Fig. 26.1
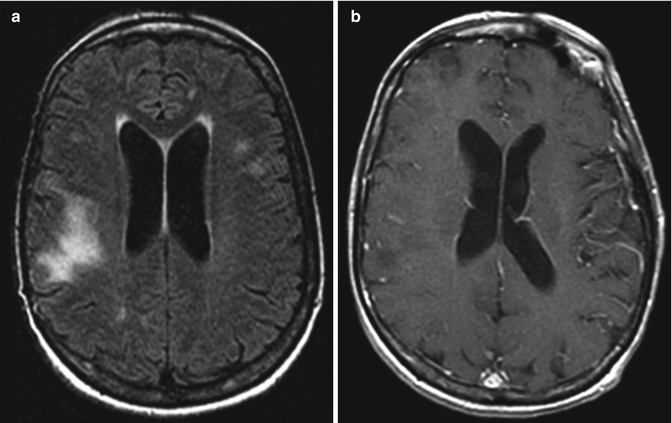
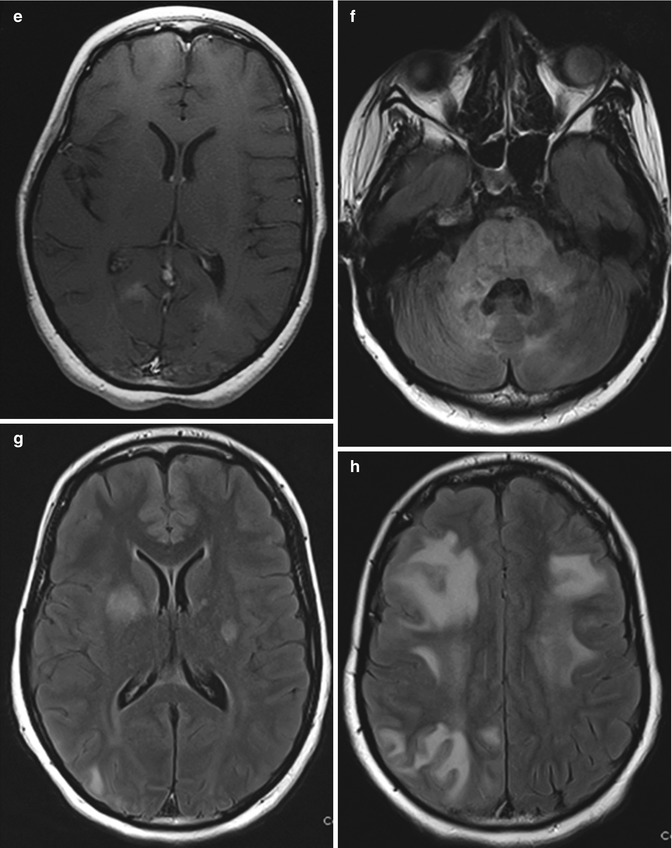
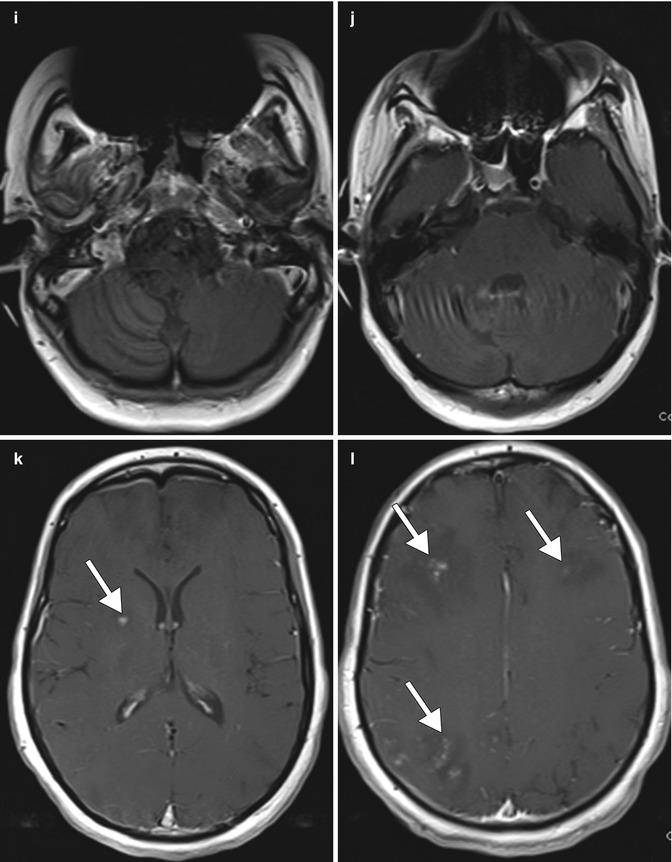
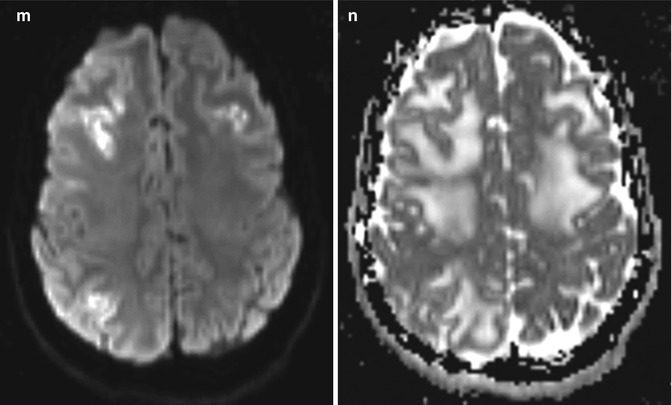
CNS PML-IRIS. The patient was HIV positive and presented with subacute onset of right-sided weakness, slurred speech, and left beating nystagmus. The CD4 count at admission was 5 and the viral load was 82,000. The patient was then started on HAART with three drugs (efavirenz , tenofovir, and emtricitabine). Axial FLAIR (a, b) and post-contrast T1-weighted (c, d) MR images at initial presentation show patchy areas of signal abnormality without associated enhancement in the brainstem, cerebellum, and right basal ganglia. Subsequently, the patient presented with worsening neurologic symptoms, although the viral load decreased to 96 and the CD4 count increased to 11. Axial FLAIR (e–h) and post-contrast T1 (i–l) MR images obtained 1 month after initial presentation show marked interval progression of the signal abnormality in the brainstem, cerebellum, and supratentorial white matter with patchy enhancement (arrows). Corresponding DWI (m) and ADC map (n) show elevated diffusion in the affected white matter
Table 26.1
Imaging findings for the different types of IRIS
Pathogen | Neuroimaging findings |
|---|---|
JC virus PML | Interstitial edema, mass effect, and on contrast T1WI parenchymal and perivascular enhancement |
Mycobacterium tuberculosis | Tuberculoma, basal leptomeningeal enhancement, and hydrocephalus |
Atypical mycobacterium | Lymphadenitis; rarely enhancing lesions in the brain |
Cytomegalovirus | Cerebral vasculitis and infarcts; ventriculitis; retinitis |
Varicella | Cerebral vasculitis and infarcts, which may be associated with parenchymal and leptomeningeal enhancement |
Cryptococcus | Lymphadenitis; gelatinous pseudocysts with restricted diffusion and parenchymal enhancement; cryptococcoma meningitis with meningeal or choroid plexus enhancement |
Toxoplasma | Focal-enhancing parenchymal mass lesions, often with edema |
The keys to the diagnosis of IRIS are the symptomatic and radiologic progression of disease after the initiation of HAART, despite an increasing CD4 T-cell count and the suppression of HIV viremia and the absence of a new opportunistic infection. Treatment for CNS IRIS related to HAART mainly consists of steroids. Patients may succumb to the disease, with mortality rates as high as 30 %.
26.4 Differential Diagnosis
The main alternative diagnostic considerations to IRIS include treatment failure and opportunistic infections without the superimposed effects of HAART. The imaging manifestations of opportunistic infections depend upon the specific pathogen, such as the JC virus, toxoplasmosis, Mycobacterium tuberculosis, or Cryptococcus.
JC virus PML: Untreated PML typically presents as white matter lesions that are often subcortical with low T1 signal and high T2 signal, without mass effect and without contrast enhancement or restricted diffusion centrally (Fig. 26.2). The parietal and occipital lobes are most commonly involved, and the cerebellum is affected in one third of cases.