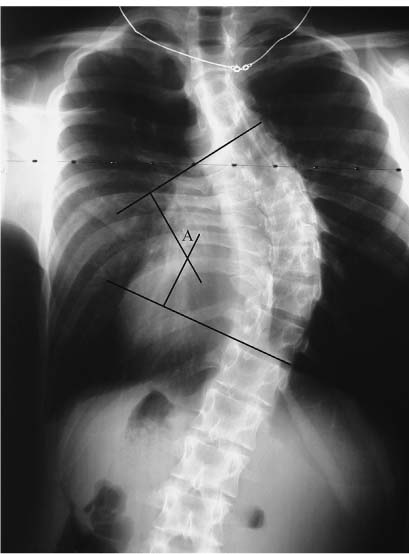
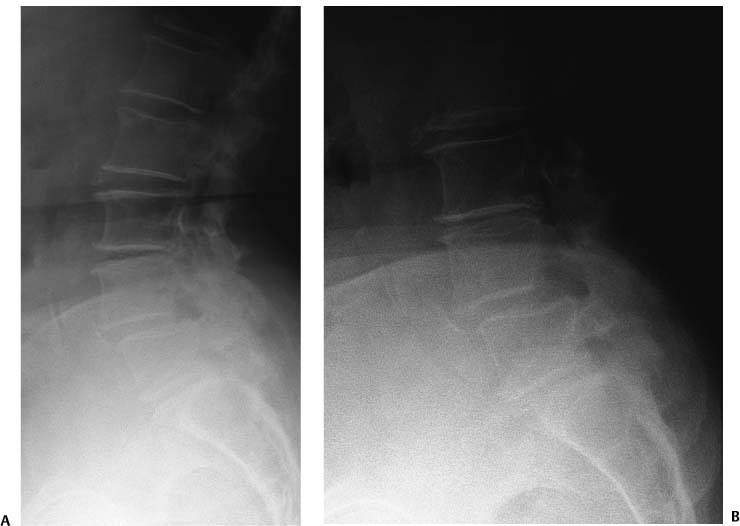
Chapter 2 There are several spinal imaging modalities available to the spine surgeon. These imaging modalities may be used to provide diagnostic information, as part of a preoperative evaluation, intraoperatively, and as a means to follow patients after surgery. Different imaging modalities have different strengths. For example, plain films will not demonstrate a compressive lesion of the cauda equina in a patient with an ependymoma. Magnetic resonance imaging (MRI) is more sensitive for the detection of soft tissue structures affecting the nerves or spinal cord. Conversely, plain films are much more appropriate for the diagnosis and management of spinal deformity (such as scoliosis or spondylolisthesis), and the use of dynamic images, bending, or flexion and extension provides further information regarding spinal mobility and stability. Computed tomography (CT) provides exquisite bony detail and is often useful for preoperative planning. For example, the use of CT to measure the size of the C2 pars interarticularis prior to attempting placement of a C1-C2 transarticular screw helps to prevent screw placement likely to produce a vertebral artery injury. Computer-aided navigation technologies allow the use of preoperative or intraoperative imaging for the intraoperative localization of hidden structures during surgery. These techniques are used to place instrumentation and to immediately assess the position of implants after placement. Some imaging modalities, such as diskography and dynamic radiographs, provide functional information in addition to anatomical detail. The purpose of this chapter is to provide an overview of the more commonly employed imaging modalities in spinal surgery. The relative strengths and weaknesses of each modality will be discussed and illustrated in the context of a clinical example. Figure 2–1 Cobb angle. The Cobb angle is a commonly used measure for the determination of global or regional spinal deformity. It is measured by drawing lines parallel to the superior end plate of the most tilted rostral vertebral body and to the inferior end plate of the most tilted caudal vertebral body. Perpendicular lines are drawn, and the angle (A) formed is the Cobb angle. Plain radiographs are relatively inexpensive, readily available, and probably the best imaging tool for the assessment of spinal deformity. The addition of dynamic images allows for the assessment of ligamentous integrity and for the assessment of spinal rigidity when corrective procedures are contemplated. The disadvantages of plain radiographs are the use of ionizing radiation and relatively poor anatomical resolution compared with other imaging modalities. Scoliosis describes a deformity of the spine with deformation in the coronal and sagittal planes associated with a substantial rotatory component as well. Plain radiographs are commonly used to measure the degree of deformity, and studies are repeated over time to assess for progression of deformity. Coronal plane deformity is measured using the Cobb angle, defined as the intersection between lines drawn perpendicular to the upper end plate of the most tilted cephalad vertebrae and the lower end plate of the most tilted caudal vertebrae1(Fig. 2–1). The Cobb angle has been found to have a reasonable inter- and intraobserver reliability, with the vast majority of measurements made on a given set of films being within 4 to 8 degrees.2,3 The use of automated measuring techniques may improve accuracy and reliability even further.4 The use of repeated films in the assessment of patients with scoliosis does expose young patients to ionizing radiation. There have been several studies that have suggested a higher risk of cancer in patients with scoliosis as opposed to similar patients without scoliosis. Most authors attribute this increased risk to the radiation received as part of the radiographic monitoring of these patients.1,5,6 Spondylolisthesis, or the relative movement of one vertebral body on another, is another type of deformity frequently detected, assessed, measured, and followed with plain radiographs (Fig. 2–2). Multiple grading systems have been proposed to describe the degree of deformity associated with spondylolisthesis. The most commonly used measurement is the Meyerding grading system.7 Meyerding assigned grades of slippage based on the percentage of slip noted relative to the caudal vertebral body. Grade 1 slips refer to a slip of 1 to 25% of the caudal vertebral body. Slips of 26 to 50% are referred to as grade 2, 51 to 75% as grade 3, and 76 to 100% as grade 4. Complete spondyloptisis is referred to as grade 5.7 Figure 2–2 Spondylolisthesis. Plain films are an excellent tool for demonstrating sagittal plane deformity as well as scoliosis. The Cobb technique may also be employed to measure regional kyphosis or lordosis. This film demonstrates a translational deformity at L4-L5 due to spondylolytic (asterisk) spondylolisthesis. Degrees of spondylolisthesis are often graded using the Meyerding classification system (see text). This patient has a slip that is borderline between a grade 1 and a grade 2. Plain films are also useful for the evaluation of traumatic deformity of the spine. Plain radiographs are a useful screening tool for injury to the spine and can provide information regarding both bony anatomy and ligamentous integrity when dynamic images are included. Information derived from dynamic plain films regarding the ligamentous integrity of the spine may also be useful in the setting of degenerative disease, where “unstable” segments are considered for fusion (Figs. 2–3A and 2–3B). The precise definition of instability of the lumbar spine is not universally agreed upon8,9; however multiple authors have described the use of radiographic instability as an important determinant of surgical technique.10,11 Figure 2–3 Dynamic imaging. Extension (A) and flexion (B) radiographs allow for the determination of ligamentous integrity in awake cooperative patients. This patient with neurogenic claudication and lumbar stenosis associated with spondylolisthesis demonstrates a relative kyphosis at L4-L5 in flexion. This degenerative instability may influence decisions regarding the necessity for and technique used to achieve a lumbar fusion at the time of decompression. Static radiographs of the spine are commonly employed to assess the success or failure of bony fusion after surgery for spinal deformity. The accuracy of static radiographs is not sufficient to allow for the definitive determination of fusion (Fig. 2–4). Several authors have reported case series of patients who were believed to have achieved a successful fusion based on static plain radiographs but who were later found to have a pseudarthrosis and vice versa.12,13 The addition of flexion and extension radiographs or thin cut CT improves the accuracy of radiographic determination of fusion success.12,13 In summary, plain radiographs are very useful for the assessment of spinal deformity as they may provide a wide field of view and allow for the determination of spinal alignment and balance. Scoliosis, spondylolisthesis, and malalignment of the spine due to trauma or degenerative disease are often well demonstrated by plain films. Plain films do deliver ionizing radiation and do not usually provide the degree of anatomical detail associated with axial imaging techniques (see below). Plain films are not generally useful for the detection of soft tissue structures, unless such structures affect the bony spine. Finally, static plain films alone are probably not sufficient for the determination of fusion success.12 CT provides excellent anatomical detail of the bony spine. The use of CT as a diagnostic tool is especially useful in trauma, where the sensitivity of CT for detecting fractures or subtle changes in alignment is superior to that of plain films14–16(Fig. 2–5).
Imaging Modalities for Spinal Deformities
♦ Plain Films
♦ Computed Tomography
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree