31 How does encephalitis fundamentally differ from encephalopathy? Encephalitis includes inflammation, whereas encephalopathy is diffuse cerebral dysfunction without inflammation. What other clinical signs and symptoms are commonly associated with encephalitis but not encephalopathy? Fever, headache, focal neurological signs, seizures, leukocytosis, pleocytosis, focal abnormalities on EEG and/or MRI What is the preferred imaging modality for diagnosing encephalitis? MRI What are the most common focal neurological signs encountered with viral encephalitis? Aphasia, ataxia, cranial nerve palsies, hemiparesis, myoclonus, and seizures1 What other abnormalities might be expected? • Diabetes insipidus or SIADH • Autonomic dysfunction What pathogens would you expect in a patient with frontotemporal signs, such as personality changes, memory changes, and aphasia? • Herpes simplex virus (HSV) • Human herpes virus type 6 • Autoimmune • Neoplastic What is the most common cause of sporadic viral encephalitis in the U.S.? HSV Which type of HSV is associated with encephalitis in adults? in neonates? Adults: HSV-I Neonates: HSV-II Which of these is more likely to cause recurrent disease? HSV-II is more likely to cause recurrent, benign lymphocytic meningitis (in patients of any age)2; it is also more likely to cause myelitis in adults. What is the gold standard for diagnosing HSV encephalitis? PCR of HSV DNA in the CSF (brain biopsy shows improvement in neither sensitivity nor specificity)3 What kind of inclusion would be expected on histopathology? Cowdry A inclusion What is the drug of choice for its treatment? Acyclovir (10 mg/kg q8h for 2 to 3 weeks) True or false: A patient known to have HSV encephalitis should be isolated for infection control. False; patients with known herpesvirus or arbovirus encephalitis do not need to be isolated; however, patients whose pathogen is unknown should be on full precautions. If a patient presents with signs of parkinsonism, such as bradykinesia, rigidity, and rest tremor, what pathogen ought to be suspected? Flavivirus (St. Louis encephalitis virus, Japanese encephalitis virus, and West Nile virus)4 What CSF finding would be atypical (when compared with other viral infections) in flavivirus infection? Neutrophils may predominate over lymphocytes What is an arbovirus? An arthropod-borne virus (Togaviridae, Flaviviridae, Bunyaviridae, Reoviridae) that is usually transmitted by mosquitos and ticks What are risk factors for neuroinvasion by West Nile virus (WNV)? • Age >60 • Hypertension • Diabetes • Immunocompromised status How is WNV encephalitis differentiated from meningitis? The presence of signs and symptoms of parenchymal involvement (e.g., clinically, on EEG, or on neuroimaging) How is WNV encephalitis diagnosed? WNV-specific IgM in CSF by enzyme-linked immunosorbent assay (ELISA)5 Which pathogens might be responsible for flaccid paralysis? Those that affect the anterior horn of the spinal cord, including flavivirus, poliovirus, and enterovirus Which arbovirus is associated with encephalitis in about half of affected patients under 20, but 90% of patients over 60? St. Louis encephalitis virus What findings would you expect on MRI? Either normal MRI or increased T2 signal in the substantia nigra Which encephalitis virus’s primary reservoir host is birds? Eastern equine What kinds of mortality rates are associated with eastern equine encephalitis virus? 33% on average, but 50% in patients >604 What kind of virus causes the relatively benign, usually self-limited California encephalitis? Bunyavirus Which viruses compose the enteroviruses? Polioviruses, coxsackieviruses A and B, echoviruses, and the numbered enteroviruses How is infection with poliovirus diagnosed? Reverse transcriptase polymerase chain reaction (RT-PCR) of the CSF Which patients are most at risk of developing encephalitis from nonpoliovirus enteroviruses? Neonates and patients with hypogammoglobulinemia When does encephalitis from nonpoliovirus enteroviruses typically present? Summer months What is seen on MRI? Increased T2-weighted intensity of the cerebral hemispheres What is rhombencephalitis? Extreme brainstem injury that occurs together with pulmonary edema and shock after infection with enterovirus6 What are the major classes of pathogens responsible for meningitis? • Bacteria • Viruses • Spirochetes • Protozoa and helminths What are the clinical signs used to identify meningitis on exam? • Meningismus: nuchal rigidity (sensitivity approximately 30%), photophobia, and headache • Kernig’s sign (sensitivity approximately 5%): flexing the patient’s hip 90 degrees and then extending the knee causes pain • Brudzinski’s neck sign (sensitivity approximately 5%): flexing the patient’s neck causes flexion of the patient’s hips and knees7 Describe the clinical presentation of a child with bacterial meningitis. Vomiting, irritability, seizures Which pathogens are most responsible for neonatal (<1 month) meningitis? • Gram-negative rods (Escherichia coli) (50–60%) • Group B streptococcus (30%) • Listeria (2–10%) Which pathogens most commonly affect children (1 month to 15 years old)? • Haemophilus influenzae (50%) • Neisseria meningitidis (aka meningococcus) (30%) • Streptococcus pneumoniae (aka pneumococcus) (20%) What was almost singularly responsible for changing bacterial meningitis in the U.S. from a disease of children to one of adults? Vaccination for H. influenzae type B has decreased cases by more than 90% in the U.S. H. influenzae meningitis often occurs now secondary to what events? • Skull fractures • Otitis • Sinusitis What kind of effusion may occur as a result of H. influenzae meningitis? Subdural Which pathogens cause most meningitis in patients of ages 15 to 60 years? • Pneumococcus (50%) • Meningococcus (25%) • Staphylococcus (15%) How do older patients (>60 years) with bacterial meningitis present? Altered consciousness and low-grade fever Which pathogens are typically responsible for their disease? • Pneumococcus • Gram-negative rods • Listeria What diagnostic tests should be ordered for any patient suspected of having meningitis? • CT scan of head (for patients suspected of having mass lesions) • LP with CSF analysis and culture • CBC, blood cultures Which patient population would you suspect of needing CT scan before LP may be safely performed? Clinical and neurological features that indicate potential CT abnormalities include age ≥60, history of CNS disease, seizure within 1 week of presentation, altered consciousness, inability to answer two questions or follow two commands, gaze palsy, abnormal visual fields, abnormal language, limb drift, facial palsy, and immunocompromised status8 Is it appropriate to wait for blood and CSF results before beginning treatment? No. Treatment should begin immediately after tests are drawn and LP is completed because bacterial meningitis is potentially fatal. What are the routes by which bacteria may enter the meninges and cause infection? • Direct extension from the sinuses/ears • Hematogenous spread/septic emboli • Abscess rupture • Surgery • Shunt • Penetrating trauma Name the factors that predispose to bacterial meningitis. • Alcoholism • Head injury/recent surgery • Otitis media • Pneumonia • Sickle cell disease What are the major risk factors for death in community-acquired bacterial meningitis? • >60 years of age • Obtunded on admission • Seizures within first 24 hours of illness Which other factors are associated with a poor outcome? • Otitis or sinusitis • Tachycardia • Positive blood culture • Thrombocytopenia • Elevated ESR • Low CSF WBC count What structural feature is shared by the most common meningeal bacterial pathogens? Encapsulation: H. influenzae, N. meningitidis, S. pneumoniae, E. coli, and Streptococcus agalactiae are all encapsulated,9 which may help them survive intravascularly. If a patient presents with a petechial rash (palpable purpura), what pathogen would you expect is causing the meningitis? Neisseria meningitidis What other clinical signs might you expect with meningococcal meningitis? • Cranial nerve VII and VIII palsies • Hydrocephalus What is the most common cause of hospital-acquired bacterial meningitis? Gram-negative bacilli10 Which pathogen causes the majority of bacterial meningitis cases in the U.S.? Streptococcus pneumoniae What test of the CSF specifically identifies pneumococcal meningitis? Quellung If a patient presents with hemorrhagic meningitis, what pathogen would you expect to find on culture of the CSF? Bacillus anthracis What is the mainstay of treatment in bacterial meningitis?? Ceftriaxone 2 g q12h or cefotaxime 2 g q4h What other agents may be added empirically? • If Listeria is suspected: ampicillin • If Staph is suspected: vancomycin • If Gram-negative rods are suspected: aminoglycosides What is the role of dexamethasone in treating meningitis? It has long been recommended in children, but it remains a contentious issue in the current literature with respect to adults. According to Cochrane meta-analysis, corticosteroids reduce hearing loss and other neurological sequelae but did not reduce overall mortality in patients of all ages. True or false: Togaviruses are the most frequent cause of viral meningitis. False; enteroviruses (picornaviruses) are the most common, though togaviruses are also a significant cause. How do CSF findings differ in bacterial versus viral meningitis?
Infections in the Nervous System
31.1 Encephalitis
31.2 Bacterial Meningitis
31.3 Viral Meningitis
| Viral | Bacterial |
Opening pressure | Normal (or slightly elevated) | >18 cm of water |
WBC count | 50–2000 | 10–10,000 |
Lactic acid | Normal | >4 mmol/L |
Glucose | >45 mg/dL | <40 mg/dL |
C-reactive protein (CRP) | Minimal | >100 ng/mL |
Aside from immunodeficiency, what may predispose adults to enterovirus meningitis?
• Physical exercise
• Treatment with rituximab9
What is the most common manifestation of infection with poliovirus?
Aseptic meningitis
How does enterovirus meningitis present in neonates?
With fever with or without rash, vomiting, anorexia, and upper respiratory signs
Is viral culture a useful tool for diagnosis?
No, because the mean time for growth is 3.7 to 8.2 days.
How is enterovirus best diagnosed?
Through RT-PCR
Is there any treatment option for enterovirus meningitis?
Supportive care is the mainstay of therapy. Pleconaril, which integrates into the hydrophobic pocket of enteroviruses and blocks viral replication, may shorten the duration of headache in treated patients.11
What kind of viral meningitis typically follows parotitis by approximately 5 days?
The myxovirus that causes mumps (though occasionally the meningitis may occur without parotitis ever having presented)
What triad of symptoms indicates CNS infection by mumps?
• Fever
• Vomiting
• Headache
Which cells are invaded by the myxovirus?
Ependymal cells, which are also where the virus replicates
If a viral meningitis presents with an diffuse vesiculopapular rash, which pathogen would be expected?
Varicella-zoster virus
What if a patient presents with pharyngitis, lymphadenopathy, and splenomegaly?
Epstein-Barr virus
What is Mollaret’s meningitis?
Recurrent benign lymphocytic meningitis caused by HSV-II
Is it treatable?
Acyclovir is typically offered, though its efficacy has not been definitively demonstrated.2
31.4 Spirochetal Meningitis
During which phase of the natural history of infection with Treponema pallidum is CSF invasion and meningitis most likely to occur?
During early infection. Most cases of syphilitic meningitis occur during the first 2 years of infection.
What are the four syndromes of clinical neurosyphilis?
• Syphilitic meningitis (0.3 to 2.4% of untreated cases within 2 years of contracting disease)
• Meningovascular syphilis (10 to 12% of patients with CNS involvement, approximately 7 years after infection; focal findings secondary to syphilitic arteritis)
• Parenchymatous neurosyphilis (general paresis and tabes dorsales, >10 years after primary infection)
• Gummatous neurosyphilis (late manifestation of tertiary syphilis)9
What are the main presenting features of syphilitic meningitis?
Headache, nausea, and vomiting; meningismus, cranial nerve palsies, and fever are less common in these patients
Why is Venereal Disease Research Laboratory (VDRL) testing of CSF contraindicated in a traumatic tap?
If there is enough blood to be visible, it may cause false-positive VDRL due to blood contamination.
What is the recommended therapy for syphilitic meningitis?
• IV aqueous crystalline penicillin G, 18 to 24 million units daily for 10 to 14 days
or
• Procaine penicillin, 2.4 million units IM daily plus probenecid 500 mg po QID for 10 to 14 days
True or false: Meningitis secondary to Lyme disease is preceded by erythema migrans.
False. This occurs in only approximately 40% of cases. When it does follow the rash, it usually occurs 2 to 10 weeks later.
What is the most common presenting symptom?
Headache
Which cranial nerve is most often palsied?
VII
How long are patients typically symptomatic?
Meningeal reactions improve over days, whereas palsies take weeks or months to improve.
What are the treatment recommendations?
Mild cases: PO doxycycline for 14 days
More serious cases: IV ceftriaxone 2 g daily for 14 days
31.5 Protozoal and Helminthic Meningitis
Which nematode is commonly associated with eosinophilic meningitis?
Angiostrongylus cantonensis
How do people contract it?
By eating a host (mollusk, shrimp, crabs, frogs) or a food contaminated by a host
What clinical signs are associated with A. cantonensis meningitis?
Severe headache, stiff neck, paresthesias, vomiting, and moderate fever, typically 1 to 2 weeks after ingesting an infected food
What laboratory tests are helpful to make a diagnosis?
• Serum and/or CSF eosinophilia
• Larvae may be seen on CSF microscopy (more often in children than adults)
How long do symptoms last?
Disease typically resolves 1 to 2 weeks later
Why is treatment with antihelmintic agents controversial?
Most patients’ infections resolve spontaneously, and larval death may worsen neurological symptoms
What are the two forms of primary amoebic meningoencephalitis, and how does each present?
• Acute form: similar picture to acute bacterial meningitis—after 3 to 8 days’ incubation, high fever, photophobia, headache, nuchal rigidity, and progression to stupor or coma
• Subacute/chronic: low-grade fever, headache, and focal signs with gradual deterioration over 2 to 4 weeks leading to death
Which diagnostic tests may identify amoebic meningitis in the acute form of disease?
• Giemsa or Wright stain of CSF smear
• Increased red blood cell count in CSF
How is it treated?
Though amphotericin B has in vitro activity against amoebas, fewer than 10 patients have been reported to survive primary amoebic meningoencephalitis.9
31.6 Abscess
Describe the four steps to take when CNS abscess is suspected in a patient.
1. CT or MRI of the head to look for mass-occupying lesion
2. If a ring-enhancing lesion is found, the patient should undergo surgical evacuation/aspiration for diagnostic and/or therapeutic purposes. Any lesion ≥2.5 cm should be excised; if the lesions are smaller, material should be aspirated from the largest one.
3. Empiric antibiotics should be started as soon as material has been collected for histopathology and culture.
4. Corticosteroids and phenytoin may be started if there is significant mass effect and/or edema.
What are the surgical options for collecting a sample?
• Open craniotomy and resection
• Aspiration through a burr hole (with or without stereotactic navigation)
Which patients would be the exception to this rule?
HIV+/AIDS patients, because of the high suspicion of toxoplasmic encephalitis, which is treated empirically
When would surgery be indicated in such a patient?
Only if herniation seems to be imminent, in which case a decompressive craniectomy may be indicated
What pathogen is the most common cause of spinal epidural abscess in an immune competent adult?
Staphylococcus aureus, particularly after a previous neurosurgery or trauma
What is the most common cause of intracranial epidural abscess?
Streptococcus anginosus
What other pathogens are frequently found in adults?
Bacteroides fragilis and Pseudomonas aeruginosa
Which antibiotics should be started in a non–HIV-infected patient with a brain abscess?
• Specific therapies if pathogen is known or strongly suspected
• Otherwise, empiric therapy with vancomycin, metronidazole, and a third- or fourth-generation cephalosporin is indicated
Which pathogen is associated with brain abscesses in neonates?
Citrobacter
How is it typically treated?
Third-generation cephalosporins with penems as an alternative
31.7 Empyemas
What is a subdural empyema?
A collection of pus between the dura and the arachnoid meningeal layers
Is subdural hematoma considered a risk factor for developing empyema?
Yes, as the hematoma may become infected
What is the most common predisposing finding to cranial subdural empyema?
Otorhinolaryngeal infection (especially of the paranasal sinuses)
What is another common cause?
Otitis media
Why can infection spread so easily?
There are no anatomical barriers against spreading in this space.
What is the most common pathogen found?
Streptococcus anginosus if there is an individual bacterium, but usually the aspirate is polymicrobial.
What cause has historically been associated with neonates?
Meningitis (however, nowadays meningitis has been shown to cause subdural empyema in older children, due to the prevalence of the H. influenzae B vaccine)
When would you expect to find Propionibacterium acnes?
After a neurosurgical procedure, trauma, or use of a dural allograft
What is meant by a “metastatic” infection?
An empyema may result from “metastasis” of the bacteria from another source, most commonly the lung.
True or false: Empyemas may only result from bacterial infection.
False; Candida may also cause empyema, together with Mycobacterium.
Are antibiotics alone sufficient for treatment?
No, surgery for drainage of the purulent material is indicated, as antimicrobials do not reliably sterilize the infection.
Which subdural empyemas are more common: cranial or spinal?
Cranial
What typically causes spinal empyema?
Spread of infection from another site
Which organism is most commonly found in spinal subdural empyema?
S. aureus
What is the dangerous potential complication of empyema, abscess, and/or meningitis that is more likely to occur in patients with increased coagulability?
Suppurative intracranial thrombophlebitis
31.8 HIV/AIDS
If a patient presents with aseptic meningitis, which pathogen should you test for via RNA PCR?
HIV. Headache, stiff neck, fever, nausea, and vomiting may occur as soon as 1 week after primary infection with HIV.12
What is the most common form of opportunistic meningitis in a patient who is known to have AIDS?
Cryptococcus13
How is cryptococcal meningitis diagnosed?
• CSF enzyme immunoassay
• Confirmatory culture
• Direct observation of the organism by India ink stain is possible in approximately 70% of cases.
Is the risk of bacterial meningitis increased in AIDS patients?
No14
Does HIV infect neurons?
No15
What is the most common neurological complication of HIV infection/AIDS?
Peripheral neuropathies
Name the HIV-associated neuropathies.
• Distal sensory polyneuropathy (bilateral paresthesia, numbness, and pain of the legs)
• Acute inflammatory demyelinating polyneuropathy (similar to Guillain-Barré)
• Nucleoside neuropathy (dose-dependent neurotoxicity of the Nucleoside Reverse Transcriptase Inhibitors [NRTI] drugs)
• Mononeuritis multiplex (acute sensory or motor deficit of a peripheral nerve)
• Progressive polyradiculopathy (occurs late in the illness; diagnosed by CMV in the CSF)
What is the “Sjögren’s syndrome-esque” neuropathy associated with CD8 hyperlymphocytosis?
Diffuse infiltrative lymphocytosis syndrome–associated neuropathy
What is its prognosis?
Patients with this syndrome tend to have higher CD4 counts, fewer opportunistic infections, and better overall survival than other HIV+ patients, though some of these patients develop B cell lymphoma.16
What is HAND, and what causes it?
HIV-associated neurocognitive disorder (HAND) is a symptom of cognitive (forgetfulness, decreased concentration), behavioral (lack of spontaneity, apathy), and motor (gait instability, poor coordination) changes that arises in AIDS patients. It is thought to be mediated by HIV-infected macrophages, the cytokines they produce (including TNF-α, IL-2, IL-6), activation of NMDA receptors, and toxicity of the viral proteins gp120 and tat.
How is HAND best treated?
By antiretrovirals. Those with higher CNS penetrance (zidovudine, nevirapine, ritonavir-boosted indinavir) are thought to help the most, though this is still the subject of much debate.12
What are the most common CNS mass lesions found in HIV+/AIDS patients?
• Toxoplasma encephalitis
• Cytomegalovirus (CMV) encephalitis
• Progressive multifocal leukoencephalopathy (PML)
• CNS lymphomas
For which of these is brain biopsy indicated?
• Toxoplasma is treated empirically with drugs; a biopsy is not indicated.
• CMV may be detected via DNA PCR of CSF or via biopsy.
• PML may require a brain biopsy for diagnosis since highly active antiretroviral therapy (HAART) reduces the levels of JC virus in the CSF (detected by DNA PCR if levels high enough).
• Lymphomas are evaluated first by testing CSF for lymphomatous cells and/or EBV DNA (by PCR) and then by brain biopsy, if CSF evaluation is negative.
31.9 Fungal Infections
Name the most frequent fungal infections affecting the CNS.
• Aspergillosis
• Blastomycosis
• Candida
• Coccidioidomycosis
• Cryptococcus
• Histoplasmosis
• Zygomycosis
Which one is very prevalent in the central U.S.?
Histoplasmosis
Which one is prevalent around the Ohio and Mississippi rivers?
Blastomycosis
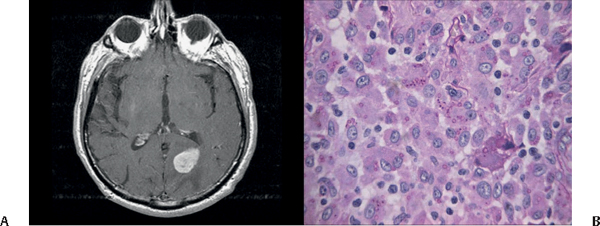
Fig. 31.1 Example of intracranial blastomycosis. (A) Axial MRI demonstrating homogeneously enhancing lesion in the left occipital lobe. (B) H&E stain demonstrating numerous round basophilic single budding yeasts in a reactive parenchyma.







