this behavior. He could not recall and describe his feelings and thoughts during the episode in detail and remained vague in his recollection of the scene. At the same time, he was not absolutely amnesic and felt very guilty and depressed because of this behavior.
This case illustrates the complexity and danger of episodic dyscontrol and illustrates why many authors believe that ED might be related to epilepsy in particular because of its paroxysmal nature. Before we discuss the precise phenomenology and neurobiology of ED, however, we first have to clarify the relationship of this special form of aggressive behavior to aggression and violence as a general phenomenon of human life.
Human aggression is an important social and clinical problem.32,67,75,82 The phenomenologic and probably neurobiologic heterogeneity of aggressive and violent behaviors is a major scientific problem leading to difficulties in assessment and classification. An important distinction has emerged between the terms violence and aggression. Treiman defined violence as forceful infliction of abuse or damage on another individual or object.81 However, according to this concept, violence is not necessarily the result of intentional aggression. Aggression, in contrast, is defined as an offensive action directed toward another individual or object with the premeditated intention to harm, threaten, or control other subjects, groups, or situations.81
An advantage of this distinction is that it can be used to describe different destructive behaviors more precisely by referring to a special mental state, that is, the intentionality that does or does not motivate the destructive behavior. It leaves researchers with the problem of assessing intentionality, however, which in clinical practice is often impossible.
Therefore, it seems to be desirable to define phenomenologic criteria of specific behavioral syndromes of interest to obtain a nontheoretical approach to classifying aggressive and violent behaviors.
Classifying Aggression
One approach to doing this is to refer to basic research on animals. Here, aggressive behavior is classified according to the context in which it is observed. Authors like Moyer distinguished different subtypes of aggressive behavior in animals based on a precise characterization of the behavioral context in which such behavior is observed.55 For example, predatory aggression is defined as violent behavior in which a predator kills its prey. It is characterized by a calm and very concentrated mental state of the aggressive animal and behavior that is well structured and goal directed. Maternal aggression, in contrast, is characterized by high arousal of the aggressive animal and a specific situational trigger when its offspring is menaced by predator. Table 1 summarizes the context-specific classification of aggressive behavior in animals.
Table 1 Subtypes of animal aggression | |||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||
Contrary to animal behavior, human behavior depends less on external cues and stimuli, and behavioral programs are less preformed. Therefore a simple transfer of the context-based classification of animal aggression to human behavior is not
possible.42 Nevertheless, there is general agreement that at least two different phenomenologic and neurobiologic subtypes of aggressive behavior can be differentiated in humans: (a) predatory and (b) defensive aggression.35,42,55,56,85
possible.42 Nevertheless, there is general agreement that at least two different phenomenologic and neurobiologic subtypes of aggressive behavior can be differentiated in humans: (a) predatory and (b) defensive aggression.35,42,55,56,85
Predatory aggression as described earlier is characterized semiologically as a well-structured and goal-directed behavior performed in an emotionally calm and concentrated state of mind. Defensive aggression, in contrast, is generally seen in the context of high emotional arousal and is associated with vocalizations and signs of anger or fear. The behavioral pattern itself is less structured and is defensive.83
Most forms of human aggression that are generally seen in a clinical context are considered to be defensive, that is, the behavior is generally poorly structured and a reaction toward a perceived threat, be it adequate or not.2 Obviously, the perception of whether a stimulus is threatening is decisive in the information processing leading to this kind of aggressive behavior. However, there are also forms of offensive aggression that are often seen in criminals or patients with a diagnosis of dissocial personality disorder (ICD-10 Classification of Mental and Behavioural Disorders [ICD 10] F60.2), conduct disorder in adolescents, or hyperkinetic disorder of social behavior (ICD-10 F90.1).
Aggressive Behavior in Clinical Practice
In clinical practice, aggressive behavior can be observed in the context of different medical, neurologic, and psychiatric disorders and diseases. In patients with mental retardation, it is a common problem, possibly as a consequence of impaired social perception or deficits in expressing personal needs.9,37,44,67 Furthermore, aggression is often seen in the context of organic brain disease such as frontal or hypothalamic brain tumors, neurodegenerative disease, delirium, or drug abuse. These common forms of aggression in the clinical setting tend to be malstructured, defensive, and generally occur in the context of states of confusion and diffuse emotional arousal.
Well-structured, premeditated, and goal-directed aggressive behaviors can occur on the background of psychiatric disorders such as psychosis with delusional states, ADHD, or bipolar disorder. It is frequently observed in patients with antisocial personality disorder (APD), in which it is part of the characteristic traitlike behavior.9,53,71
The only clinical syndrome of aggression that has been identified as a distinct category in the international classificatory system is intermittent explosive disorder (IED) according to the guidelines of the Diagnostic and Statistical Manual of Mental Disorders, 4th ed. (DSM–IV).5 The concept of IED has been modeled on the clinical descriptions of episodic dyscontrol.8
Phenomenology of Episodic Dyscontrol
As mentioned, IED is basically a synonym for episodic dyscontrol. Because IED is an internationally accepted diagnostic construct, we will use this term in this chapter rather than ED. Both entities are characterized by several discrete episodes of failure to resist aggressive impulses that result in serious assaults or destruction of property. The behavior is out of proportion to any apparent precipitating psychosocial stressors and is not due to substance abuse, another mental disorder such as personality disorder, any other first-axis psychiatric disorder, or a general medical condition such as head trauma or neurodegenerative diseases. Consequently and in spite of the sometimes suggestive paroxysmal semiology, IED cannot be regarded as a special semiology of epilepsy. Whether this distinctive conception will stand the test of time, however, remains to be seen.
Epidemiology of Intermittent Explosive Disorder
There are only a few studies analyzing the prevalence of IED in primary medical settings. One study aimed at determining the lifetime and current prevalence of IED along with other demographic characteristics and patterns of comorbidity in an outpatient psychiatric sample of 1,300 individuals presenting for outpatient psychiatric treatment.21 Following structured diagnostic assessment for axis I and II disorders, the authors reported a lifetime prevalence of IED of 6.3% (SE, ±0.7%) and a cross-sectional prevalence of 3.1% ± 0.5% of psychiatric patients. IED was the current principal diagnosis in only 0.6% ± 0.2% of patients. Most of these patients (80%) were interested in treatment for their intermittent aggressive
behavior. The authors concluded that DSM-IV IED in psychiatric samples is far more common than previously thought and pointed out that IED develops early in life, especially in male patients.
behavior. The authors concluded that DSM-IV IED in psychiatric samples is far more common than previously thought and pointed out that IED develops early in life, especially in male patients.
Neurobiology of Intermittent Explosive Disorder
There are few studies looking at neurobiologic mechanisms specifically in IED. The fact that there is some controversy as to the reliability of the clinical diagnosis aggravates the problem of neurobiologic research into this entity.54 Nevertheless, there is some evidence that disturbances of the functional integrity of frontotemporal brain circuits might play an important role in the genesis of IED and ED.
Clinical Studies
There are numerous studies addressing the relationship between focal lesional brain pathology and aggressive and impulsive behavior. Prefrontal brain damage and in particular orbitofrontal brain pathology have been closely associated with aggressive dyscontrol.17 The specific entity of ED or IED has scarcely been addressed in any of these studies, however, although there are a few cases in which ED has been related to hypothalamic or basal ganglia lesions.27,80
With respect to neurochemical brain pathology, there is some vague evidence that functional disturbances of the serotonergic system might play a critical role in impulsive aggression in general.43 In fact, one consistent finding in biologic psychiatry is an association between low cerebrospinal fluid 5-hydroxyindole acetic acid levels and impulsive aggressive acts, suggesting a decreased serotonin turnover. Again, however, there no specific studies in IED or ED.
Electroencephalographic and Imaging Studies
EEG studies point to an increased prevalence of unspecific EEG abnormalities in disorders with disturbed impulse control in general and ED in particular.12,30 Drake et al., for example, reported a significant increase of diffuse or focal slowing in the EEGs of ED patients as compared to healthy volunteers or depressed patients.30 N100 and P160 auditory-evoked potential amplitudes were lower in episodic-dyscontrol patients than in controls, but the difference was not significant. The authors concluded that such findings suggest that nonspecific cerebral dysfunction and EEG changes may be associated with disordered impulse or behavior control.30
A systematic literature review based on PubMed searches did not reveal any positron emission tomography, single photon emission computed tomography, or functional MRI study that specifically looked at neurobiologic mechanisms of ED or IED. There are two studies by our group, however, in which we addressed IED in the context of epilepsy, using structural MRI techniques.78,88
In these studies we hypothesized that, in patients with TLE and intermittent affective aggression, amygdala sclerosis in the context of hippocampal sclerosis would be more common as compared to control patients. In addition, we aimed to analyze a possible association between aggression on one hand and hippocampal sclerosis, low IQ, and poor social adjustment on the other in patients with TLE. In a further approach, we analyzed cortical gray matter abnormalities in these patients to gather evidence for frontal lobe pathology in patients with TLE and IED.
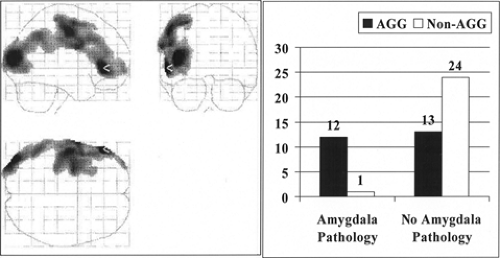
Amygdala Pathology in Patients With Temporal Lobe Epilepsy and Episodic Dyscontrol
For that purpose, we compared 25 patients with TLE and IED with 25 control patients with TLE without any psychopathology and 20 healthy volunteers.78 Both patient groups were matched for age, gender, demographic background, duration of epilepsy, and seizure severity. There was no significant group difference regarding the history of birth complications, febrile convulsions, or status epilepticus. In the IED group, however, the incidence of encephalitic brain disease (Fisher’s exact test: p = .05) and left-handedness (chi-square test: p < .05) was significantly increased. There was less right-sided focal EEG abnormality and more bilateral EEG abnormality in the aggressive group, and hippocampal sclerosis was significantly less common in patients with TLE and IED. Other left temporal pathology, including 3 patients with amygdala pathology (amygdala sclerosis, amygdala glioma, amygdala dysembryoplastic neuroepithelial tumor), 2 patients with multiple small temporal infarctions, and 2 patients with diffuse left temporal atrophy of unknown origin, was significantly more common in patients with TLE plus IED. In the aggressive patients, a subgroup of 5 patients (20%) showed amygdala atrophy as compared to only 1 in the nonaggressive group (chi-square test: p = .04). An increased incidence of encephalitis (chi-square test: p < .005; Fisher’s exact test: p = 0.1) was the only clinical feature that distinguished patients with amygdala atrophy from those with normal amygdala volumes. In 12 of 25 patients, we could prove some evidence of amygdala-related brain pathology as compared to only 1 in the nonaggressive group. Furthermore, there was a highly significant group difference in IQ figures, with the verbal IQ (VIQ), the performance IQ (PIQ), and hence the full IQ (FIQ) all being lower in the aggressive group. In addition, there was a significant group difference in Beck Depression Inventory and Spielberger State Trait Anxiety Index scores, with the aggressive group rating much higher in depression (p < 0.05), state (p < 0.05), and trait anxiety (p < 0.01).78
Cortical Abnormalities in Patients With Temporal Lobe Epilepsy and Episodic Dyscontrol
In a second analysis, we employed the method of voxel-based morphometry to detect possible subtle cortical brain pathology that was not present on visual assessment of the MRI scans analyzing the same study sample.88 Both TLE patient groups were compared with each other and with the control subjects on a voxel-by-voxel basis for increases and decreases of gray matter. Details of the methodology are published elsewhere.88,89 In this study, we were able to demonstrate reductions of gray matter density over large areas of the left extratemporal neocortex with maxima in the left frontal neocortex; one maximum difference projection had a Z score of 5.67 at Talairach coordinates x = 58, y = 36, z = 9 mm (left anterior frontolateral cortex), the other a Z score of 4.78 in a more-posterior left frontal lobe location (Talairach coordinates x = 66, y = 0, z = 28 mm). Patients with TLE who did not have IED showed no significant decrease of cortical gray matter compared with control individuals. Patients with TLE with IED also had reduction of left frontal gray matter compared with patients with TLE without IED, although this was less marked than when compared with control individuals (Z score of 3.49 at Talairach coordinates x = 66, y = 2, z = 26 mm). The statistical parametric mapping–based voxelwise correlation of social dysfunction and aggression scale scores and automatically segmented gray matter in all patients with TLE showed a left frontal gray matter area
being negatively correlated with these scores, which expressed social consequences of interictal affective aggression (Z score of 3.65 at Talairach coordinates x = 66, y = 2, z = 26 mm). Age, scores of depression and anxiety, IQ measures, or scores of verbal fluency did not significantly correlate with specific decreases in gray matter in all patients with TLE.88 FIGURE 1 illustrates the main findings from these two studies.
being negatively correlated with these scores, which expressed social consequences of interictal affective aggression (Z score of 3.65 at Talairach coordinates x = 66, y = 2, z = 26 mm). Age, scores of depression and anxiety, IQ measures, or scores of verbal fluency did not significantly correlate with specific decreases in gray matter in all patients with TLE.88 FIGURE 1 illustrates the main findings from these two studies.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree