♦ Preoperative
Special Equipment
- Basic tray
- Intrathecal catheter (Medtronic, two piece, Model 8731)
- Catheter passer (Medtronic, Model 8583)
- Infusion pump for most patients (Medtronic, SynchroMed 2, 20 mL, Model 8637–20)
- Infusion pump for select patients (Medtronic, SynchroMed 2, 40 mL, Model 8637–40)
Operating Room Set-up
- Headlight
- Loupes
- Bovie, bipolar
- C-arm fluoroscopy
Anesthetic Issues
- Monitored anesthesia care in most cases
- General anesthesia for uncooperative or extremely pain-sensitive patients
- Perioperative antibiotics (first generation cephalosporin)
- Pad patient appropriately
Miscellaneous
- Chronic pain patients customarily undergo evaluation by a pain psychologist prior to implantation to rule out psychologic comorbidities that may compromise outcome; this is generally unnecessary for cancer pain or spasticity patients.
- Patients undergo an intrathecal trial of the desired medication prior to implantation; this may consist of a single bolus dose or a catheter-based infusion lasting several days. The purpose is to test the patient’s response to the medication prior to implantation.
- Intrathecal bolus dose for morphine: 1 mg
- Intrathecal bolus dose for baclofen: 50 mcg
- Intrathecal bolus dose for morphine: 1 mg
♦ Intraoperative (Fig. 146.1)
Positioning
- Lateral decubitus position, beanbag support, patient chooses side of pump placement
- Hip and knee flexion to open interlaminar spaces
- Intraoperative fluoroscopy is positioned to permit anteroposterior spinal views; the image intensifier is positioned ventrally so that the surgeon has more room to work when situated at the dorsal incision
Planning of Sterile Scrub and Preparation
- Chlorhexidine scrub of back, flank, and abdomen, followed by alcohol paint, followed by Betadine paint that is allowed to dry
- The goal is to position the infusion pump equidistant from the costal margin superiorly and iliac crest inferiorly, and equidistant from the umbilicus medially and the midaxillary line laterally.
- A 10-cm subcostal incision is marked parallel to and several centimeters below the costal margin to accommodate the desired pump positioning.
- A 4-cm midline dorsal incision is marked over the L4-L5 spinous processes.
Technique
- The incisions are injected with local anesthetic (four parts lidocaine 0.5% with epinephrine, four parts bupivacaine 0.25%, one part sodium bicarbonate)
- Withdraw pump contents using the 22-gauge noncoring needle, and fill with desired drug
- The abdominal incision is opened first, and a subcutaneous pocket large enough to accommodate the infusion pump is created. There should be 1 to 2 cm of subcutaneous fat superficial to the pump; more makes refilling difficult. The wound is packed with gauze to allow hemostasis.
- The dorsal incision is then opened, and dissection is carried down to (but not through) the thoracolumbar fascia. The soft tissue is dissected off the fascia over about a 3- by 3-cm area; this space allows for later coiling and anchoring of the catheter.
- A catheter passer is tunneled from the dorsal to the abdominal incision and is used to place the extension catheter.
- Under fluoroscopic guidance, and using a paraspinous approach, the large gauge Tuohy needle is advanced through the fascia into the next higher interspace (L3-L4). A direct midline approach is avoided since the spinous processes may compress and break the catheter in spinal extension.
- Once the intrathecal space is encountered, cerebrospinal fluid (CSF) will generally flow briskly through the needle with the stylet removed; avoid loss of an excessive amount of CSF.
< div class='tao-gold-member'>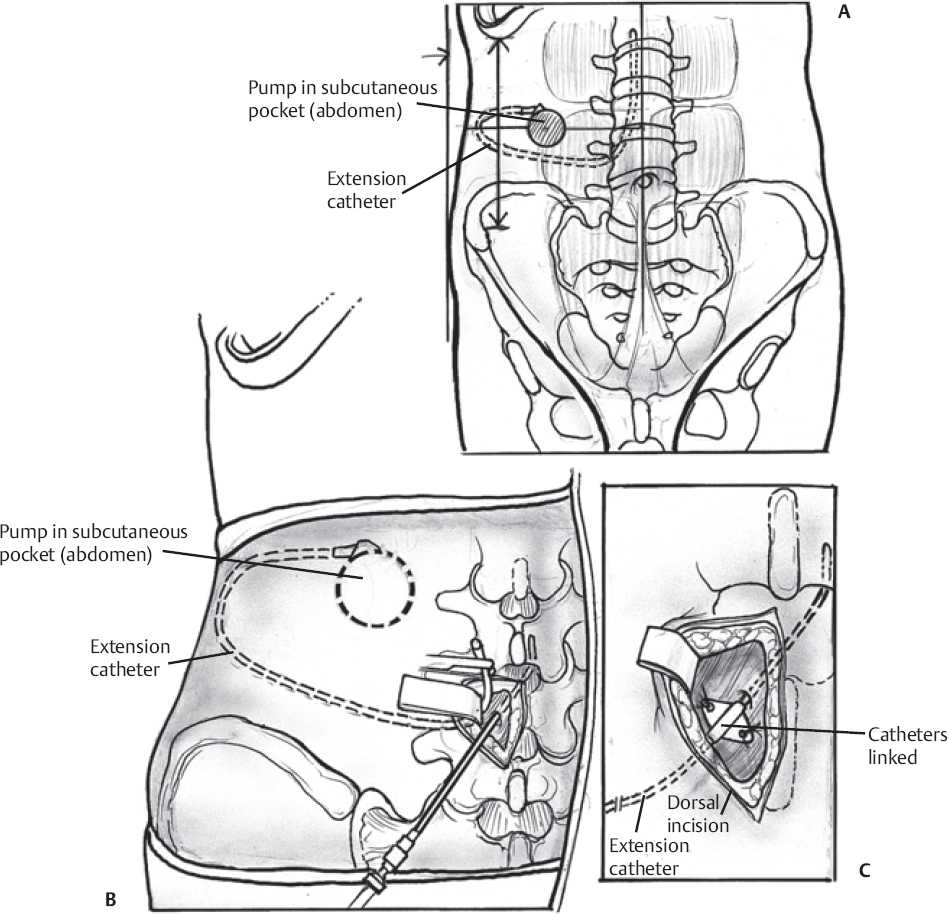 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree







