Fig. 1
A 63-year-old woman with vertigo: (a) MRI discovery of a large (18 mm) MCA aneurysm; (b) pre-operative angiography showing a large aneurysm on the MCA trifurcation (1 frontal and 2 temporal branches); (c) post-operative CT scan; (d) post-operative angiography showing complete exclusion of the aneurysms with multiple clips. Upon discharge, the patient showed a transient hemiparesis (36 h), without deficits
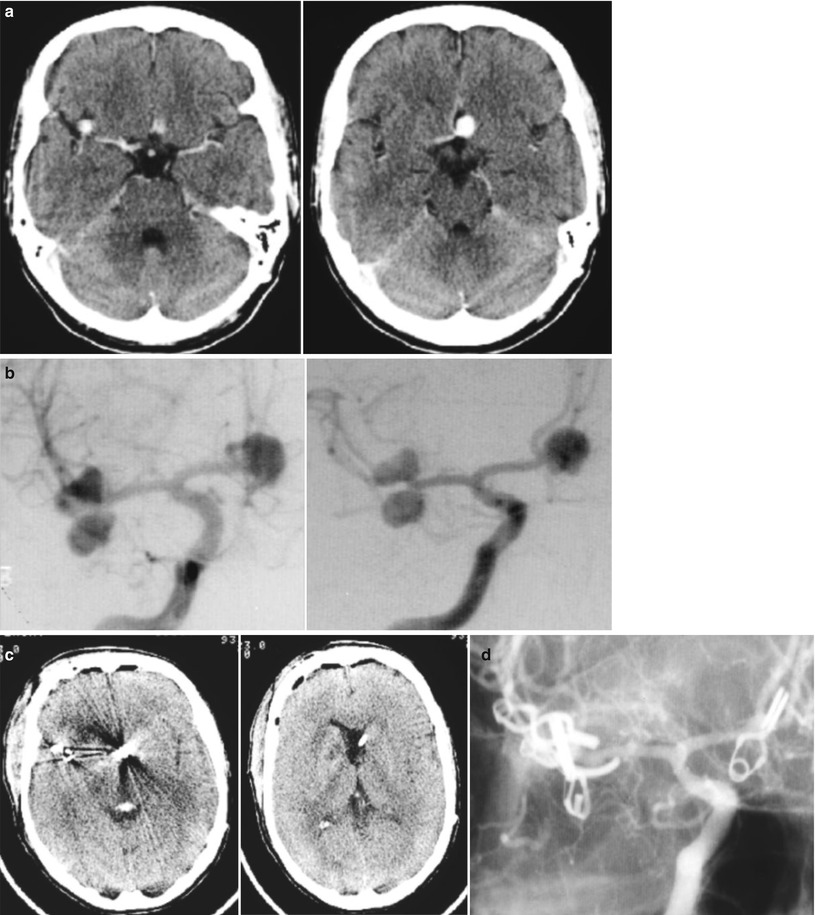
Fig. 2
A 39-year-old woman submitted to VP shunt 11 years earlier: (a) CT scan with evidence of multiple aneurysms; (b) pre-operative angiography, showing two MCA aneurysms and an ACoA aneurysm; (c) post-operative CT scan after exclusion of all aneurysms in one stage; (d) post-operative angiography showing complete exclusion of all aneurysms. Upon discharge, the patient showed transient confusion in the post-operative period, without deficits
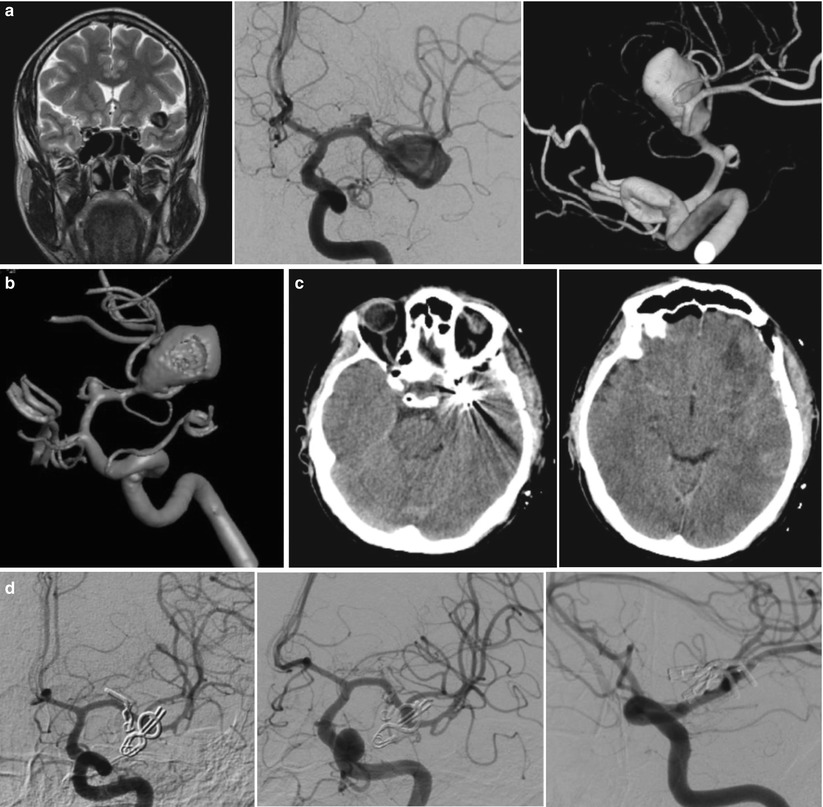
Fig. 3
A 55-year-old man with headache and family history of aneurysms: (a) MR coronal T2 weighted image showing a large MCA aneurysm; (b) pre-operative angiography with 3D reconstruction, showing a large (18 mm) aneurysm of left MCA division and a small aneurysm on the ipsilateral M1 tract; (c) post-operative CT scan; (d) post-operative angiography, showing complete exclusion of the aneurysms. The patient did not show post-operative deficits
One hundred and twenty-four patients underwent aneurysm exclusion by clip; in 2 patients, only a wrapping was performed. During surgery, intraoperative flowmetry was applied in order to avoid inadvertent occlusion or stenosis of parent vessels, and temporary proximal vessel occlusion was used in order to obtain a safer manipulation of the aneurysm before the positioning of a definitive clip. On the whole, an intraoperative measurement of flow was obtained in 78 patients; the mean flow recorded (± SD) was 39.2 ± 16.0 ml/min on the M1 tract, 21.0 ± 10.6 ml/min on the M2 branches, and 13.5 ± 5.6 ml/min on the M3 branches. As regards temporary occlusion, this was divided into two modalities – intermittent and continuous – according to a previous classification of our group [8]. A total of 57 patients underwent temporary occlusion, which was continuous in 34 patients (59 %) and intermittent in 23 (41 %), with a total of 8 occlusions lasting ≥ 10 min (Table 1). All patients underwent post-operative angiography in order to confirm the complete obliteration of the aneurysm.
Table 1
Temporary clipping (57 patients): occlusion period versus modality of afferent vessel occlusion
Occlusion modality | Total | ||
|---|---|---|---|
Continuous | Intermittent | ||
<5 min | 18 (31 %) | 5 (9 %) | 23 (40 %) |
5–9 min | 14 (25 %) | 12 (21 %) | 26 (46 %) |
≥10 min | 2 (3 %) | 6 (11 %) | 8 (14 %) |
The clinical outcome was evaluated at 6 months according to the modified Rankin Scale (mRS), and a statistical analysis was done using the chi-square test and the Fisher exact test if the sample size was too small.
Results
Following surgery, neurological deficits were reported in 5 patients (8 %) out of the 57 who underwent temporary vessel occlusion (Table 2); of these, 2 experienced a transient deficit, while 3 patients experienced a permanent deficit, with hemianopsia in 1 case and hemiparesis in 2 cases; in three of the patients with a permanent deficit, occlusion of an efferent vessel was demonstrated on post-operative angiography. Hemorrhage due to reperfusion was seen in 3 patients (5 %) – in 2 cases (with hemorrhage size ≈ 1 cm) without symptoms and in 1 case (with hemorrhage ≈ 2.5 cm) with transient symptoms (Table 2). On the whole, 49 patients were subjected to temporary occlusion for <10 min, and of these, 2 (4 %) experienced symptomatic stroke; conversely, 8 patients were subjected to temporary occlusion for ≥10 min and 3 of them (37 %) experienced a symptomatic stroke. Therefore, the duration of occlusion ≥10 min carries a significantly higher risk of symptomatic stroke (p = 0.01).
Table 2
Temporary clipping (57 patients): relation between temporary occlusion and post-operative morbidity
Transient deficit | Permanent deficit | |
|---|---|---|
Ischemic symptoms (5 cases) | 2 (occlusion times 5 and 12 min) | 3a (occlusion times 7, 19, 21 min) |
Hemorrhage due to reperfusion (3 cases) | 1 (occlusion time 9 min) | – |
During intraoperative flowmetry, the following was seen in a small number of patients: (1) redistribution of flow on the MCA division branches, with significant decrease in the flow in one branch (generally in the temporal one) and an increase in the other branch; and (2) post-occlusive hyperemia on M1 tract and M2 branches after temporary clipping, with an average two-fold increase of flow immediately after removal of the temporary clip.
The clinical outcome is shown in Table 3. Of the 126 patients operated on for unruptured MCA aneurysm, 115 did not show pre-existing neurological deficits; in this subgroup, 8 (7 %) showed post-operative disability, which was severe (mRS > 3) in 4 cases (3.5 %); one patient died due to severe coagulopathy. In the group of patients with pre-existing deficits (11 cases), 7 (64 %) showed a moderate disability, and 4 (36 %) a significant disability after surgery. In patients without pre-existing deficits, the clinical outcome was also related to the size of the aneurysm (Table 4); on the whole, an unfavorable result was reported in 3 cases (3.1 %), with small or standard-size aneurysms, and in 2 cases (11.7 %) with large or giant aneurysms.
Table 3
Clinical outcome (modified Rankin scale) according to clinical presentation
Presentation | mRS | |||||
|---|---|---|---|---|---|---|
0 | 1 | 2 | 3 | 4 | Death | |
No deficit (115 cases) | 106 (92 %) | 4 (3.5 %) | – | 2 (1.8 %) | 2 (1.8 %) | 1a (0.9 %) |
Pre-existing disability (11 cases) | – | 6 (54 %) | 1 (9 %) | 1 (9 %) | 3 (28 %) | – |
Total (126 cases) | 106 (84 %) | 10 (8 %) | 1 (0.8 %) | 3 (2.2 %) | 5 (4.2 %) | 1a (0,8 %) |
Table 4




Clinical outcome (modified Rankin scale) according to aneurysmal size, in 115 patients without pre-existing disability
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








