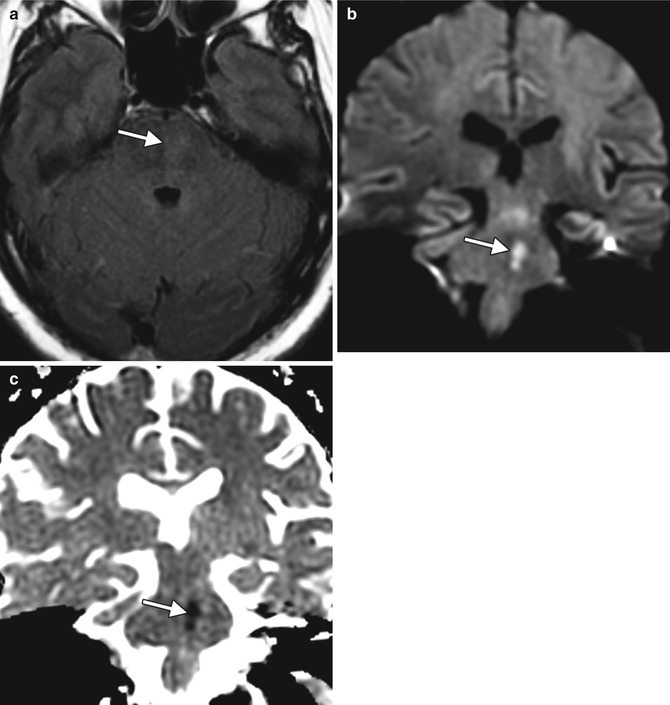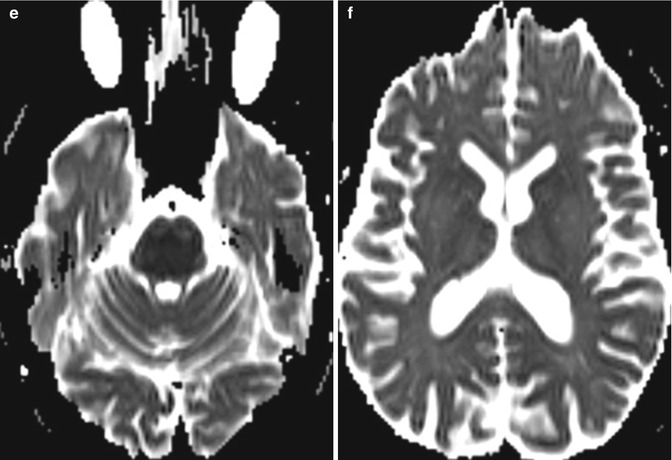
Fig. 36.1
Osmotic demyelination related to rapid correction of hyponatremia with hypertonic saline. Axial FLAIR (a, b), axial DWI (c, d), and axial ADC maps (e, f) show a trident-shaped area of abnormal signal with peripheral sparing within the mid-pons, consistent with pontine myelinolysis. In addition, bilateral symmetric signal abnormality within the basal ganglia, thalami, and external capsules is noted, consistent with extra-pontine myelinolysis. There is restricted diffusion in the pons, but not in the affected portions of the supratentorial brain
36.4 Differential Diagnosis
Osmotic demyelination can also occur in the setting of hyperglycemia, hypoglycemia, normonatremia, and hypernatremia. Without the pertinent clinical history, however, the differential considerations for the imaging findings may include microangiopathy (Fig. 36.2), infarct (Fig. 36.2), neoplasms, such as glioma (Fig. 36.3), and viral encephalitis (Fig. 36.4). Microangiopathy is a chronic process that can produce streaky FLAIR hyperintensity in the central pons and supratentorial white matter without associated restricted diffusion. Unlike central pontine myelinolysis, pontine infarcts can involve the corticospinal tracts and are often unilateral, with a sharp margin along the midline. Furthermore, concomitant involvement of the brainstem and bilateral basal ganglia with stroke is distinctly uncommon. Pontine gliomas tend to present with a mass-like appearance and may or may not demonstrate enhancement. In certain cases, viral encephalitis can affect the brainstem and basal ganglia in a bilateral symmetric manner similar to osmotic demyelination, although involvement of the external capsules is relatively uncommon.