CHAPTER 277 Fungal and Tubercular Infections of the Spine
Epidemiology
The incidence of fungal infections has increased greatly in recent years.1 This increase is thought to be due in part to the greater use of immunosuppressive drugs, more prevalent use of broad-spectrum antibiotics, and more widespread use of indwelling catheters, as well as the prevalence of acquired immunodeficiency syndrome (AIDS).2 The incidence of fungal and other nonbacterial infections is also increasing, not only because of the increasing number of immunocompromised patients but also because of the increasing use of intravenous therapy, central parenteral nutrition, surgery, and hemodialysis.3–5 Fungal infections of the spine are relatively uncommon but arise most commonly from hematogenous spread from another source, often the lung (Fig. 277-1).6–8 Additional routes of infection include direct spread from other organs or from contamination at the time of surgery.9,10 Unfortunately, in most industrialized countries the diagnosis of fungal infection is often delayed because of a variety of factors. This delay has been shown to lead to worse patient outcomes.11 Tubercular infections are simply so uncommon outside the Third World that they are often missed or misdiagnosed on initial evaluation. The importance of appropriate history taking, including a detailed travel history when such an infection is suspected, cannot be overemphasized.
Candida (Fig. 277-2) is most commonly found in normal skin flora and within the gastrointestinal tract but can also exist in the sputum, female genital tract, and urine of patients with indwelling catheters.2 Candida and Aspergillus are the most common types of disseminated fungal infection in susceptible patients, and vertebral osteomyelitis is the most common form of bone infection.3,12–14 Ten species of Candida are pathogenic in humans; 62% of cases of candidal vertebral osteomyelitis are caused by Candia albicans, 19% by Candida tropicalis, and 14% by Candida glabrata.14 Because of the increased use of azole antifungals, the overall incidence of Candida infection of the spine is increasing,15 and Candida is reported to be responsible for approximately 0.7% to 2.7% of spine infections.16–18 The most common (83%14) initial complaint is back pain for more than 1 month. The lower thoracic and lumbar spine is most commonly involved.14
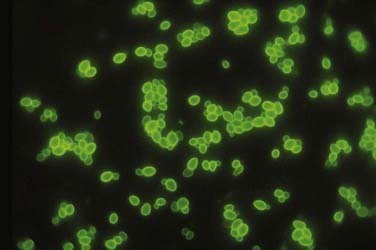
FIGURE 277-2 Appearance of oval budding yeast cells of Candida albicans with fluorescent antibody stain.
(Courtesy of Maxine Jalbert, Dr. Leo Kaufman, Centers for Disease Control and Prevention.)
Aspergillus is a ubiquitous fungus that creates small spores typically found in water, soil, decaying vegetation, hay, and grains,19 thereby allowing deposition into air conduction systems and subsequently human alveoli (Fig. 277-3).2 Although bone infection from disseminated Aspergillus is rare (<1%), the vertebral body is the most common site of such infection.20 The average delay in diagnosis is on the order of months.21 The most common species isolated in human infection is Aspergillus fumigatus.22 Even though Aspergillus most commonly infects the lung, those at risk for development of the disseminated form include patients with AIDS or chronic granulomatous disease and those who take antibiotics long term or abuse intravenous drugs.2 Spinal involvement in disseminated Aspergillus infection is uncommon. When it does infect the spine, the lumbar region is affected in 63% of cases.23 Aspergillus osteomyelitis typically arises as a result of hematogenous spread, extension from an adjacent organ, or direct inoculation at the time of surgery.24–27 Aspergillus vertebral osteomyelitis is similar to other fungal infections of the spine in that it has a male preponderance, bimodal age distribution, predilection for the lumbar spine, and back pain as the most common initial symptom.2
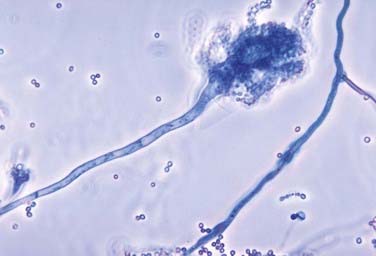
FIGURE 277-3 Photomicrograph depicting the appearance of a conidiophore of the fungus Aspergillus fumigatus.
(Courtesy of Centers for Disease Control and Prevention/Dr. Libero Ajello, Public Health Image Library.)
Cryptococcus infection is rare in immunocompetent hosts; however, 10% to 40% of human immunodeficiency virus (HIV)-negative patients with cryptococcosis have no underlying disease or deficiency.28,29 Although isolated cryptococcal osteomyelitis is rare, 5% to 10% of patients with disseminated central nervous system (CNS) cryptococcosis will have bone lesions.30 Cryptococcus neoformans (Fig. 277-4) is found in pigeon feces and in the soil2; it is the fourth most common infection in patients with HIV and is found in 1% to 5% of transplant patients.31 Typically, the pathogen enters the human host by way of inhalation and can remain dormant. Cryptococcus can then spread to the CNS and bone hematogenously and often resembles a cold abscess, similar to tuberculosis (TB).32 The lumbar spine is most often affected, followed by the cervical region.6 Other sites of osseous involvement include the femur, tibia, rib, and humerus.33 Unlike many other disseminated fungal infections, sinus tract and abscess formation are rare with Cryptococcus.33
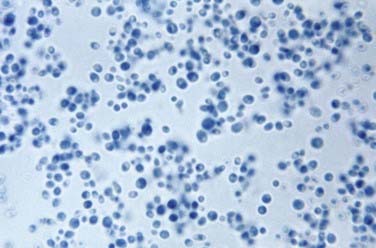
FIGURE 277-4 Photomicrograph depicting the yeast form of a Cryptococcus fungus.
(Courtesy of Centers for Disease Control and Prevention/Dr. Lucille K. Georg, Public Health Image Library.)
Blastomyces dermatitidis (Fig. 277-5) is found in soil and is believed to infect humans by way of inhalation of conidia.34 The pathogen is endemic to the southeastern and south central states, especially those bordering the Mississippi and Ohio River basins, and to the midwestern states bordering the Great Lakes.35 Like other fungal infections, Blastomyces spreads via the bloodstream and can affect any organ months to years after pulmonary infection.7 Even though the skin is the most common site of extrapulmonary infection, osseous involvement is seen in 14% to 60% of patients with disseminated infection. The spine is the most common bone site, followed by the skull, ribs, tibia, and bones of the wrist and foot.36,37 The lower thoracic and lumbar segments are affected most frequently, with the anterior aspect of the vertebral body being involved first. Infection can spread both via the intervertebral disk and along the anterior longitudinal ligament and affect other vertebral bodies; it can also lead to psoas or other paravertebral abscesses.2,33
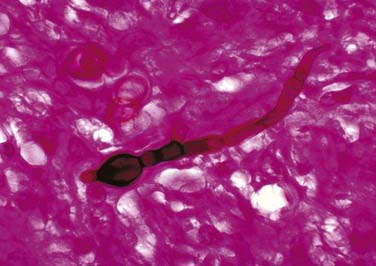
FIGURE 277-5 Micrograph showing the histopathologic changes that reveal the presence of the fungal agent Blastomyces dermatitidis.
(Courtesy of Centers for Disease Control and Prevention/Dr. Libero Ajello, Public Health Image Library.)
Coccidioides immitis (Fig. 277-6) is endemic to parts of the southwestern United States, including the San Joaquin Valley, as well as Central America and parts of South America.38,39 Humans most commonly become infected by inhalation of the spores and less commonly through abrasions of the skin.40 The primary focus of infection is typically in the lung, but in 0.5% of patients the disease is disseminated. Osseous involvement develops in 10% to 20% of those with disseminated disease, and spine involvement occurs in 10% to 60% of these individuals.8,24,33 Those at risk for the development of disseminated disease include Filipinos, African Americans, pregnant women in their third trimester, and younger and elderly individuals.40
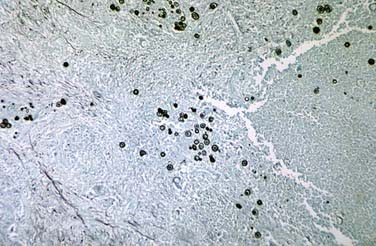
FIGURE 277-6 Methenamine silver–stained photomicrograph revealing spherules of Coccidioides immitis.
(Courtesy of Centers for Disease Control and Prevention/Dr. Martin D. Hicklin, Public Health Image Library.)
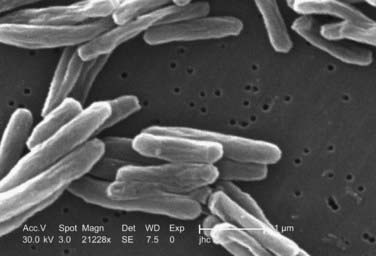
M. tuberculosis (Fig. 277-7) infects nearly one third of the world’s population. According to the World Health Organization (WHO), there were nearly 1.6 million deaths in 2005 alone as a result of TB, the most for any infectious disease. A person with active TB will infect between 10 and 15 other people every year, and according to WHO estimates, someone is newly infected with TB every second. Given these statistics, the burden of TB cannot be underestimated, and it causes significant morbidity when associated with disseminated disease to the spine.
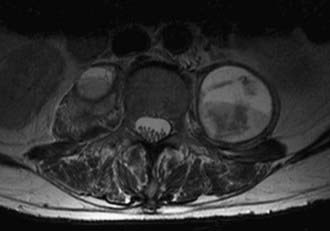
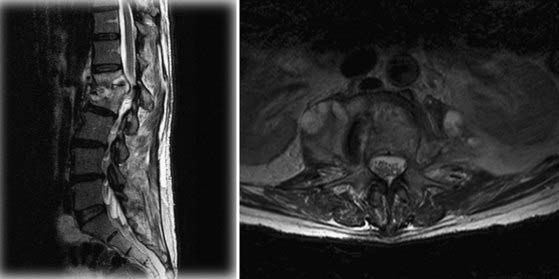
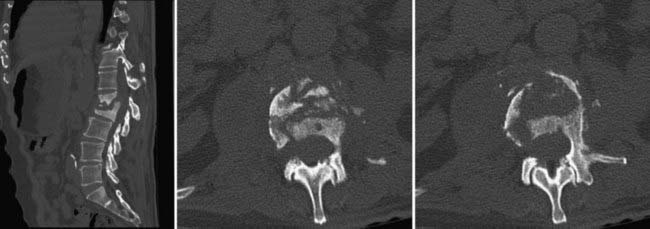
M. tuberculosis primarily infects the lungs through inhalation (Fig. 277-8) and is then spread throughout the body hematogenously. Because of their high blood flow, the vertebral bodies are particularly at risk for infection from disseminated M. tuberculosis. In fact, bone and joint infection account for as many as 10% to 35% of all cases of extrapulmonary TB, with 50% of all cases of musculoskeletal TB involving the spine.41–44 Spinal TB, also known as Pott’s disease, most often affects the lumbar and lower thoracic spine. One common complicating factor in spinal TB is tuberculous abscess (Fig. 277-9), which can often be bilateral.45,46 After primary infection there is ongoing evidence of active containment of reactivating foci by the TH1 cellular immune response, CD4 and CD8, lymphocytes, and interferon-γ.47 Certain factors such as poor nutrition, advancing age, HIV infection, or renal failure can predispose one to progression of disease, and thus active TB can develop immediately or after decades.48 In spinal TB, the focus of infection usually starts in the anterior-inferior aspect of the cancellous vertebral body, and inflammatory bone destruction and caseating necrosis ensue. Infection can then spread behind the anterior longitudinal ligament to infect the adjacent vertebral body. The infection can also spread to adjacent local structures and lead to a potentially compressive epidural abscess. Extraspinal abscesses can erode local structures such as ribs or can expand within the psoas muscle and track down as far as the groin (Fig. 277-10). The destructive capabilities of TB can lead to spinal deformity (Fig. 277-11) and thus create a further set of complications and unique need for intervention.
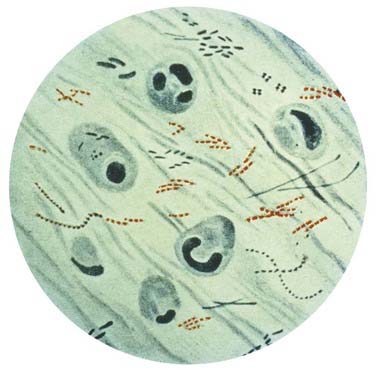
FIGURE 277-8 Photomicrograph of Mycobacterium tuberculosis from a sputum specimen viewed with Ziehl-Neelsen stain.
(Courtesy of Centers for Disease Control and Prevention, Public Health Image Library.)
Historical Perspective
TB has been recognized as an infectious disease process as far back as 4000 BC, with the features of spinal TB having been seen in Egyptian mummies dating back to that period.49 The Greco-Roman civilization knew the disease as phthisis or consumption.50 Paleopathologic evidence of TB of the bones and joints has been demonstrated.51 Hippocrates (400-300 BC) first formally reported TB of the spine with a description of gibbosity above and below the diaphragm.52 Early scientists and physicians in India also described the TB disease process as early as 3500 BC as “yakshma.”52,53 Percivall Pott then described spinal TB in 1779 as “that kind of palsy of the lower limbs which is frequently found to accompany a curvature of the spine.”53,54 Laennec, a French physician, discovered the microscopic pathogen and designated it a “tubercle.”53 Mycobacterium was discovered as the causative agent in 1870. Bacille Calmette-Guérin (BCG) vaccination was introduced in 1945, and specific antitubercular drugs came into common use between 1948 and 1951.50 Before the use of antitubercular drugs, treatment consisted of bed rest and immobilization in specialized hospitals known as “sanatoria,” with the average length of bed rest being 1 to 5 years.50 Treatment of TB of the bones and joints, including the spine, can be divided into three categories: (1) the pre–antitubercular era, where patients were treated by a variety of methods, including ancient medical/pharmacologic therapies, in addition to operative and nonoperative procedures; (2) the post–antitubercular era, where patients were universally treated by radical surgical intervention in conjunction with antitubercular drug therapy; and (3) the post–antitubercular era, where surgical intervention is reserved for those who fail nonoperative management with antitubercular drug therapy or for those with neurological or medical complications requiring surgical intervention.50
Early cases of TB allowed demonstration of the natural history and progression of the disease. For example, skeletal TB was divided into three stages. First, the “stage of onset” consisted of localized infection and a warm tender area of swelling with significant osteoporosis but minimal bone destruction. The second stage, known as the “stage of destruction,” consisted of progression of disease with bone destruction, deformity, subluxation, contracture, and abscess formation. The abscesses often developed draining sinuses that were susceptible to superimposed pyogenic infection, which significantly taxed the host immune system. Cachexia with miliary TB then often developed, as well as tubercular meningitis, thus popularizing the term consumption. Those who survived this stage entered the phase known as the “stage of repair and ankylosis,” in which the overall condition frequently improved. Unfortunately, frequent reactivation of the disease caused progression of symptoms and deformity.50 For those who underwent orthodox nonoperative treatment, only 30% to 44% were able to return to full working capacity.50 Surgery before the advent of antitubercular drugs was aimed at drainage of abscesses and almost uniformly resulted in poor outcomes, including persistent sinus formation, superimposed pyogenic infection, and death. Surgeons then began to pursue operations at sites distant from the location of infection to avoid opening the site of disease. Albee as early as 1911 and Hibbs as early as 1912 developed the technique of posterior spinal fusion in the hope of shortening the period of immobilization and bed rest by providing some degree of internal stability.50 Fusion resulted in some functional improvement in terms of stability but could not offer any benefit for those with neurological deficits.
The advent of antitubercular drugs with streptomycin in 1947, p-aminosalicylic acid in 1949, and isoniazid in 1952 signified a tremendous step forward in the fight against TB. Throughout the 1950s and 1960s, many surgeons continued to aggressively operate on spinal TB. Improved outcomes were due to the fact that antitubercular drugs prevented the dissemination of the disease at the time of surgery that was common before the use of antitubercular agents. As the use of antitubercular agents was becoming more commonplace, resolution of the draining sinuses and abscesses without surgical intervention could occur. Surgeons then began to reserve surgical intervention for prevention and correction of deformity, for patients with neurological deterioration or progressive disease, and in an attempt to improve functionality and the quality of life of severely affected patients.50
Pathophysiology
The various types of fungal and tubercular infections of the spine have variable mechanisms of entering the human host and thus progressing to infection of the spinal column. Most fungal infections that ultimately infect the spine first involve the lung. For example, Aspergillus, Cryptococcus, Coccidioides, Blastomyces, and M. tuberculosis all produce spores that can be inhaled and then spread to the spine, and these organisms can all secondarily infect the spine via hematogenous dissemination. After inhalation, Aspergillus can affect the spine by direct extension from lung tissue or by hematogenous spread. Another important source of infection for some of these pathogens is direct contamination at the time of surgery. Candida infection can occur in patients with intravenous lines or monitoring devices and during implantation of prosthetic devices.2 The difficulty in controlling some of these infections leads to the need for both medical/pharmacologic forms of treatment and possibly surgical intervention. Treatment is needed to both control the primary source and address the sequelae of destructive spine infections.
Clinical Findings
In both fungal and tubercular infections of the spine, the most common initial symptom is localized pain. Given that back pain is such a common complaint with an extremely varied series of causes, it is essential to perform a complete history and physical examination, including pulmonary examination in patients in whom a history of predisposing factors such as travel or immunosuppression should raise the index of suspicion for rare fungal or tubercular infections. For example, a history of previous fungemia, immunosuppression, diabetes, central venous catheterization, intravenous drug abuse, parenteral nutrition, or implanted prosthetic devices all place patients at higher risk for fungal infection of the spine in the setting of back pain.55,56 There are also multiple case reports of Aspergillus infection from contaminated air-handling systems.57 Other factors associated with increased risk for fungal osteomyelitis include diabetes, needle tracks signifying intravenous drug use, opportunistic infections, and weight loss.
Spinal TB is commonly manifested as back pain that progresses over a period of weeks to months. This pain may be associated with muscle spasm and has a mechanical nature in that it may be triggered by even the slightest of movements. This collection of symptoms has been described as causing the patient to have an “aldermanic gait,” or a rigid posture that induces the patient to walk with short deliberate steps to avoid any jarring of the spine.58 Constitutional symptoms such as fever and weight loss, though nonspecific, are present in less than 40% of patients with spinal TB.59,60 One important complication of spinal TB is cord compression. The incidence of neurological involvement in patients with spinal TB has been estimated to be 10% to 46%.61,62 The compression can result from M. tuberculosis itself during the active phase of the infection or be due to the spinal deformity created by the destructive nature of the infection (see Fig. 277-11). The neurological deficit known as Pott’s paraplegia can also be a result of arachnoiditis or vasculitis inducing an inflammatory spinal artery thrombosis.63,64 In industrialized countries, the index of suspicion for Pott’s disease is low,60 and thus late complications, including cord compression and resulting paraplegia, can often be the initial symptoms. However, even in countries in which TB is endemic, access to medical care is poor, and thus 40% to 70% of patients have symptoms of cord compression at the time of diagnosis.64 Late manifestations of Pott’s disease include psoas abscess, as well as rare late paraplegia as a result of degenerative changes at sites of previous infection.
According to Jain, two different types of neurological deficit are associated with TB of the spine: paraplegia in those with active disease (early onset) and paraplegia in those with healed disease (late onset) that appears many years after initial disease onset.62 Paraplegia in those with active disease usually develops as a result of local pressure on the spinal cord itself by tubercular abscess, granulation tissue, tubercular debris, and caseous tissue. Mechanical instability or the formation of kyphosis as a result of vertebral destruction, pathologic fracture, or subluxation can also contribute to neurological complications. The spinal cord itself may begin to display some signs of inflammation such as cord edema, or the disease burden may affect the meninges, which can trigger reactionary inflammatory changes in the cord that result in neurological compromise. In addition, vascular complications such as infective thrombosis or endarteritis of spinal vessels may lead to cord infraction and thus neurological complications. In those with neurological complications as a result of healed disease, the etiology is usually thought to be due to localized pressure on the cord by an osteophyte anterior to the cord or to inflammatory changes and resultant scarring of and around the dura. Stretching of the cord over an anterior internal gibbus can lead to spinal cord gliosis and ultimately neurological complications. It is important to point out, however, that the cord can accommodate remarkably well when the pressure placed on it is slowly progressive, as in TB. For example, Jain and coworkers found that in a case series of patients with spinal TB, the cord can often accommodate as much as 76% canal compromise without neurological deficit. Unfortunately, neurological sequelae can occur at much lesser degrees of canal compromise in the setting of vascular complication or mechanical instability.65
Tuli and associates developed a grading system for spinal TB that encompasses the following stages.66 In stage I the patient does not have any weakness but there is clumsiness of gait and a suggestion of upper motoneuron signs. In stage II the patient has weakness and clear upper motoneuron signs, but the patient is able to walk. In stage III the patient is bedridden because of total muscle weakness and maintains signs of upper motoneuron paraplegia. The patient also has less than 50% sensory loss. In stage IV patients have complete motor weakness, greater than 50% loss of sensation, loss of bowel/bladder control, or any combination of these findings, as well as probably flaccid paraplegia and possibly flexor spasm.
The radiographic appearance of fungal infections of the spine is much like that of the pyogenic causes of spinal osteomyelitis. For example, Williams and coauthors reported a case series of three immunocompromised patients with fungal infections of the spine.67 They described hypointensity on T1-weighted magnetic resonance imaging (MRI), which is typical of many infectious processes. They also noted a lack of hyperintensity on T2-weighted MRI, which is commonly seen in pyogenic infections. This lack of signal was thought to be the result of a depressed immune response in these immunocompromised individuals. Pyogenic infections typically show T2 hyperintensity in the intervertebral disk, whereas the absence of T2 hyperintensity in the intervertebral disk with preservation of the internuclear cleft is more typical of pathogens such as M. tuberculosis. It is also believed that the lack of hyperintensity is a result of the absence of proteolytic enzymes in Mycobacterium.68 Furthermore, involvement of the posterior elements is rare in pyogenic causes of spondylitis but is characteristic of other causes such as TB. It is important to point out that although the lack of hyperintensity with fungal infections may be the result of a blunted immune response, it may also represent the paramagnetic and ferromagnetic properties of the fungus itself, as seen in fungal sinusitis.67 The imaging characteristics of spinal TB are similar to those of a neoplasm, and thus the clinical history must be closely correlated not only to differentiate between pyogenic and nonpyogenic causes of spondylitis but also to distinguish the findings from a neoplasm. Two important characteristics that separate fungal/TB infections, as well as neoplastic processes, from pyogenic infections are sparing of the disk space on MRI and involvement of the posterior elements.69 M. tuberculosis, as well as Blastomyces, can commonly form paraspinal masses with an incidence as high as 55% to 96%.69 TB-associated paraspinal masses also tend to contain calcifications68 and exhibit thick irregular enhancement on computed tomography (CT).70 Another factor that makes tubercular infection difficult to distinguish from neoplastic disease is the fact that TB can involve three or more vertebral bodies in as many as 50% to 64% of patients.68–71 Actinomycosis can also spare the disk space and thus mimic TB or metastatic disease.68
It is important to mention that another key characteristic differentiating spinal TB from pyogenic infections is the duration of symptoms. Typically, TB develops over a period of 2 to 3 years, whereas pyogenic infections become symptomatic in days to months.69 Pyogenic osteomyelitis tends to occur in the sixth to seventh decades of life, whereas TB can develop much earlier in life. In addition, the geographic distribution of TB in less industrialized countries further underscores the importance of a thorough history from each patient.69
Radiographic evaluation of fungal infections of the spine parallels that of tubercular infections in that fungal infections tend to spare the disk space, involve the anterior vertebral body, and lead to the development of large soft tissue abscesses. However, they tend to involve adjacent ribs and posterior elements and develop draining sinuses less frequently.33,38 Paravertebral soft tissue swelling and involvement of the posterior elements are most common with Coccidioides infections.72 Vertebral body collapse and gibbus formation are common with Blastomyces infection,73 and the vertebral body lytic lesions associated with Cryptococcus infection can mimic both Coccidiomycosis infection and TB, including the formation of soft tissue abscesses.33,38,73 CT in patients with fungal osteomyelitis typically reveals hypodensities in the bone itself with small irregular bone islands, as opposed to the appearance of metastatic tumor, in which bone is completely replaced by tumor in larger segments.2
With so many radiographic similarities between fungal and tubercular infections of the spine it can be difficult to distinguish between these lesions for targeting of therapy. Scintigraphic and radionucleotide studies have not been shown to be helpful in differentiating among various pathogens, but other nonspecific markers such as the white blood cell count, erythrocyte sedimentation rate, and C-reactive protein level certainly help reveal the possibility of an infectious process.2,74,75 There are various commercially available antibody tests that have shown varying degrees of success in differentiating fungal causes, but tissue diagnosis via histopathologic examination is essential for establishing the appropriate diagnosis. Finding the correct diagnosis can be aided by other testing methods, such as the carbohydrate assimilation test for Candida and the phenol oxidase reaction for Cryptococcus.76
Tuberculin skin testing in immunocompetent patients with suspected skeletal TB reveals more than 90% to have a positive intermediate-strength skin test.77 However, a small number of immunocompetent patients will have a negative skin test, as will many immunocompromised patients. Therefore, a negative skin test does not exclude TB as a possible cause of infection. Furthermore, the tuberculin skin test is useless in countries in which the BCG vaccine is used. Patients with TB may have draining sinuses. Frequently, the draining exudate is colonized with bacteria or fungi, which when cultured may lead to an incorrect diagnosis. To further complicate diagnosis, 50% of patients with spinal TB have no signs of tubercular disease on chest radiography.44,60,78,79
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree