Chapter 10 Peripheral Applications of Ultrasonography for Chronic Pain
 Applying ultrasonography for injection of peripheral structures in chronic pain is a very useful technique because it offers an affordable and portable device that provides visualization of the target structures.
Applying ultrasonography for injection of peripheral structures in chronic pain is a very useful technique because it offers an affordable and portable device that provides visualization of the target structures. In contrast, fluoroscopy is not designed to visualize various soft tissues in the injection of the peripheral structures.
In contrast, fluoroscopy is not designed to visualize various soft tissues in the injection of the peripheral structures. Ultrasound-guided injections of peripheral structures have mostly been validated in the literature, showing with high accuracy in reaching the target structures, in contrast to the poor location of target structures with conventional landmark-based techniques.
Ultrasound-guided injections of peripheral structures have mostly been validated in the literature, showing with high accuracy in reaching the target structures, in contrast to the poor location of target structures with conventional landmark-based techniques. The ideal injection site for the SSN is along the course of the nerve between the suprascapular and spinoglenoid notches, where the nerve is contained in a compartment.
The ideal injection site for the SSN is along the course of the nerve between the suprascapular and spinoglenoid notches, where the nerve is contained in a compartment. The risk of pneumothorax with intercostal nerve injection is real because the distance between the intercostal nerve and pleura is usually less than 0.5 cm. The ideal injection site is at the costal angle where the nerve is in between two layers of muscle in the subcostal groove.
The risk of pneumothorax with intercostal nerve injection is real because the distance between the intercostal nerve and pleura is usually less than 0.5 cm. The ideal injection site is at the costal angle where the nerve is in between two layers of muscle in the subcostal groove. Although it is abundantly clear that the course of the IL and IH nerves is highly variable medial to anterior superior iliac spine (ASIS) and is very constant lateral to ASIS, all landmark-based techniques proposed the needle insertion site medial to ASIS with a high failure rate. Ultrasonography allows accurate injection of the IL and IH nerves lateral to the ASIS.
Although it is abundantly clear that the course of the IL and IH nerves is highly variable medial to anterior superior iliac spine (ASIS) and is very constant lateral to ASIS, all landmark-based techniques proposed the needle insertion site medial to ASIS with a high failure rate. Ultrasonography allows accurate injection of the IL and IH nerves lateral to the ASIS. The course of GF nerve is highly variable, but the genital branch consistently transverses the inguinal canal. Ultrasonography can accurately locate the inguinal canal and the spermatic cord, allowing blockade of the genital branch of GF nerve.
The course of GF nerve is highly variable, but the genital branch consistently transverses the inguinal canal. Ultrasonography can accurately locate the inguinal canal and the spermatic cord, allowing blockade of the genital branch of GF nerve. The lateral femoral cutaneous nerve is a small peripheral nerve with a variable course in the infrainguinal region. Experience is required to locate this nerve with ultrasonography.
The lateral femoral cutaneous nerve is a small peripheral nerve with a variable course in the infrainguinal region. Experience is required to locate this nerve with ultrasonography. Pudendal nerve blockade at the ischial spine level can be achieved either by CT scan or ultrasonography with the visualization of the interligamentous plane; a fluoroscopy-guided technique relies on the surrogate landmark, the ischial spine.
Pudendal nerve blockade at the ischial spine level can be achieved either by CT scan or ultrasonography with the visualization of the interligamentous plane; a fluoroscopy-guided technique relies on the surrogate landmark, the ischial spine.Introduction
Application of ultrasonography in pain medicine (USPM) is a rapidly growing medical field in interventional pain management. It is evidenced by the remarkable increase in the publication of literature on ultrasound-guided injection1 and the remarkable increase in the number of USPM workshops held in the past 3 years in North America, Europe, and Asia.
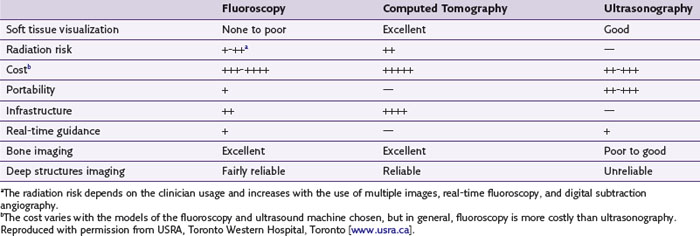
Traditionally, interventional procedures for pain management are performed either by a landmark-based technique or with imaging guidance such as fluoroscopy and computed tomography (CT) scanning. A comparison of the advantages and disadvantages of various imaging equipment is summarized in Table 10-1. Based on the target structures, the application of USPM can be classified into three areas: peripheral, axial, and musculoskeletal (Table 10-2). Applying ultrasonography for the injection of peripheral structures is particularly useful because it allows the visualization of various soft tissues (nerve, muscle, tendon, or vessels), and most of the interventional pain procedures for peripheral structures are performed without imaging guidance. This chapter reviews the relevant anatomy, sonoanatomy, and the injection techniques of a few peripheral structures.
Suprascapular Nerve
First described in 1941,2 suprascapular nerve (SSN) block has been performed over the years by anesthesiologists, rheumatologists, and pain specialists to manage the pain that follows trauma3 or shoulder surgery,4,5 to ameliorate the pain associated with various chronic shoulder pain syndromes (adhesive capsulitis, frozen shoulder, rotator cuff tear, and glenohumeral arthritis),6–9 and to aid in the diagnosis of suprascapular neuropathy.10
Anatomy and Sonoanatomy
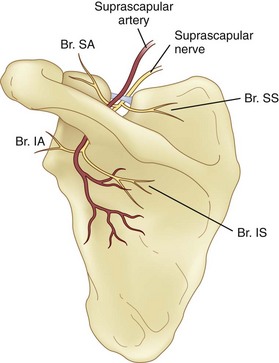
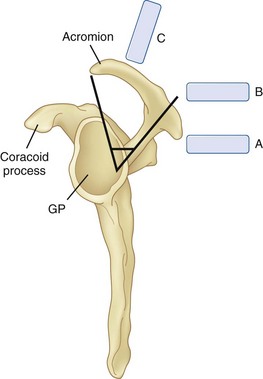
The SSN originates from the superior trunk of the brachial plexus (formed by the union of the fifth and sixth cervical nerves). It then runs parallel to the omohyoid muscle and courses under the trapezius before it passes under the transverse scapular ligament in the suprascapular notch (Fig. 10-1). Entering the suprascapular fossa, the SSN passes beneath the supraspinatus and curves around the lateral border of the spine of the scapula (spinoglenoid notch) to the infraspinatus fossa (Fig. 10-2). In the supraspinatus fossa, it gives off two branches: one to the supraspinatus muscle and another as an articular branch to the shoulder joint; and in the infraspinatus fossa, it gives off branches to the infraspinatus muscle and to the shoulder joint and scapula. The sensory component of the SSN provides fibers to about 70% of the shoulder joint. There is no significant cutaneous branch of this nerve.
The suprascapular notch is located on the superior margin of the scapula and medial to the coracoid process. The size and shape of the notch are highly variable and even absent in up to 8% of cadavers.11 Above the transverse scapular ligament run the suprascapular artery and vein, although rarely, the artery travels along with the SSN through the notch. The suprascapular fossa is bordered by the spine of the scapula dorsally, by the plate of the scapula ventrally, and by the supraspinatus fascia superiorly, forming a classic compartment, the only exit through which is the suprascapular notch.
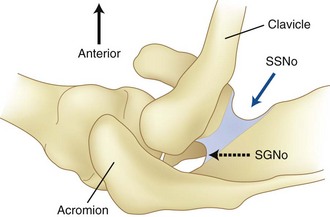
The ideal site to perform the SSN injection is at the floor of the scapular spine between the suprascapular notch and spinoglenoid notch (Fig. 10-2).12 First, this technique is independent of the notch as a target. Thus, it avoids the risk of pneumothorax if one considers the direction of the needle. This technique is also feasible in individuals without a suprascapular notch (8% of the population). Second, the suprascapular fossa forms a compartment and retains the local anesthetic around the nerve with a small volume.13 In contrast, depositing local anesthetic at the notch level will potentially result in the spread of local anesthetic to the brachial plexus.13 Third, although imaging the suprascapular notch is possible, advancing the needle perfectly in plane in this orientation is very challenging (Fig. 10-3). A slight deviation in the anterior direction will direct the needle toward the thorax.
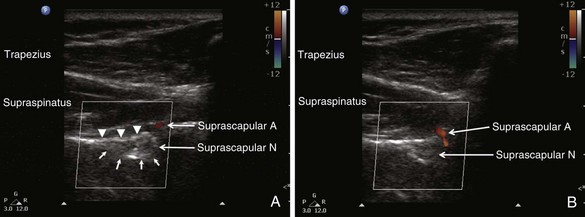
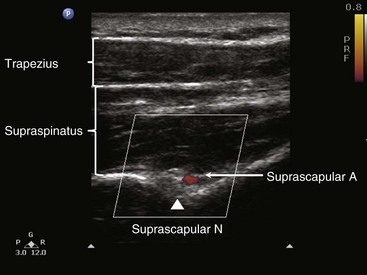
When imaging the suprascapular fossa with ultrasonography, the two key muscles in the scan are trapezius and supraspinatus muscles (Fig. 10-4). The SSN is often seen accompanied by the suprascapular artery on the floor of the scapular spine between the suprascapular notch and spinoglenoid notch (Fig. 10-5). The scapula spine forms an angle (39.5 degrees ± 5.8 degrees) to the axis of the scapula blade,14 so the orientation of the ultrasonography probe should be closer to the coronal plane to visualize the contents of the suprascapular fossa (Fig. 10-6).
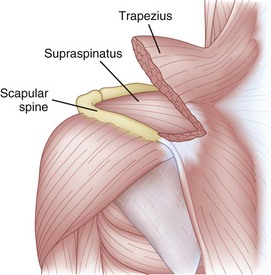
Fig. 10-4 Left shoulder showing the muscle layers in the suprascapular fossa.
(Modified with permission from USRA, Toronto Western Hospital, Toronto [www.usra.ca].)
Existing Techniques
Various approaches have been described. In general, the targets for the SSN are either at the suprascapular notch itself or in the suprascapular fossa.1 To direct the needle to these targets, various methods have been used, including a “blind” insertion using various landmarks,2 a peripheral nerve stimulator3 or electromyography,7 and a direct insertion using fluoroscopic15 or CT scan guidance.16
There are a few disadvantages to targeting the SSN at the notch using the blind or landmark-guided approach, including the risk of pneumothorax, intravascular injection, and nerve injury.17 In an attempt to evaluate needle tip placement radiologically following a “blind” needle placement, Brown et al18 demonstrated that the proximity of the “needle tip-to-notch” was poor. The precision of the needle tip location can be improved by fluoroscopy or CT scan guidance. Placing the needle into the suprascapular fossa is a popular alternative.13 The technique is easy to perform and further minimizes the risk of pneumothorax because of the direction of the needle. To ensure that the SSN is blocked, an adequate volume of solution is injected into the suprascapular fossa compartment. A recent CT scan study showed that 10-mL injectate spread to the brachial plexus in the axilla in three of 33 cadavers.13 They also showed that blind injection could lead to placement of the needle in or even above the supraspinatus muscle.
Four articles described the sonoanatomy of the SSN relevant to the nerve injection.12,19–21 Most of them19–21 described the visualization of the suprascapular notch, transverse scapular ligament, and suprascapular artery and nerve. The ultrasound probe was placed in the suprascapular fossa in the long axis of supraspinatus muscle. According to some authors19,20 the ultrasound image showed the suprascapular notch (as a curved continuous hyperechoic line), transverse scapular ligament, and SSN. A correlation study with fluoroscopy and cadaver dissection suggested the site of injection was actually at the suprascapular fossa between the suprascapular notch and spinoglenoid notch (Fig. 10-2).12
Ultrasound-Guided Injection Technique
With the patient in sitting or prone position, ultrasound scanning is performed with a linear ultrasound probe (7-13 MHz) placed in a coronal plane over the suprascapular fossa with a slight anterior tilt. The probe is place in an orientation such that it is in the short axis to the line joining medial aspect of the coracoid process (approximating the suprascapular notch) and posterior aspect of the acromion (reflecting the position of the spinoglenoid notch). The supraspinatus and trapezius muscles and the bony fossa underneath them should come into view (Fig. 10-5). By adjusting the angle of the ultrasound probe in a cephalocaudad direction, the SSN and artery should be brought into view in the trough of the floor (Fig. 10-5). The nerve can sometimes be difficult to visualize because of the orientation. A 22-gauge, 80-mm needle is inserted in plane from the medial aspect of the probe because of the presence of the acromion process on the lateral side. Because of the proximity of the nerve, an injectate volume of 5 to 8 mL is usually sufficient.
Clinical Pearls and Pitfalls
 One should avoid scanning the SSN at the suprascapular notch because (1) it is challenging to obtain the narrow plane of the suprascapular notch and to guide the needle to this target and (2) there is the risk that injectate will spill outside the notch to the brachial plexus.
One should avoid scanning the SSN at the suprascapular notch because (1) it is challenging to obtain the narrow plane of the suprascapular notch and to guide the needle to this target and (2) there is the risk that injectate will spill outside the notch to the brachial plexus.Intercostal Nerve
The intercostal nerves (ICNs) supply skin and musculature of chest and abdominal wall. Blockade of ICNs has been in clinical use for decades for treatment of acute and chronic pain conditions affecting the thorax and upper abdomen.22 ICN blockade provides excellent analgesia for pain from rib fractures23 and from chest and upper abdominal surgery.24 Neuroablation of ICN may be used to manage chronic pain conditions such as postmastectomy and postthoracotomy pain.25–28
Anatomy and Sonoanatomy
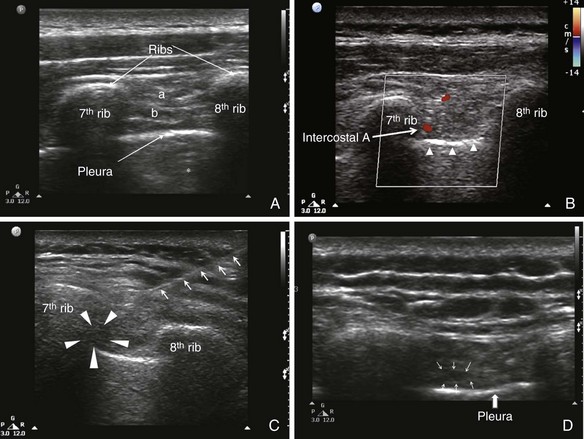
The ICNs are the ventral rami of the 12 thoracic nerves (Fig. 10-7, A). After exiting from the spine, the ICNs are located between the pleura and the internal intercostal membrane and subsequently traverse the membrane. Between costal tubercles and costal angles, the ICNs lie between the external intercostal muscle and internal intercostal membrane, which are immediately adjacent to the parietal pleura. The course of ICNs for that distance really deserves their name “intercostal” nerve (or “in between ribs”). From the costal angle onward, the ICNs run deep to the subcostal groove within the internal intercostal muscles, thus creating an innermost muscular layer known as the innermost intercostals muscle (Fig. 10-7, B).29,30 Readers should be aware that in some anatomy textbooks, the ICNs are described to situate in between the two layers of internal intercostal muscle. The ICNs travel in the costal groove accompanied by intercostal vein and artery and the neurovascular bundle is arranged from above downwards in the manner: “V-A-N” (Fig. 10-8). At a distance about 5 to 8 cm anterior to the angle of the rib, the groove ends and blends into the surface of the lower edge of the rib. The lateral cutaneous branch of the ICN, which supplies the skin of the chest, branches off and pierces the external intercostal muscle in the region between the posterior and mid-axillary line. As the ICN approaches the midline anteriorly, it pierces the overlying muscles and skin to terminate as the anterior cutaneous branch (Fig. 10-7, A).
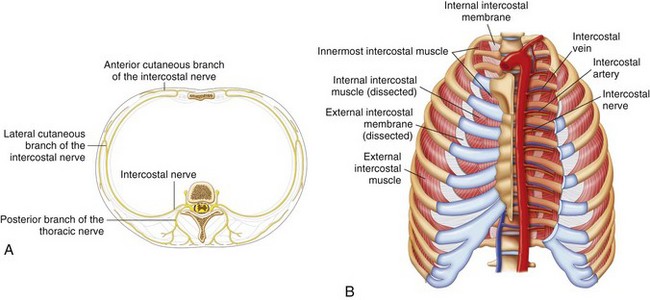
Fig. 10-7 A, Branches of the typical intercostal nerves. B, Intercostal muscles in the chest wall.
(Reprinted with permission from USRA, Toronto Western Hospital, Toronto [www.usra.ca].)
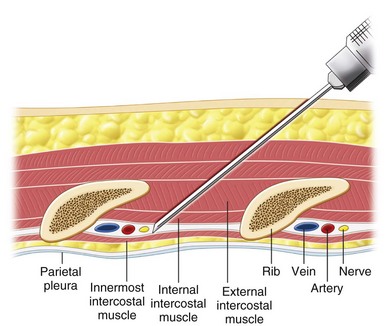
Fig 10-8 Cross section of chest wall showing intercostal muscles and neurovascular bundles.
(Reprinted with permission from USRA, Toronto Western Hospital, Toronto [www.usra.ca].)
Under ultrasound scanning, different layers of the intercostal muscles and the pleura can be visualized (Fig. 10-9). The pleura appear as a definite hyperechogenic line that glides with respiratory movement. Normally, two types of artifacts can be visualized: reverberation artifacts appearing as a series of horizontal lines parallel to the pleural interface and vertical comet tail artifacts. The neurovascular bundle cannot be visualized under normal circumstances because it is covered by the rib except in the region between costal tubercles to costal angle. However, the location of the ICN can be estimated by directing the needle in between the internal and innermost intercostal muscle.
Existing Techniques
The classic landmark-based technique is performed with the patient in the sitting position. The ICN block is usually performed at the angle of the rib to ensure that the tissues innervated by the lateral cutaneous nerve are blocked. The most feared complication with the existing “blind” technique is pneumothorax. The distance between the neurovascular bundles to the pleura in thin patients is usually within 0.5 cm.26 The injection is performed after negative aspiration for air and blood, but this maneuver cannot reliably prevent pneumothorax or hemothorax . The incidence of pneumothorax ranges anywhere from 0.09% to 8.7%.22,31,32
The fluoroscopic technique is performed with the patient in the prone position. The appropriate rib is identified under fluoroscopic anteroposterior (AP) view, and the needle is introduced in the inferior margin of the rib. After negative aspiration, a contrast injection is performed to ensure appropriate spread before injection.27 This technique does not theoretically minimize the risk of pneumothorax because the pleura cannot be visualized with fluoroscopy.
The use of ultrasound guidance for intercostal block was recommended from the personal experiences in two reviews.1,33 Either the in-plane or out-of-plane technique was recommended. However, both reviews emphasized hydrodissection to ensure the visualization of the needle tip. A small case series also confirmed the feasibility and technical advantages of ultrasound-guided cryoablation of the ICNs in four patients with postthoracotomy pain syndrome.26
Ultrasound-Guided Injection Technique
The patient is in the prone position, and a linear probe (7-13 MHz) is ideal for the superficial structures. The site is at the costal angle (≈7 cm from the midline). Both the in-plane and out-of-plane technique can be used. The authors prefer the in-plane technique because the direction of the needle is similar to the classical technique described for ICN block, and the complete needle path can be traced.1 The needle entry site is the upper margin of the rib one level caudal to the targeted ICNs. After the needle penetrates the skin, the ultrasound probe can be rolled over the needle, which is advanced deep to the internal intercostal muscle. One of the drawbacks for the in-plane technique is that when the probe is not perfectly in line with the needle, the practitioner may have a false impression of the location of the needle tip. Because the distance between the costal groove and the pleura is in the dimension of 0.5 cm, it is advisable to inject a small amount of injectate when the needle is in the external intercostal muscle to confirm the needle tip position. Under real-time injection, intravascular injection should be suspected if the spread of the medication is not visualized. After the needle tip is confirmed deep to the internal intercostal muscle, the local anesthetic can be injected, and spread of medication can be seen.
Clinical Pearls and Pitfalls
 The course of ICNs is “intercostal” from the costal tubercle to costal angle (i.e., between the ribs). Although one can locate the intercostal artery and thus the neurovascular bundle, the ICNs are adjacent to the parietal pleura. Injection at this site is recommended only for very experienced practitioners. The author recommends the injection site at the costal angle.
The course of ICNs is “intercostal” from the costal tubercle to costal angle (i.e., between the ribs). Although one can locate the intercostal artery and thus the neurovascular bundle, the ICNs are adjacent to the parietal pleura. Injection at this site is recommended only for very experienced practitioners. The author recommends the injection site at the costal angle.Ilioinguinal, Iliohypogastric, and Genitofemoral Nerves (Border Nerves)
The ilioinguinal (IL), iliohypogastric (IH), and genitofemoral (GF) nerves are the primary nerves providing sensory innervation to the skin bordering between the thigh and abdomen. Therefore, they are also called border nerves collectively.1 Injury to the IL and IH nerves is a known risk in open appendectomy incisions, postinguinal herniorrhaphy, low transverse incisions (e.g., Pfannenstiel incision), and during trocar insertion for laparoscopic surgery of the abdomen and pelvis.34–38 Patients with neuropathy after injury to these nerves present with groin pain that may extend to the scrotum or the testicle in men, the labia majora in women, and the medial aspect of the thigh. Accurate diagnostic block of those nerves is important in understanding the etiology of the clinical problem.
Anatomy and Sonoanatomy
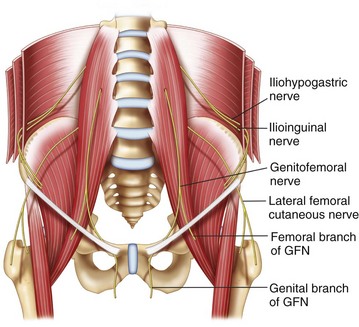
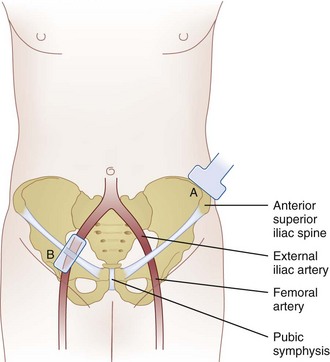
The IL and IH nerves originate from the T12 and L1 nerve roots. Emerging near the lateral border of the psoas major muscle, the nerves extend diagonally toward the crest of the ilium (Fig. 10-10).
The IH nerve pierces the transversus abdominis muscle above the iliac crest midway between the iliac crest and the twelfth rib. The IL nerve runs caudally and parallel to the IH nerve. Here, both nerves can be found consistently (90%) between the transversus abdominis and internal oblique muscles.39 Terminal branches of the IH nerve perforate the external oblique muscle aponeurosis 4 cm lateral to the midline to supply the skin over the lower portion of the rectus abdominis.40 The IH nerve also provides sensory innervation to the skin above the tensor fasciae lata through a lateral cutaneous branch. Terminal branches of the IL nerve enter the inguinal canal through the deep inguinal ring and may lie upon the cremasteric muscle and fascial layer of the spermatic cord in men or round ligament in women.41,42 This terminal branch is often accompanied by the genital branch of the GF nerve, and wide variations in the course of these nerves within the inguinal canal have been documented.4,8,10,12–14 The terminal sensory branches may innervate the skin of the mons pubis, inner thigh, inguinal crease, and anterior surface of the scrotum or anterior third of the labia.
The GF nerve originates from the first and second lumbar nerve roots (Fig. 10-10). It emerges on the anterior surface of the psoas muscle either a single trunk or separate genital and femoral branches.43 The femoral branch passes laterally over the external iliac artery and then penetrates the fascia lata to enter the femoral sheath. Terminal branches provide cutaneous innervation to the femoral triangle.44 The genital branch also crosses in front of the external iliac artery but then passes through the ventral aspect of the internal ring of the inguinal canal. Anatomical studies describe this branch running between the cremaster and internal spermatic fascia, incorporating with the cremasteric fascia, or lying outside of the spermatic cord.42,44,45 Terminal sensory branches may innervate the scrotum and possibly the upper, inner, and medial thigh.42
Anatomical studies highlight the variability of the IL, IH, and GF nerves. Variations from conventional descriptions have been reported with respect to communication among nerves, penetration of fascial layers, branching patterns, and dominance patterns.1 The most consistent anatomical location for the IL and IH nerves to perforate the abdominal muscular layers is lateral and superior to the anterior superior iliac spine (ASIS), where they run between the transversus abdominis and internal oblique muscular layers.
The recommended area for ultrasound scanning of IL and IH nerves is lateral and superior to the ASIS (Fig. 10-11). At this position, the iliac crest appears as a hyperechoic structure adjacent to which appear the three muscular layers of the abdominal wall (Fig. 10-12). Below the transversus abdominis, peristaltic movements of the bowel may be detected. After the muscular layers have been identified, the II and IH nerves will be found in the split fascial plane between the internal oblique and transversus abdominis muscle layers. Both nerves should be within 1.5 cm of the iliac crest at this site, with the II nerve closer to the iliac crest.46 The nerves are usually in close proximity to each other47 and located on the “upsloping” split fascia close to the iliac crest. In some cases, the nerves may run approximately 1 cm apart. The deep circumflex iliac artery that is close to the two nerves in the same fascial layer can be revealed with the use of color-flow Doppler (Fig. 10-13). A neural structure within the fascial split may also be seen medial and on the flat part of the internal oblique and transversus abdominis muscle junction. This is the subcostal nerve, and if mistaken for the IL and IH nerves, the nerve blockade will result in aberrant distribution of anesthesia.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree