Generalized Convulsive Status Epilepticus
David M. Treiman
Introduction
Generalized convulsive status epilepticus (GCSE) is the most common and most dangerous type of SE. The earliest mention of SE in the medical literature—in a Babylonian medical text from the first millennium before the Common Era165—referred to what we now know as generalized tonic-clonic SE,109 major motor SE,110 generalized status epilepticus,74 GCSE,135 or grand mal status epilepticus.101 The first modern description of GCSE was provided by Calmeil in 1824,17 who wrote, “There are cases where, as soon as one attack is barely over, another begins, so that there is a succession of up to as many as 40 or 60 uninterrupted attacks. This is what the patients amongst themselves call etat de mal. The danger is urgent; many patients die.” Detailed descriptions of GCSE subsequently were provided by Bourneville,12 Trousseau,152,153 and Clark and Prout.25,26,27 However, it was not until the Marseilles Conference42 that GCSE was clearly distinguished from other types of SE. In 1984, Treiman et al.143 introduced the term subtle GCSE to describe a late and subtle presentation of GCSE. At that time, subtle GCSE was not generally recognized, although Bourneville12 and later Clark and Prout25,26,27 had recognized the dynamic character of GCSE as a disorder with “progressive clinical stages.”
Definitions
Generalized convulsive SE classically has been defined as recurrent generalized convulsions without full and complete recovery of consciousness between seizures or as a single prolonged convulsion without the characteristic evolution of a single discrete seizure. Thus, recurrent primarily and secondarily generalized tonic–clonic seizures without recovery of consciousness between seizures are both forms of GCSE. However, it is now recognized that at least secondarily GCSE is a dynamic state137,138,139,141 (evidence for dynamic changes during primarily generalized convulsions is sparse). If recurrent convulsions are allowed to persist without treatment or with inadequate treatment, a progressive diminution of convulsive activity occurs, so that the motor manifestations of GCSE become increasingly subtle.33 Subtle GCSE is defined as a condition in which a patient exhibits profound coma, convulsive activity consists of only subtle twitches of the extremities or trunk or nystagmoid movement of the eyes, and bilateral (although frequently quite asymmetric) ictal discharges are present on the electroencephalogram (EEG).137 Although the clinical and EEG characteristics of GCSE are different in early (usually overt) GCSE and late (usually subtle) GCSE, there is a continuum between these two presentations, and subtle GCSE may progress to complete cessation of motor activity, even though ictal discharges continue on the EEG. Treiman141 termed this presentation of GCSE electrical GCSE and suggested that this represents the final stage in the progression from overt GCSE. Electrical GCSE, sometimes following more overt GCSE, has also been reported by others.33,34 Many investigators have used the term nonconvulsive SE for such profoundly comatose and severely ill patients.13,33,102,160 Treiman137 suggested that what others have called myoclonic SE (in patients with anoxic or other severe encephalopathies) is really subtle GCSE, even though there may be only one or two (or occasionally no) generalized convulsions before the appearance of signs and symptoms of subtle GCSE. This is an area of controversy, and some epileptologists are not convinced that the subtle convulsive activity and periodic epileptiform discharges sometimes seen in severe hypoxic encephalopathy should be considered SE.
The definition presented also distinguishes subtle GCSE from true nonconvulsive SE (a category that includes both complex partial SE and absence SE), in which the characteristic clinical feature is an epileptic twilight state, although, as noted, the increasingly common use of the term nonconvulsive SE in comatose patients adds confusion to the literature. A progression from overt to subtle motor activity has not yet been described for primarily GCSE.
The definition of GCSE must also deal with generalized convulsive activity that occurs as a single prolonged episode rather than as repeated discrete behavioral seizures. Such a situation is common in the later stages of GCSE, when convulsive movements tend to be subtle, but it may also occur early in an episode of GCSE, especially in children. Here the convulsive movements are more likely to be overt. Most authors have suggested that seizure activity should persist for at least 30 minutes before the diagnosis of SE is made. However, data from Theodore et al.130 confirming the widely held clinical impression that single convulsions that are not part of an episode of SE do not last >2 minutes (discussed later) suggest that 30 minutes of continuous convulsive activity is far too long to be a good operational criterion for the diagnosis of GCSE. For practical clinical purposes, 10 minutes of continuous behavioral or electrical seizure activity, without the evolution of the ictal discharges typical of a discrete generalized convulsion, is a more realistic criterion. Lowenstein et al.75 suggested 5 minutes’ duration as the definition of SE, but this may be too short, especially because discrete generalized convulsions in children may persist for >5 minutes.
Epidemiology
Generalized convulsive SE is the most common type of SE, especially when subtle presentations of GCSE are included. However, in many older reports, GCSE is not clearly distinguished from other types of SE. Hauser47 suggested that there are approximately 65,000 cases of SE in children and adults in the United States each year. However, DeLorenzo et al.32 estimated that there are approximately 150,000 cases of SE in the United States each year, based on extrapolation of data from their community-based study in Richmond, Virginia. About 70%
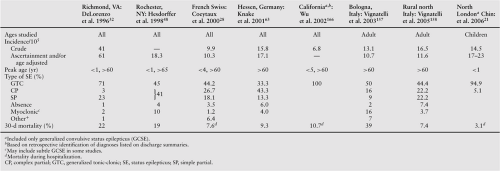
of both adults and children in the Richmond series exhibited GCSE. Shorvon,118 on the basis of a careful review of hospital-, clinic-, and population-based studies, estimated an annual incidence of GCSE of 180 to 280 per million persons in the United States and the United Kingdom. He emphasized that this probably represents an underestimate of the true incidence of GCSE, which almost certainly is still higher in developing countries. In the last decade, eight major population studies of the epidemiology of status epilepticus have been reported, six of which were reviewed by Chin et al.22 Data from all eight studies are summarized in Table 1. Five included all ages,28,32,48,63,166 two included only adults,157,158 and one included only children.21 Six covered all types of status epilepticus; two only included convulsive SE.21,166 Overall, the reported incidence of status epilepticus ranges from 10.3 to 61/105, but the incidence is much higher in the very young (<1 year: 135–156/105) and the elderly (>60 or 65 years: 14.6–86/105). Generalized convulsive status epilepticus (including both primarily and secondarily generalized convulsions) accounted for 33.3% to 71% of the cases when all types of SE were included. These numbers can be extrapolated to give an estimate of at least 2 million cases of GCSE in the world each year.
of both adults and children in the Richmond series exhibited GCSE. Shorvon,118 on the basis of a careful review of hospital-, clinic-, and population-based studies, estimated an annual incidence of GCSE of 180 to 280 per million persons in the United States and the United Kingdom. He emphasized that this probably represents an underestimate of the true incidence of GCSE, which almost certainly is still higher in developing countries. In the last decade, eight major population studies of the epidemiology of status epilepticus have been reported, six of which were reviewed by Chin et al.22 Data from all eight studies are summarized in Table 1. Five included all ages,28,32,48,63,166 two included only adults,157,158 and one included only children.21 Six covered all types of status epilepticus; two only included convulsive SE.21,166 Overall, the reported incidence of status epilepticus ranges from 10.3 to 61/105, but the incidence is much higher in the very young (<1 year: 135–156/105) and the elderly (>60 or 65 years: 14.6–86/105). Generalized convulsive status epilepticus (including both primarily and secondarily generalized convulsions) accounted for 33.3% to 71% of the cases when all types of SE were included. These numbers can be extrapolated to give an estimate of at least 2 million cases of GCSE in the world each year.
Etiology
Older series of cases of SE that tabulated etiologies usually included all varieties of status, but the majority of such cases were GCSE. A summary of these data is provided in the first edition of this book.140 However, even when newer studies are reviewed, the etiology of GCSE has not changed substantially. Ten case series in the last decade have been limited to generalized convulsive status epilepticus (Table 2). Most of these studies used variations on a classification of etiology that includes acute symptomatic and remote symptomatic causes, prolonged febrile seizures, and de novo epilepsy. Hauser47 suggested that 12% of patients with new-onset epilepsy will present in status epilepticus. Over the last decade, 10, mostly prospective, studies of the etiology of GCSE have been reported (Table 2). The etiology of GCSE is quite variable, depending on age and whether the patient has a previous history of epilepsy, as are events precipitating specific episodes of SE. In adults, the most common causes are remote symptomatic, and discontinuation of antiepileptic drugs is the most common cause of SE in patients with chronic epilepsy. Head trauma, central nervous system infection, and cerebral infarction or hemorrhage are frequent causes of SE occurring de novo. In the one series of patients with subtle GCSE,148 life-threatening medical illnesses, including hypoxic encephalopathy, accounted for more than half of the cases. In children, prolonged febrile seizures account for up to 40% of the cases.
Pathophysiology
Most convulsive seizures are of short duration, and the convulsive activity almost always terminates within 2 minutes. Theodore et al.130 studied the convulsive portion of 120 generalized tonic–clonic seizures recorded in a monitoring unit at the National Institutes of Health. The mean duration of the generalized tonic–clonic phase was 62.2 seconds, with a range of 16 to 108 seconds. Thus, mechanisms exist that terminate isolated epileptic seizures within a short period of time. Furthermore, in many patients there is a refractory period lasting for minutes, hours, or days before another seizure occurs. However, under some circumstances, seizure-terminating mechanisms fail and seizure activity either persists or recurs before full recovery of physiologic and neurochemical homeostasis. This, in physiologic terms, is the operational definition of SE. Neuronal inhibitory mechanisms that may contribute to seizure termination include Ca2+-dependent K+ currents, blockade of N-methyl-D-aspartate (NMDA) channels by Mg2+, and the inhibitory effects of adenosine, opioid peptides, and γ-aminobutyric acid (GABA). Kapur et al.,59 using a paired-pulse technique in an electrogenic model of experimental SE, showed that a marked deterioration of GABA-mediated inhibition occurs during continuous hippocampal stimulation, and Treiman et al.151 reported similar findings in hippocampal slices obtained during various EEG stages in lithium/pilocarpine-induced SE. Furthermore, NMDA receptors become activated during continuous hippocampal stimulation,8 and NMDA antagonists block the deterioration of GABA-mediated inhibition.58 Wasterlain and colleagues reported a 50% reduction in synaptic GABAA receptors and increase in synaptic NMDA receptors per granule cell synapse after 1 hour of experimental SE.20,88 On the basis of these observations they propose that alterations in receptor trafficking can explain the transition from isolated seizures to SE and the progressive refractoriness of ongoing GCSE to treatment, especially with GABAergic drugs such as benzodiazepines and barbiturates.
Although it is frequently difficult to sort out cause and effect, there is abundant evidence for profound neuropathologic changes occurring as a consequence of GCSE, starting with Pfleger’s detailed pathologic study of a patient dying in SE.100 Neuronal damage, involving principally the neocortex, hippocampus, thalamus, and cerebellum, has been observed in brains of children and adults dying shortly after an episode of SE.29,40,92,116,167 However, neuronal damage observed after SE could be caused by the initial insult to the central nervous system that precipitated the episode of status rather than by the SE seizure activity itself. DeGiorgio et al.31 attempted to test this possibility with a case-matched control study. These authors studied hippocampal neuronal density in the brains of five adult patients who died shortly after an episode of GCSE; five patients who were as closely matched as possible for parameters such as age, underlying central nervous system insult, and underlying medical conditions, including epilepsy, but who had not had an episode of GCSE; and five age-matched controls with no history of central nervous system insult or epilepsy. In five regions of the hippocampus, the patients with SE had the lowest neuronal counts, the case-matched controls the next lowest, and the central nervous system controls the highest.
Animal studies also provide evidence for SE-induced neuronal damage in previously normal subjects, even when the animals are paralyzed and artificially ventilated.83 Observation of neuronal changes in well-ventilated animals in which adequate glucose levels have been maintained suggest that although systemic complications such as hypoxia, hypoglycemia, lactic acidosis, and especially hyperpyrexia may exacerbate the neuronal damage occurring as a result of sustained seizure activity,9,76,83,120,126 the ongoing seizure activity itself substantially contributes to the neuronal damage.30,43,54,70,89,90,93,154,155 Fujikawa41 detected neuronal damage after only 20 minutes of ongoing pilocarpine-induced experimental SE. There was a progression of distribution and intensity over the 3 hours of observation. Both animal and human studies have shown that the immature brain may be less susceptible to seizure-induced neuronal damage, although it is more susceptible to seizures.
Clinical Features
Generalized convulsive SE is characterized by paroxysmal or continuous motor activity. The motor activity may be of the tonic or clonic type or a combination of both; it may be symmetric or asymmetric, and overt or subtle. However, it is always associated with a marked impairment of consciousness
and with bilateral (although frequently asymmetric) ictal EEG discharges.137 In what Treiman et al.148 called overt GCSE the episode usually begins with a series of discrete generalized convulsions in which tonic or clonic motor activity, or a combination thereof, is associated with EEG discharges that evolve during the course of the convulsion. At this stage, the clonic phase of a discrete generalized convulsion stops abruptly, coincident with the end of the electrographic seizure. Typically, there is a gradual recovery of consciousness following each convulsion, but if the patient has not recovered fully to baseline—usually a fully alert state with no residual confusion or other neurologic symptomatology—before the next convulsion occurs, the patient is considered to be in GCSE. If GCSE is not treated or is inadequately treated, the motor manifestations become increasingly subtle as the episode of SE persists.137 Eventually, only subtle twitching of the fingers, abdominal muscles, or face or nystagmoid jerks of the eyes may be seen. Finally, if GCSE continues for a prolonged period of time, all motor activity may cease, although ictal discharges on the EEG persist. This condition is then called electrical GCSE. Such a term is not an oxymoron because GCSE is a dynamic state in which the clinical and electrical manifestations change with time, as discussed in the Definition section. Thus, the evolution of untreated or undertreated GCSE is usually from overt GCSE to subtle GCSE to electrical GCSE. However, in some patients the encephalopathic insult is so severe (e.g., anoxic encephalopathy) that only one or two generalized convulsions (or sometimes even none) occur before subtle convulsive activity develops or the patient progresses to electrical GCSE.24,156
and with bilateral (although frequently asymmetric) ictal EEG discharges.137 In what Treiman et al.148 called overt GCSE the episode usually begins with a series of discrete generalized convulsions in which tonic or clonic motor activity, or a combination thereof, is associated with EEG discharges that evolve during the course of the convulsion. At this stage, the clonic phase of a discrete generalized convulsion stops abruptly, coincident with the end of the electrographic seizure. Typically, there is a gradual recovery of consciousness following each convulsion, but if the patient has not recovered fully to baseline—usually a fully alert state with no residual confusion or other neurologic symptomatology—before the next convulsion occurs, the patient is considered to be in GCSE. If GCSE is not treated or is inadequately treated, the motor manifestations become increasingly subtle as the episode of SE persists.137 Eventually, only subtle twitching of the fingers, abdominal muscles, or face or nystagmoid jerks of the eyes may be seen. Finally, if GCSE continues for a prolonged period of time, all motor activity may cease, although ictal discharges on the EEG persist. This condition is then called electrical GCSE. Such a term is not an oxymoron because GCSE is a dynamic state in which the clinical and electrical manifestations change with time, as discussed in the Definition section. Thus, the evolution of untreated or undertreated GCSE is usually from overt GCSE to subtle GCSE to electrical GCSE. However, in some patients the encephalopathic insult is so severe (e.g., anoxic encephalopathy) that only one or two generalized convulsions (or sometimes even none) occur before subtle convulsive activity develops or the patient progresses to electrical GCSE.24,156
Table 2 Etiology of generalized convulsive status epilepticus | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree