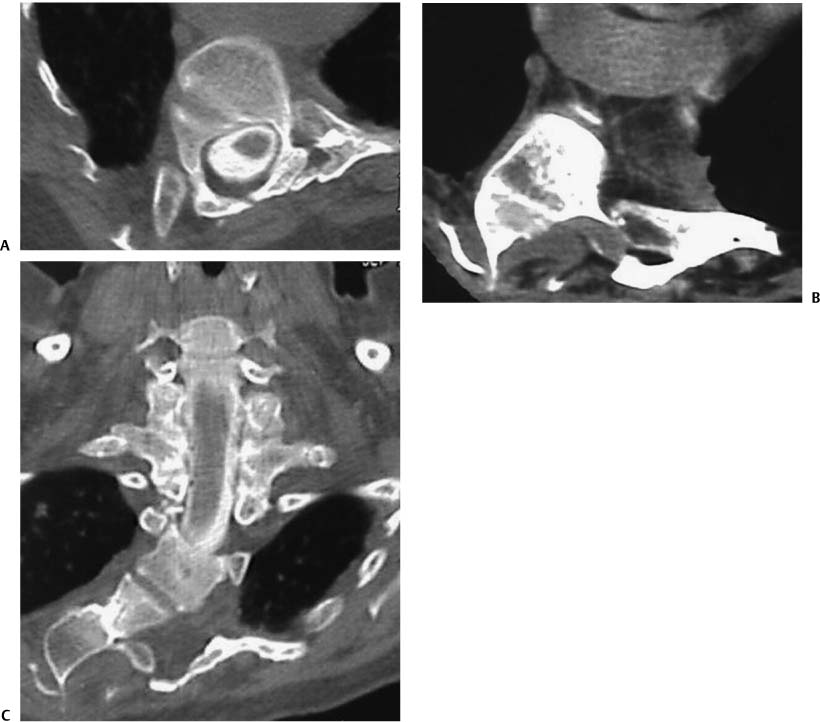
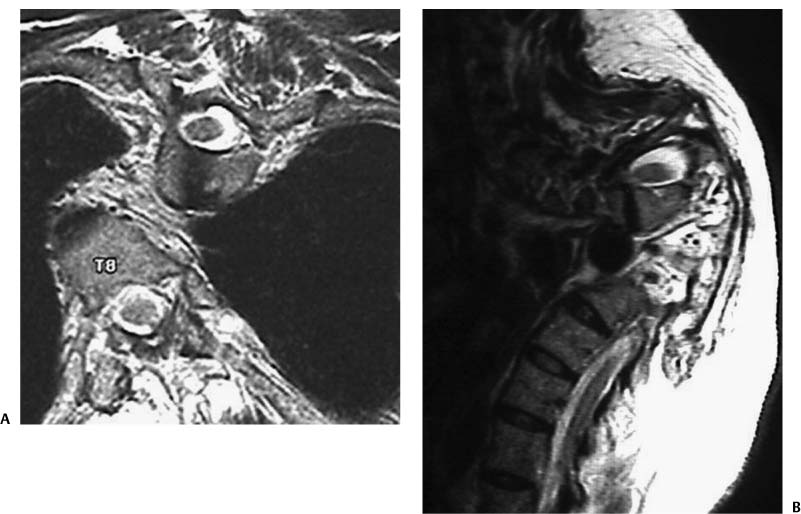
Chapter 9 Historically, Min Mehta wrote an “important decrease of scoliotic curve with supine position is a factor in the successful result for orthopedic treatment.” The management of spinal deformity has gone through a significant evolution in the past decade. The goal of spinal deformity surgery remains to achieve a stable, well-balanced spine centered over the pelvis, fusing as few motion segments as possible. The balanced spine is created by a close interplay of the patient’s spinal anatomy, the biomechanical properties of the spine and its surrounding structures, and the corrective capabilities of surgical techniques and instrumentation. A determination of whether the spinal deformity is fixed or flexible plays a crucial role in the surgical planning and the ultimate type of operative corrective procedure that is selected. Duval-Beau-pere and associates assessed factors contributing to the flexibility of neuromuscular scoliosis,1 and they demonstrated that flexibility included two very different and noncorrelated phenomena: the collapse and the reducibility of the structural curve. They differentiated whether the deformation is greatly reduced in magnitude or disappeared with gravity removed (i.e., a nonstructural curve) or whether the deformity persists and is fixed. They determined reducibility is an elasticity process whereas collapse is a more complex structural process that may predict evolution rate and the effectiveness of treatment. Although the study involved patients with neuromuscular scoliosis, reducibility and collapse are important factors that need to be considered in adult spinal deformity as well. Newer surgical techniques as well as advances in spinal instrumentation have markedly improved the ability to correct spinal deformity, particularly rigid deformity, and correction frequently involves the use of transpedicular instrumentation with or without an anterior release or osteotomy procedure. As the complexity of the surgical procedure increases, the risk for a complication markedly increases particularly in adult patients. To balance surgical benefits and risks, a detailed analysis of the coronal balance, sagittal balance, relative flexibility of all curves, and determination of whether fixed or fused deformity is present is fundamental to effectively treating deformity. There are inherent differences between treating pediatric and adult spinal deformities. In general, adult deformities are more rigid, and there is less compensatory potential in areas adjacent to the deformity. The deformity found in idiopathic adolescent scoliosis (AIS) often will have areas where the deformity is more rigid than others. Determining the relative rigidity with an assessment of structural and nonstructural characteristics of the curve has been used recently as the framework for developing a comprehensive classification of AIS.2,3 This classification assesses curve magnitude on side-bending radiographs and determines whether structural or nonstructural curves are present in the proximal thoracic, main thoracic, thoracolumbar, and lumbar spine. This system also assesses both the thoracic sagittal profile and a lumbar spine modifier. This classification has been proposed as a template to more accurately describe the true nature of a scoliotic deformity and can potentially serve as a guide to best surgical intervention.4–6 Frequently, adult spinal deformity involves abnormalities in both the coronal and sagittal planes. The magnitude of the coronal deformity has not been found to directly correlate with pain. Factors such as lateral vertebral olisthy, L3 and L4 end-plate obliquity angles, loss of lumbar lordosis, and thoracolumbar kyphosis and sagittal balance have been significantly correlated with pain.7,8 In addition to correlation with symptoms, surgical outcome in adults correlates strongly with obtaining good coronal and sagittal balance. The correction strategy for inducing spinal balance in patients with rigid deformity depends principally upon the structural characteristics of the curves and the bone quality. A global assessment of spinal deformity is required in all patients. The analysis begins with full-length scoliosis films to determine coronal and sagittal balance. This is complemented with additional radiographic studies including supine full-length radiographs, flexion, extension, and side-bending views, and the use of push-prone, traction, or bolster radiographs to assess flexibility. The specific indications for each of the supplemental radiographic studies will be discussed in more detail later in the chapter. Computed tomography (CT) or CT-myelogram is often needed for evaluation of congenital malformations of the spine or in cases of prior spinal instrumentation and fusion procedures (Figs. 9–1A to 9–1C). Magnetic resonance imaging (MRI) studies are indicated in any pediatric patient with any neurologic symptoms, rapid curve progression, atypical curve pattern, early onset scoliosis, congenital malformations, or painful scoliosis (Figs. 9–2A and 9–2B). The determination of whether each sagittal and coronal component of a spinal deformity is fixed or flexible contributes significantly toward the surgical decision-making process. The extent of curve flexibility, whether segments are either congenitally or surgically fused, and the compensatory ability of adjacent segments of the spine all impact the choice of surgical approach, spinal levels fused, and the type of implant selected. The degree of flexibility will determine whether an isolated anterior procedure or posterior procedure will suffice or whether a circumferential approach is considered. A rigid and fixed deformity will also dictate whether an anterior release and fusion, a posterior osteotomy, or vertebral column resection procedure is required to successfully achieve spinal balance.9–20 Figure 9–1 Computed tomography (CT) scans are invaluable especially in patients with congenital spinal deformities. (A) Axial CT of a patient with a complex kyphoscoliotic curve demonstrating the location of the spinal cord on the convexity of the curve with a congenitally small pedicle on one side. (B) Another axial CT at the apex of the deformity in a patient with absent pedicles and posterior elements who had severe neuromuscular scoliosis. (C) A coronal CT scan of a patient with a severe congenital kyphoscoliotic curve with evidence of fused ribs and a fairly rigid scoliosis. Figures 9–2 Magnetic resonance imaging (MRI) of the spine is valuable in assessing the location of the spinal cord and other pertinent soft tissue structures. (A) This patient had such a severe curve that the spinal cord is seen in one plane at two different levels of the spine. (B) In some cases the deformity is so severe that multiple planes must be evaluated prior to locating the spinal cord. Inherent characteristics of each spinal deformity also should be considered while assessing its flexibility and its role in the overall management scheme.2 Both curve flexibility and structural characteristics of the vertebrae included in the deformity are major determinant of the ability to achieve deformity correction with a traditional posterior only approach. For instance, an isolated 55-degree main thoracic adolescent idiopathic curve is usually flexible on side-bending films and has almost no secondary degenerative changes. It would be anticipated that following posterior segmental instrumentation an improvement to 25 degrees would be anticipated. Improvement in Cobb angle measurement using modern surgical correction could be expected to exceed 70% for this type of case. However, the treatment of an adult degenerative lumbar curve of similar magnitude would rarely achieve the same amount of correction. The flexibility in an adult curve is usually less as demonstrated by less improvement in curve magnitude on bending radiographs with more superimposed degenerative changes. As illustrated, the management plan for same initial curve magnitudes will be different based on the inherent characteristics of the curves. Advancements in spinal instrumentation have also contributed toward significant evolution in the management of rigid spinal deformity. Many cases treated in the past with circumferential procedures can now be effectively treated with posterior instrumentation using pedicle screws. Pedicle screws engage all three columns of the spine and permit application of strong corrective forces. Several studies demonstrate both improved correction of spinal deformity with the use of pedicle screws compared with traditional techniques and better three-dimensional spinal realignment.7,18,19,21,22 The rigidity or the flexibility of the spinal deformity should be evaluated in all curves that are considered for surgical intervention. Certain techniques of radiographic evaluation have advantages over others depending on the curve characteristics and patient compliance. Traction films may be suitable for cooperative pediatric patients with large and prominent coronal curve or proximal thoracic curves. The use of a bolster placed under the apex of the deformity to maximize postural correction is particularly useful in cases of kyphotic deformity in adolescent or adult patients. This technique permits a better assessment of curve flexibility than can be performed by the patient attempting correction by maximally extending the spine. Literature on radiographic assessment of curve flexibility principally discusses methods of evaluation used in assessing adolescent idiopathic scoliosis and neuromuscular scoliosis. There is unfortunately little data critically comparing the effectiveness of radiographic methods of determining curve flexibility in the adult spinal deformity patient. In all cases, the initial assessment involves upright full-length 36-in. × 14-in. scoliosis films with both posterior/anterior (PA) and lateral views. Because curve magnitudes may vary with the elimination of gravity in supine radiographs, these should be considered in adult scoliosis patients. To optimize visualization for the lateral radiograph, “clavicle position,” where the patient fully flexes the elbows with the hands in a relaxed fist, wrists flexed, placing the proximal interphalangeal (PIP) joints comfortably up into the supraclavicular fossa, thus passively flexing the humerus forward, produces significantly better overall visualization of critical vertebral landmarks compared with positions where the arm is either straight out or partially flexed.16 Ideally, the lateral radiograph should visualize C2 to the pelvis including the femoral heads to assess the sagittal balance of the spinal column. Similarly, on the PA view, the margins of the rib cage and the pelvis along with the femoral heads should be clearly visualized. This will facilitate the assessment of the skeletal maturity of a pediatric patient. The visualization of the ribs helps to determine the associated thoracic cage deformity. Both a congenital fusion of the ribs or significant chest wall deformity are associated with rigid or fused spinal segments. After assessing the spinal balance on the sagittal and coronal planes, the Cobb measurements are obtained for each area of the spine (cervical, proximal thoracic, main thoracic, and thoracolumbar/lumbar). The amount of vertebral body rotation at the apex of the coronal curve also determines the rigidity of the curve. The greater the vertebral body rotation, the greater the rigidity of the coronal curve. If the curve and clinical characteristics warrants the possibility of requiring surgical intervention, then the flexibility of the curve should be performed. Flexibility of the coronal plane deformity is most commonly measured by supine PA left and right lateral bending films. The supine position is recommended so the patient can give a maximal effort without the possibility of falling. This position also eliminates the effect of gravity and will further clarify the flexibility of the deformity. Optimally, the full-length scoliosis films should be used to permit assessment of the flexibility of all areas of the deformity.1,23 Traction and push-prone radiographs have been used by some deformity surgeons to measure the flexibility of the thoracic and lumbar curves.24,25 Traction films are also used to determine the flexibility of the primary and compensatory curves and to assess the inherent capability of the curve to correct with traditional spinal instrumentation techniques. This enables the spine surgeon to determine the extent of intraoperative correction maneuvers that will be necessary to achieve spinal balance both in the sagittal and coronal planes. Traction radiographs are performed by the surgeon pulling on the head and neck while countertraction is applied to the lower extremities (Figs. 9–3A to 9–3E).26 A push-prone radiograph is performed with patient in a supine position with manual force placed over the apex of the spinal deformity. This radiographic technique can determine both the primary curve flexibility and the compensatory curve response with forceful correction of the primary curve.25 For this particular curves pattern in a patient with AIS, the push-prone radiograph most accurately predicts the position of the last instrumented vertebrae when treated with anterior spinal fusion and instrumentation. The technique involves translational forces applied at the apex with counterstabilizing forces applied at the axilla and pelvis on the opposite side. Fulcrum-bending films are similar to bolster films used for kyphosis correction and are advocated by some authors in assessing scoliosis. This method involves placing the patient in the lateral decubitus position and bending over a fulcrum (a radiolucent padded cylinder) so that the spine is passively hinged open. The fulcrum-bending radiograph has been shown to be more predictive of the degree of flexibility and correctability than the lateral-bending radiograph in this group of patients who had segmental spinal instrumentation for correction of idiopathic scoliosis.27 These films are thought to be more effective in predicting curve responses to surgical intervention. Halo gravity traction is an option for assessing very large curves and rigid curves particularly in patients with severe scoliosis, kyphoscoliosis, and kyphosis. It has been found to be a safe, well-tolerated method of applying gradual, sustained traction to maximize preoperative evaluation and postoperative correction in this difficult population.28 Assessment of the flexibility and balance of the spine in the sagittal plane is an important aspect of the evaluation of spinal deformity both in children and adults. This evaluation should be performed in all children with kyphosis, congenital malformations of the spine, and in all adults with spinal deformity. There are several causes of kyphosis and kyphoscoliosis in pediatric patients including Scheuermann’s disease, congenital malformations, achondroplasia, and neurofibromatosis. There are myriad perioperative and operative factors that can lead to an unsuccessful surgical outcome, including inadequate preoperative kyphosis assessment; inappropriate selection of proximal and/or distal instrumentation and fusion levels; inadequate spinal fixation applied at the ends of the posterior construct where tension forces are greatest; failure of a posterior spinal construct; absence and/or an inadequate performance of an anterior spinal fusion when required either before or after the posterior procedure; and overcorrection of the kyphotic deformity based on the ability of the spine above and below to compensate for the correction. Some corrective procedures carry a significantly higher risk of spinal cord injury; for example, any type of correction of a kyphotic deformity carries a substantially higher risk compared with treatment of scoliosis.29
Flexible versus Fixed Spinal Deformity
♦ Structural Characteristics of Pediatric and Adult Deformities
♦ Fixed and Flexible Deformities
♦ Radiologic Evaluation of the Spinal Deformity: Is It Fixed or Flexible?
♦ Balance and Flexibility Issues Impacting Surgical Management
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree