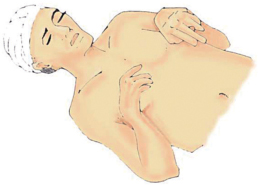
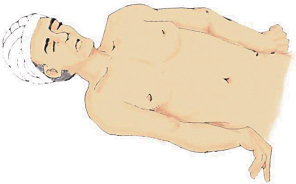
10 What are the six components of a full neurological exam? 1. Level of consciousness/mental status 2. Cranial nerve exam (usually nerves II through XII) 3. Motor exam (Royal Medical Research Council of Great Britain grading scale) 4. Sensory exam (key sensory landmarks) 5. Reflexes (muscle stretch [“deep tendon”] reflexes and primitive reflexes) 6. Coordination and gait What is a “focused neurological exam”? It is a problem-oriented exam (based on the chief complaint and manifested symptoms) that should be conducted in an efficient time frame with the purpose of localizing the lesion. What three deficits may a physician observe by careful observation alone? (1) Obvious speech problems/aphasia (expressive or receptive), (2) general gross motor problems, and (3) dysarthria How long should a focused neurological exam last? It should be patient-specific. Serving as a screening tool, it may be short if there are no findings but extend to a lengthier examination if pertinent positives are found. What are the four objectives of a focused neurological exam? To determine (1) the etiology, (2) appropriate diagnostic testing, (3) the working diagnosis, and (4) ultimately the proper treatment necessary to improve the patient’s presenting symptoms. Such an exam that is both focused and rapid allows the trauma surgeon and neurosurgeon to collaborate and prioritize the patient’s injuries and institute diagnostic tests and imaging before starting treatment. When would extensive examination of higher cerebral functioning, cerebellar functioning, and cranial nerve function be deemed unnecessary? When a patient presents with isolated spinal pathology and does not present with complaints or symptoms that are suggestive of intracranial pathology When should one use the Glasgow Coma Scale (GCS) or Full Outline of Unresponsiveness (FOUR) scale?1 When approximating level of consciousness in a poorly responsive patient What is the maximum number of points that one can receive in the GCS? 15: 4 for eye opening 5 for verbal 6 for motor What is the minimum number? 3 What does “T” mean in GCS scoring? Intubated (e.g., the patient may arrive 3T: unresponsive and intubated from the field) How are points awarded for verbal responses? 1: no verbal response 2: incomprehensible sounds 3: inappropriate words 4: confused, disoriented 5: normal, appropriate speech When applying the GCS, who receives a “best eye opening” score of 4? Those whose eyes are opened spontaneously upon entering the room. Patients who respond to speech only should not be confused with an awaking or a sleeping person; such patients receive a score of 4, and not 3. When applying the GCS, how is best eye opening to pain only (a score of 2) tested? By applying pressure on the patient’s fingernail bed Pulling part of the body away when pinched, exhibiting normal flexion to central pain stimulation When assessing the “best motor response” of the GCS, what is meant by “localization to pain” (a score of 5)? Purposeful movements toward changing painful stimuli (e.g., when the patient’s hand crosses the midline with deep sternal rub or gets above the clavicle when supraorbital pressure is applied)1 How would a physician recognize decorticate posturing (a score of 3) when estimating level of consciousness? Flexion at the arms and elbows, hyperextension of the legs (clue: decorticate = “hands over heart” [or Corazon])1 Fig. 10.1 Flexion at the arms and elbows, hyperextension of the legs. How would a physician recognize decerebrate posturing when estimating level of consciousness? Hyperextension of both the upper and lower extremities1 Fig. 10.2 Hyperextension of both the upper and lower extremities. What is the most important feature of consciousness? Wakefulness What is gained by the nature in which a patient recollects the events of his or her history? Insight about any alterations in memory or judgment When should one check orientation? When a patient is able to communicate What are the six components of the mini–mental state exam? 1. Orientation 2. Registration 3. Attention and calculation 4. Recall 5. Language 6. Visual spatial2 What is the maximum score obtained through the mini–mental state exam? Max score = 30; any score greater than 27 is considered normal.2 What is assessed by the clock-drawing test? Executive functioning, (altered when dementia is suspected) What are the four orientation parameters in order from last to be lost to the first? 1. Person (the last parameter to be lost when mental status is compromised) 2. Place (includes city, state, country, hospital, and floor) 3. Time (includes year, season, month, date, and temporal orientation [i.e., day of the week]) 4. Situation (the first to be lost when mental status is compromised)2 What questions should be asked to test the four aforementioned parameters?
Focused Neurological Exam
10.1 Basic Concepts
10.2 Level of Consciousness/Mental Status
| English/Spanish |
1. Person: | “Sir … (Ma’am …) tell me your name?”/“Senor … (Senora …) ¿Cómo te llamas?” |
2. Place: | “Where are we?”/“¿Dónde estamos?” “What city?”/“¿Qué ciudad?” “What state?”/“¿Qué estado?” “What country?”/“¿Qué país?” “What is this place?/“¿En qué lugar estamos?” If the patient is able to give a correct answer to the above question, ask: “What hospital?”/“¿Qué hospital?” “What floor?”/“¿Qué piso?” |
3. Time: | “What year is it?”/“¿Qué año es?” “What season is it?”/“¿Qué temporada es?” “What month?”/“¿Qué mes?” “What is today’s date?”/“¿Cúal es la fecha de hoy?” “What day of the week is it?”/“¿Qué día de la semana es?” |
4. Situation: | “Why are you here?”/“¿Por qué está usted aquí?” |
How are memory and intellectual functioning routinely tested at bedside or within a clinical setting?
By asking the patient to name three objects immediately and recall them after 5 minutes, to name the last three presidents, and to perform serial subtraction of 7’s from 100
How are speech and language disorders explored during testing of higher cortical functioning?
By testing reading, writing, spelling, and an ability to execute spoken commands, and by asking the patient to name objects and solve simple arithmetic problems
10.3 Cranial Nerves
Which cranial nerve (CN) controls the following:
Secretomotor to the parotid gland causing salivation | Glossopharyngeal (CN IX) via the otic ganglion |
Motor to the sternocleidomastoid (SCM) muscle | Spinal accessory (CN XI) |
Sensation from the tonsils, pharynx, and middle ear | Glossopharyngeal (CN IX) |
Afferent motor and efferent sensory of the GI tract | Vagus (CN X) |
Sensation from the face, sinuses, and teeth | Trigeminal (CN V) |
Information from the carotid sinus and body | Glossopharyngeal (CN IX) |
Motor for accommodation | Oculomotor (CN III) |
Motor for pupillary constriction | Oculomotor (CN III) |
Motor to the lateral rectus of the eye | Abducens (CN VI) |
Efferent sensory from the heart and lungs | Vagus (CN X) |
Afferent motor to the heart and lungs | Vagus (CN X) |
Sensory from the vestibule conveying balance | Vestibulocochlear (CN VIII) |
Secretomotor to submandibular glands for salivation | Facial (CN VIII) via the submandibular ganglion |
Motor to the superior oblique muscle of the eye | Facial (CN VII) |
Motor to the stylopharyngeus muscle and muscles of the upper pharynx | Glossopharyngeal (CN IX) |
Motor to the muscles of the tongue | Hypoglossal (CN XII) |
Taste and sensation of the back of the mouth | Vagus (CN X) |
Sensory and motor to and from the pharynx, larynx, trachea, and bronchi | Vagus (CN X) |
Vestibulocochlear (CN VIII) | |
Secretomotor to the lacrimal glands | Facial (CN VIII) via the pterygopalatine ganglion |
Motor innervation to the strap muscles | Hypoglossal (CN XII) via the ansa cervicalis |
Sensation of smell | Olfactory (CN I) |
Taste from the anterior two thirds of the tongue and soft palate | Facial (CN VIII) via the chorda tympani nerve |
Sensation from the anterior two thirds of the tongue and soft palate | Trigeminal (CN V), mandibular division |
Taste and sensation from the posterior one third of the tongue | Glossopharyngeal (CN IX) |
Supplies motor to the majority of extraocular muscles | Oculomotor (CN III) |
Sensory from the eye, responsible for sight | Optic (CN II) |
Touch sensation of the eye | Trigeminal (CN V), ophthalmic division |
Supplies motor to the muscles of mastication | Trigeminal (CN V), mandibular division |
Supplies motor to the muscles of facial expression | Facial (CN VII) |
Motor to the trapezius muscle | Spinal accessory (CN XI) |
In what manner should cranial nerves be examined?
Cranial nerves should be examined in anatomical sequence to ensure complete examination of all nerves.
What simple test can be done to rule out evidence of raised intracranial pressure?
Funduscopic examination
How may a patient’s visual fields (CN II) be examined?
By confrontation. Corrected acuity is tested in each eye with a Snellen’s chart or Jaeger type card.
How is CN I (the olfactory nerve), governing smell, tested?
Each nostril is examined separately by asking the patient to identify and discriminate between odors (aromatic, nonirritant substances, e.g., soap, coffee, or spices). This CN is rarely tested.
How is CN VII (the facial nerve) examined?
Initially observe the patient, watching for eye closure, asymmetrical elevation of one corner of the mouth, or flattening of the nasolabial fold as he or she talks and smiles. Then, ask the patient to wrinkle his or her forehead by looking upward (examining the frontalis muscle), close his or her eyes tightly while you, the examiner, attempts to open them (examining the orbicularis oculi muscle), purse his or her lips while you, the examiner, presses his or her cheeks (examining the buccinator muscle), and finally, show you his or her teeth (examining the orbicularis oris).
What does weakness to the lower face only signify?
Weakness limited to the lower face signifies a contralateral cerebral (supratentorial) lesion.3
What does weakness involving the forehead signify?
Weakness including the forehead signifies a facial nucleus (brainstem) or facial nerve (peripheral) lesion (i.e., Bell’s palsy).3
How is CN III (oculomotor function) examined?
By checking bilateral pupillary size and reactivity to light and accommodation via a pen light
What are three indicators of CN III dysfunction by exam?
1. Ptosis is present.
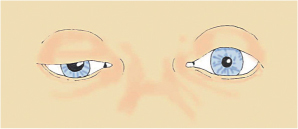
Fig. 10.3 Ptosis of the levator palpebrae muscle may indicate either a CN III palsy (in which it is more apparent) or a lesion to the sympathetic system (less apparent).







