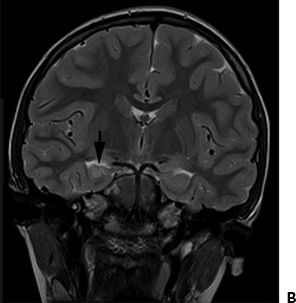
Figure 34.1. Brain MRI of a child that had a 2-hour febrile convulsion. A: Coronal image obtained from brain MRI performed <6 months after febrile status epilepticus. Image shows abnormal high T2 signal in the right hippocampus with slight volume loss. B: Coronal image obtained from brain MRI performed approximately 5 years after febrile status epilepticus. Image shows increased T2 signal intensity within the right hippocampus with associated slight volume loss.
Human Herpes Virus
Human herpes virus 6 (HHV6) is a common childhood infectious agent responsible for roseola infantum and several severe infectious syndromes. In immunocompromized patients, reactivation of viral activity may lead to severe limbic encephalitis. Examination of temporal lobectomy specimens reveals a high incidence of active HHV6B replication in hippocampal astrocytes (46). This association suggests a possible link between early viral infection, complex or prolonged febrile seizures and later HS.
As part of the FEBSTAT study, serum was evaluated for the presence of HHV-6A, HHV-6B, or HHV-7 DNA and RNA (31,47). The study concluded that HHV-6B infection is commonly associated with febrile status epilepticus, and HHV-7 infection is less frequently associated. Together HHV infections were identified in one-third of the febrile status epilepticus subjects (47). The study did not detect HHV-6B or HHV-7 DNA in the CSF of 23 subjects who presented in febrile status epilepticus and had a documented HHV-6B or HHV-7 viremia.
FEBRILE SEIZURES AND NEUROPSYCHOLOGICAL STATUS
The consequences of febrile seizures on later intellectual functioning and behavior of children has been studied extensively. A cohort of 381 children with simple and complex febrile seizures was compared with a control group on measures of academic progress, intelligence, and behavior; there were no differences between groups in any measures (48).
Two large, longitudinal, population-based studies provide strong evidence that febrile seizures do not adversely affect neuropsychological status. Ellenberg and Nelson (49) studied intellectual and academic function following febrile seizures in 431 sibling pairs 7 years of age who were part of the National Collaborative Perinatal Project. Children with febrile seizures and normal intelligence achieved reading and spelling milestones at rates similar to those of their seizure-free siblings. The National Child Development Study, completed in the United Kingdom, also found that children with febrile seizures did not differ from controls in behavior, height, head circumference, or academic achievement (40). It is important to remember that the consequences of febrile seizures can be influenced by seizure duration.
THERAPY
It is accepted that antipyretic agents do not reduce the risk of febrile seizure or seizure recurrence. Prophylactic antiepileptic drug (AED) therapy for febrile seizures should be withheld, as the benefits of treatment do not outweigh the risks. Recurrent febrile seizures and later afebrile epilepsy, which are the major sequelae of a febrile seizure, are both rare. Despite their anxiety, family members should be counseled about the merits of withholding prophylactic treatment.
There are exceptions to the use of AEDs following the occurrence of complex febrile seizures, for example when there is significant risk for later epilepsy. However, even seemingly life-threatening seizures must be evaluated cautiously because neurologic impairment and death are extremely unlikely, even after febrile status epilepticus. The NIH consensus panel found that high-risk patients with two risk factors (e.g., abnormalities on neurologic examination, prolonged focal seizure, and family history of epilepsy) still had only a 13% chance of developing epilepsy. Moreover, although phenobarbital reduced febrile seizure recurrence, there is no firm evidence that the prevention of recurrent febrile seizures diminishes the risk for later epilepsy.
Febrile seizures often cease by the time a child is examined, but prolonged episodes should be treated similar to seizures of any other etiology. A child that is actively having a seizure should receive acute abortive treatment by 5 minutes after seizure onset. All prolonged convulsions carry an increased risk of complications, and treatment should be initiated before 5 minutes after seizure onset to help prevent prolonged seizure activity and consequences. A prolonged FS should be treated promptly by emergency medical services (EMS) or the emergency department. Initially a benzodiazepine should be used, for example rectally administered diazepam gel, but if continued seizure activity a full status epilepticus protocol should be initiated (44).
CONCLUSIONS
Febrile seizures are the most common seizure presentation in infancy and early childhood and are usually benign. Most events are self-limited and carry only a modest risk for febrile seizure recurrence. Febrile seizures are thus a genetically predetermined, age-dependent response to fever and are not classified as epilepsy. Treatment with prophylactic AEDs is not indicated. Febrile status epilepticus is frequently unrecognized and prolonged seizures frequently need medication to terminate the seizure (31). Unfortunately a small percentage of children with prolonged febrile seizures do have long term consequences.
Fewer than 10% of patients with febrile seizures experience severe or recurrent attacks. Risk factors for complex episodes are known, and the likelihood of developing epilepsy remains <5%. Diagnostic procedures or treatment should be performed on an individual basis; febrile status epilepticus must be treated as a medical emergency. Underlying neurologic disorders require investigation, and “epileptic seizures exacerbated by fever” should be distinguished from febrile seizures per se. There is no evidence that prophylactic administration of AEDs prevents the occurrence of later epilepsy.
References
1. National Institutes of Health. Consensus Development Conference on febrile seizures. Proceedings. Epilepsia. 1981;22:377–381.
2. Commission on Epidemiology and Prognosis, International League Against Epilepsy. Guidelines for epidemiologic studies on epilepsy. Epilepsia. 1993;34:592–596.
3. Nelson KB, Ellenberg JH. Prognosis in children with febrile seizures. Pediatrics. 1978;61:720–727.
4. Verity CM, Butler NR, Golding J. Febrile convulsions in a national cohort followed up from birth. I. Prevalence and recurrence in the first five years of life. Br Med J. 1985;290:1307–1310.
5. Tsuboi T. Epidemiology of febrile and afebrile convulsions in children in Japan. Neurology. 1984;34:175–181.
6. Hackett R, Hackett L, Bhakta P. Febrile seizures in a South Indian district: incidence and associations. Dev Med Child Neurol. 1997;39:380–384.
7. Stanhope JM, Brody JA, Brink E, et al. Convulsions among the Chamorro people of Guam, Marianna Islands, Am J Epidemiol. 1972;95:299–304
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








