Chapter 12 Facet (Zygapophyseal) Intraarticular Joint Injections
Cervical, Lumbar, and Thoracic
 Facet arthropathy is a significant contributor to spinal pain in the cervical, thoracic, and lumbar regions.
Facet arthropathy is a significant contributor to spinal pain in the cervical, thoracic, and lumbar regions. Intraarticular injection or medial branch block with a small volume of local anesthetic play a critical role in establishing the diagnosis because no radiographic modality, historical, or physical exam finding has proven reliable.
Intraarticular injection or medial branch block with a small volume of local anesthetic play a critical role in establishing the diagnosis because no radiographic modality, historical, or physical exam finding has proven reliable. Recent guideline statements suggested dual controlled comparative medial branch blocks with subsequent radiofrequency ablation have better evidence for outcomes, although intrarticular joint injections are more appropriate in patients who are not good candidates for radiofrequency procedures.
Recent guideline statements suggested dual controlled comparative medial branch blocks with subsequent radiofrequency ablation have better evidence for outcomes, although intrarticular joint injections are more appropriate in patients who are not good candidates for radiofrequency procedures. The specificity of diagnostic intraarticular facet injection may be increased by limiting the use of intravenous sedatives or opioids and local anesthetics for anesthesia of the needle tracks.
The specificity of diagnostic intraarticular facet injection may be increased by limiting the use of intravenous sedatives or opioids and local anesthetics for anesthesia of the needle tracks. The volume of intraarticular injection should be limited to 0.5 mL for cervical and thoracic facets and 1 mL for lumbar facets, as the cervical, thoracic, and lumbar facets can accommodate 0.5 to 1 mL, 0.75 mL, and 1.0 to 1.5 mL volume.
The volume of intraarticular injection should be limited to 0.5 mL for cervical and thoracic facets and 1 mL for lumbar facets, as the cervical, thoracic, and lumbar facets can accommodate 0.5 to 1 mL, 0.75 mL, and 1.0 to 1.5 mL volume. A reduction in concordant pain of >50% is as reliable as a >80% pain reduction in predicting therapeutic outcomes.
A reduction in concordant pain of >50% is as reliable as a >80% pain reduction in predicting therapeutic outcomes. When a steroid is used in the cervical region for therapeutic purpose, a nonparticulate injectate is recommended to avoid vascular embolization.
When a steroid is used in the cervical region for therapeutic purpose, a nonparticulate injectate is recommended to avoid vascular embolization. Lateral approach for cervical facet injection in decubitus position is easier to perform and better tolerated by patients. However, caution should be exercised to avoid parallax of fluoroscopy images at the level of injection in order to focus on the appropriate side of injection.
Lateral approach for cervical facet injection in decubitus position is easier to perform and better tolerated by patients. However, caution should be exercised to avoid parallax of fluoroscopy images at the level of injection in order to focus on the appropriate side of injection. For thoracic facet injection, careful, incremental, and measured correction and advancement of the needle should be performed to minimize the risk of pneumothorax and subarachnoid injection.
For thoracic facet injection, careful, incremental, and measured correction and advancement of the needle should be performed to minimize the risk of pneumothorax and subarachnoid injection.Introduction
Spinal pain is extremely common. The incidences of pain in the neck, thoracic, and low back are estimated at 44%, 15%, and 56%, respectively, in the general population.1 Facet arthropathy is an important source of spinal pain, and facet interventions are the second most common procedure performed in the United States by pain physicians, behind epidural steroid injections. This chapter focuses on the intraarticular injections of facet joints between vertebrae C2 through S1 for diagnostic and therapeutic purposes. The injection of the atlanto-axial joint (AAJ) between vertebrae C1-C2 is discussed elsewhere.
Prevalence of Facet Joint Pain
Estimates of lumbar facetogenic pain vary, from 15% of all back pain complaints2 to 59.6% males and 66.7% females in the community based on a population study.3 The prevalence of lumbar facetogenic pain, determined by placebo-controlled diagnostic blocks using a criterion of 90% pain reduction, ranges from 27% to 40% in patients with axial low back pain.4,5 Sedation may increase false-positive rates of diagnostic blocks by 10%, but psychological comorbidity has not been shown to affect the diagnostic accuracy. Aging is positively related to the prevalence of lumbar facet arthropathy, with an occurrence of 89% in individuals 60 to 69 years old. The most common level is at L4-L5.2
The prevalence of thoracic facet pain ranges between 33% and 48% with a 95% confidence interval based on responses to comparative controlled diagnostic blocks.6 The prevalence of cervical facet pain is 30% to 70% of cases7–9 and is not significantly affected by prior surgery, psychopathology, or age. The most commonly affected facet is C4-C5 (14.62%) followed by C3-C4, C2-C3, C5-C6, and C6-C7, respectively.10 There is no proven correlation between clinical manifestation of facetogenic pain and facet arthrosis shown by imaging studies or cadaveric observations. Diagnostic block remains the best available tool to identify facetogenic pain despite its high false-positive rates (39% to 53%).
Establishing Diagnosis
Numerous studies have attempted to determine the historical, or physical, and radiographic findings that correlate with pain associated with facet arthropathy. None has been proven specific, sensitive, and reliable.2 Consequently, diagnosis is primarily based on pain reduction and mobility improvement in response to controlled diagnostic facet blocks.4,6,11 The diagnosis of facetogenic pain is suggested by controlled comparative (lidocaine/bupivacaine) medial branch blocks. A criterion of 80% pain reduction and the ability to perform maneuvers that were painful before the diagnostic intervention are commonly used. However, a recent study suggests that using 50% pain reduction as a criterion for positive diagnostic block is just as effective as using 80% pain reduction in predicting the outcomes of medial branch radiofrequency ablation.12
Even though facetogenic pain is primarily determined by diagnostic blocks, clinical findings from history and physical examinations usually help physicians decide if diagnostic facet blocks are warranted. For example, pain from the AAJ is typically provoked by head rotation with the neck slightly flexed forward. This information may lead to an AAJ block rather than a cervical facet block. Therefore, taking the patient history and performing a physical examination is still an indispensable step in establishing a diagnosis of facet pain. Pain referral patterns for cervical and thoracic facet pain have been generated,2,13–15 as shown in Fig. 12-1.
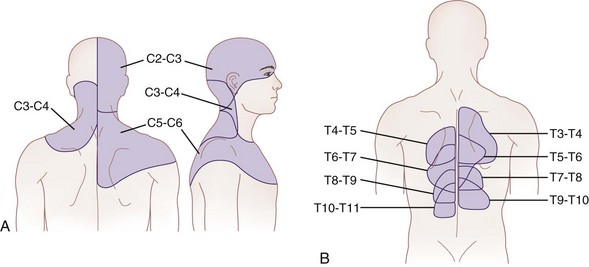
Fig. 12-1 Maps of referred pain from the cervical (A) and thoracic (B) facets.
(Part A adapted from Bogduk N, Marland A: The cervical zygapophysial joints as a source of neck pain, Spine 13:610-617, 1988; part B adapted from Dreyfuss P, Tibiletti C, Dreyer SJ: Thoracic zygapophyseal joint pain patterns: a study in normal volunteers, Spine 19:807-811, 1994.)
Cervical Facet Pain
Restricted range of motion is not pathognomonic for facet pain and can present in a variety of neck disorders, such as whiplash injury. Point tenderness was recently evaluated in 33 patients by assessing pain pressure thresholds in symptomatic and asymptomatic facets joints.16 Although the pain pressure thresholds are significantly lower in patients with neck pain, this approach is not diagnostic for cervical facet joint pain. Neck point tenderness can be indicative of myofascial pain or associated with tension headache.17 No provocative tests tend to produce pain in the referral patterns. As a general rule, the upper facet joints may cause headache, and the lower joints may have pain referred to the shoulder in a nondermatomal distribution. Cervical radicular pain is usually absent.
Thoracic Facet Pain
Pain from thoracic facet joints may be provoked by facet capsule distention,14 such as extension, lateral bending, and twisting or paraspinal pressure overlying the facet joints. Pain is often nonradicular, and there is no associated weakness.
Lumbar Facet Pain
Lumbar facet joint pain is typically described as back pain with or without nondermatomal leg pain above the knee. Paraspinal tenderness overlying the facets produced by pressure is suggestive.18 Facet pain is typically not confined to a dermatomal distribution (nonradicular). Motor function and reflex assessment are usually intact.
Anatomy of the Facet Joints
The facet joints have rich innervation, including encapsulated, unencapsulated, and free nerve endings.2 These innervations provide nociception through C and A-δ afferents as well as proprioception through low-threshold, rapidly adapting mechanoreceptors.19 Immunocytochemistry of facet joints demonstrated the presence of substance P, calcitonin-gene-related peptide, and neuropeptide Y, suggesting pain transmission and sympathetic fibers.20–22 Facet joint distraction in rats produces spinal astrocyte activation and persistent mechanical allodynia.23 The expression of a binding protein BiP, also known as growth-related protein 78, is upregulated 2.1-fold in the dorsal root ganglion after painful distraction injury to the rat C6-C7 facet, indicating neuronal stress activation.24 Cytokines and neurotrophic factors are upregulated in dorsal root ganglion neurons in models of facet joint inflammation.25–28
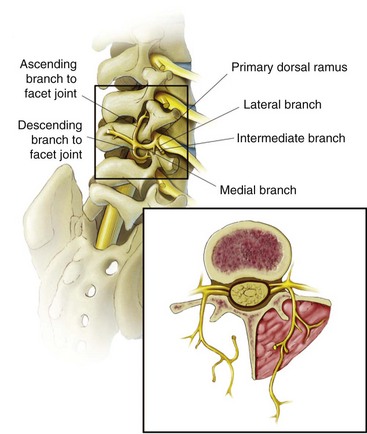
The architecture and orientation of the facet joint vary with function and position along the vertebral column.29–31 The lumbar facet joint can accommodate an average of 1 to 1.5 mL fluid. The joint is C shaped and is encased posteriorly in a fibrous capsule of approximately 1 mm thick composed of collagenous tissue. The lumbar facet joint is supported posteriorly by multifidus muscle, superiorly and inferiorly by fibroadipose menisci forming subcapsular recesses, and anteriorly by the ligamentum flavum.31 The inferior portion of the joint is larger than the superior portion. Any given facet joint has dual innervation from two segmental medial branch nerves: one arising at the given level and one from one segment above as shown in Fig. 12-2. Consequently, a given medial branch nerve innervates two facet joints, the ascending branch to the caudal portion of the facet above and the descending branch to superior portion of the facet below. For example, the L3 medial branch nerve courses along the junction of the superior articular process and the transverse process of L4 under the mamilloaccessory ligament, supplying the caudal portion of the ipsilateral L3-L4 facet joint, and then courses caudally to supply the ipsilateral superior portion of the L4-L5 facet joint. Conversely, the L3-L4 facet has dual innervation from the L2 and L3 medial branches.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree