CHAPTER 21 EXAMINATION OF THE VISUAL SYSTEM
VISUAL FIELD EXAMINATION
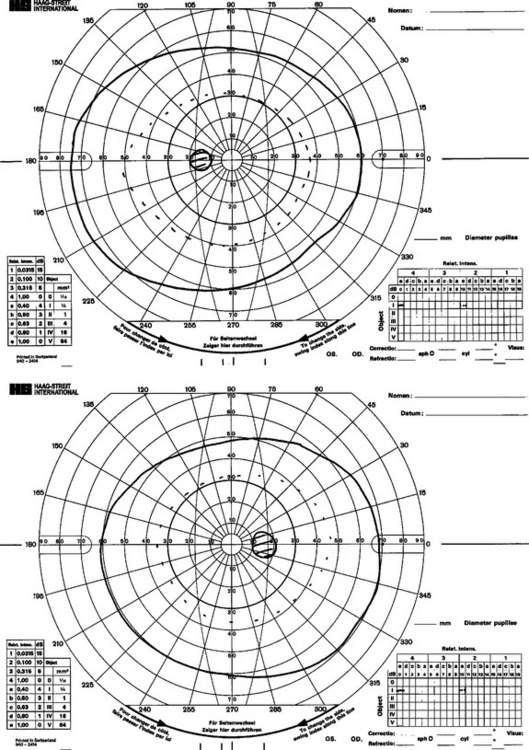
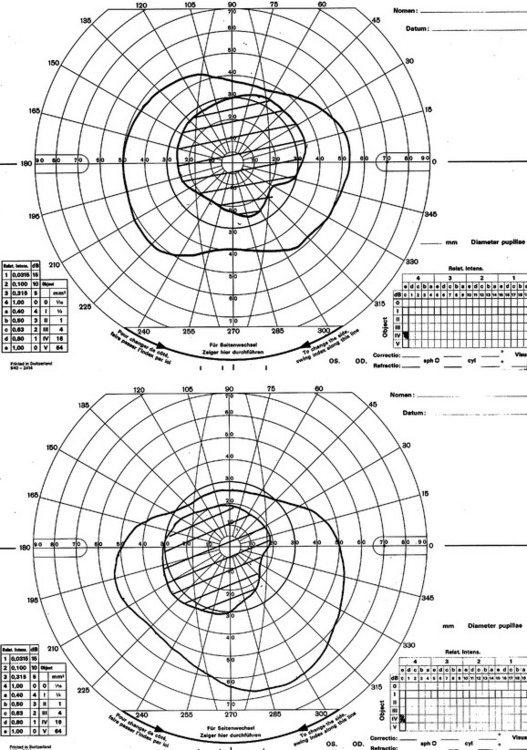
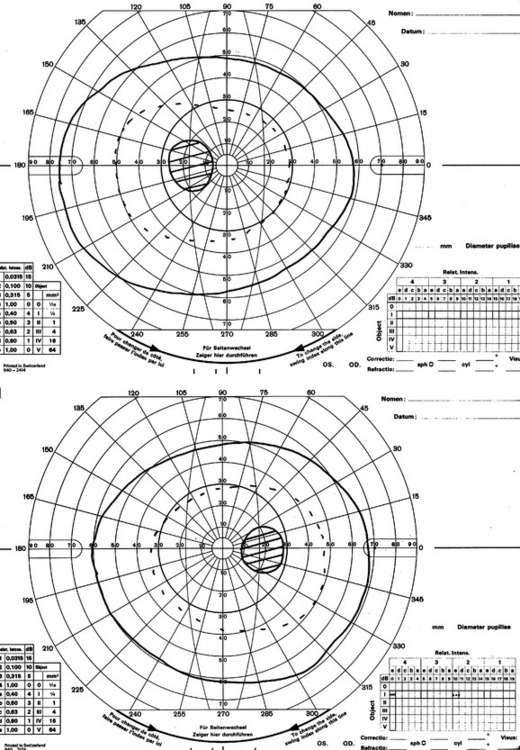
The principle behind dynamic perimetric methods of field analysis such as the Goldman is that the examiner is identifying successive boundaries of vision known as differential light sensitivities (DLSs). These are the thresholds within which it is possible for that part of the retina to identify when a light projected is more bright than the background. The fovea is most sensitive, and this reduces with distance from the fovea. The temporal field changes slowly with distance from the fovea, whereas the DLS on the nasal side reduces abruptly. A normal Goldman field is shown in Figure 21-1. The advantage of this method of field assessment is that the skilled examiner can plot very carefully visual field abnormalities and can return over and over again to check the boundaries of the field.
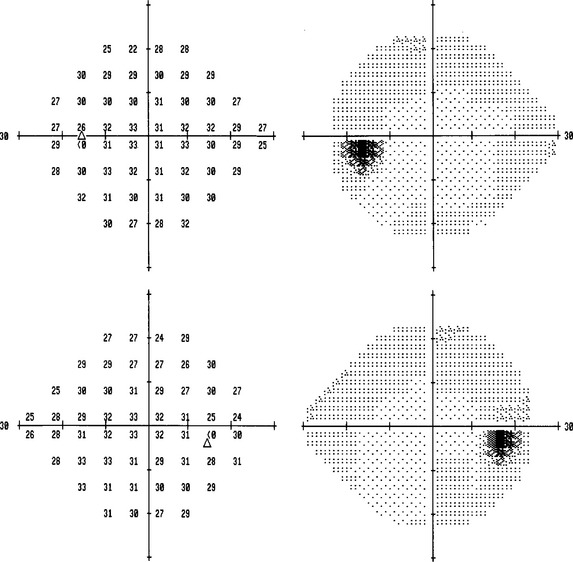
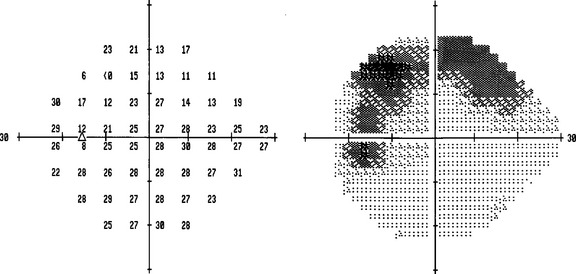
Automated static perimetry is available in all ophthalmic departments, can be carried out in around 10 minutes, is easy to administer, and does not require so much skill to perform. It is less sensitive a measure than the Goldman when the examiner is highly skilled in use of the latter. Automated static field tests identify the threshold of accurate vision within the four visual quadrants within a 10, 24-, 30-, or 70-degree field. Fields can be recorded for comparison with subsequent examinations; reliability can be assessed by noting fixation losses and false-positive and -negative errors. The gray scale indices note the mean or pattern deviation of the patient’s responses to those of age-matched normal controls (Fig. 21-2).
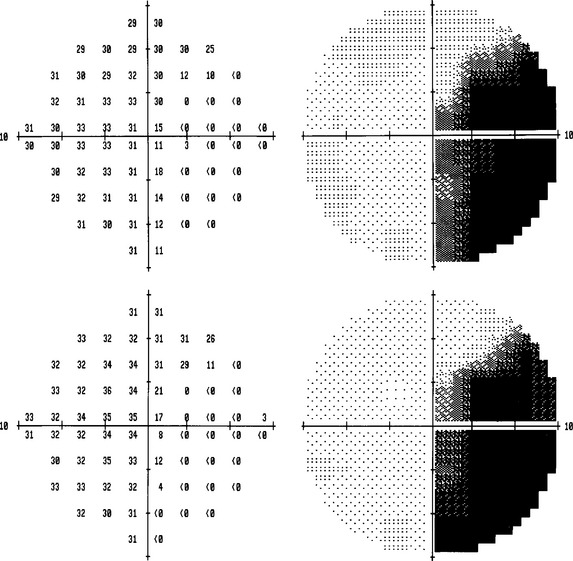
Factors that influence the precision of these field examinations include cognitive function and tiredness, refractive errors, and ophthalmic disorders such as cataract. The field is plotted at a certain level of background illumination because the threshold varies with background luminance up to a certain point and then increases in a linear way with suprathreshold background luminance. Examples of common field defects that are seen are shown in Figures 21-3 to 21-8.
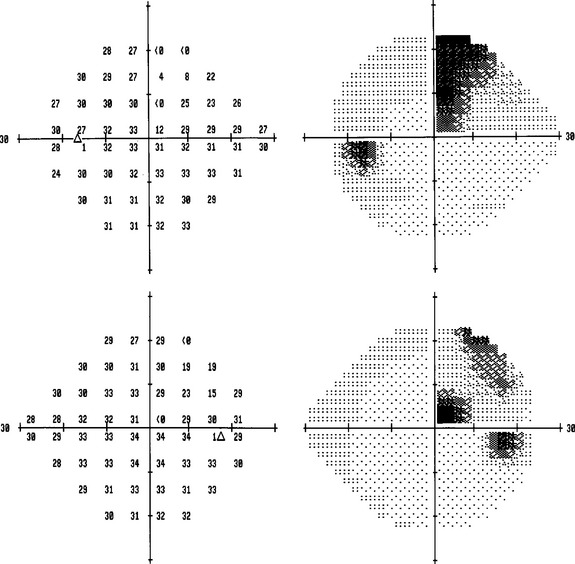
Figure 21-3 Upper quadrantinopia due to a left temporal infarction, left, upper field; right, lower field.
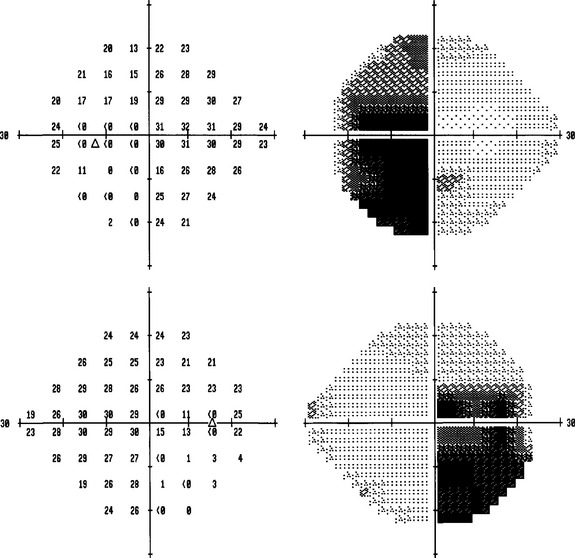
Figure 21-5 Bitemporal hemianopia due to a craniopharyngioma, left, upper field; right, lower field.
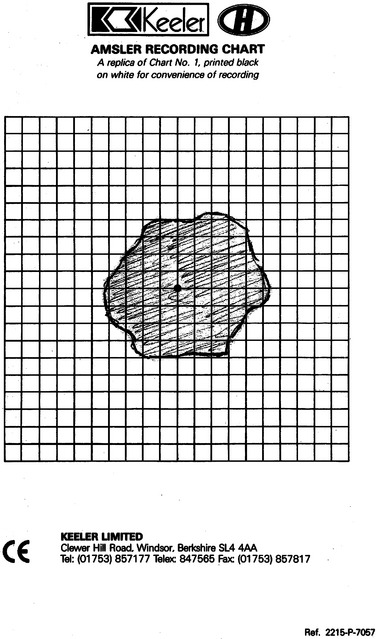
The Amsler grid is useful for plotting central field distortions, such as macular disorders, but also very small central field abnormalities due to, for example, optic neuropathy. The patient plots out the abnormality on the grid himself (Fig. 21-9).
PUPILS
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree