CHAPTER 14
Infections of the Nervous System
I. Bacterial Meningitis
1. Acute bacterial infection of the leptomeninges, subarachnoid space, and structures passing through the subarachnoid space
2. Routes of infection
a. Nasopharynx (most common)
b. Open trauma/surgical procedure
c. Sinus infection
d. Communicating congenital defect
3. Epidemiology
a. More common in winter
b. Annual incidence: 1 to 2 in 100,000 annually
c. Immunization against Haemophilus influenza with polyvalent pneumococcal and meningococcal vaccines has produced a significant reduction in the incidence in the United States.
4. Etiology
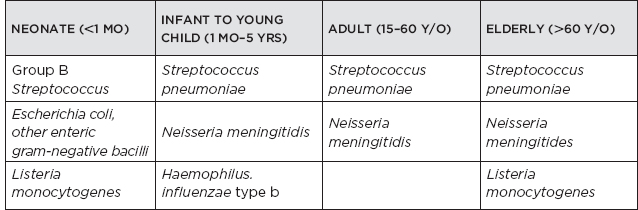
5. Clinical: presents in hours to days with rapid progression. Most patients will have at least two of the tetrad of fever, neck stiffness, headache, and altered mentation.
a. Fever—85% of cases
b. Meningismus (neck stiffness) present in 70% of cases; Kernig’s and Brudzinski’s signs may be present.
c. Diminished level of awareness
d. Headache +/– nausea, vomiting
e. Seizures—poor prognosis
f. Focal neurologic deficits
g. Petechial rash (N. meningitidis)
h. Infant: lethargy, seizures, bulging fontanel
i. Complications
i. Cerebral edema
ii. Hydrocephalus
iii. Stroke due to infectious vasculitis
iv. Sinus thrombosis
v. Cranial nerve (CN) palsies
vi. Disseminated intravascular coagulation (with N. meningitidis)
vii. Syndrome of inappropriate secretion of antidiuretic hormone
viii. Abscess/subdural empyema
ix. Respiratory failure
j. Prognosis: mortality rate of 10% to 15%, highest in pneumococcal meningitis, increased in immunocompromised host
6. Diagnostic testing
a. CT brain: no diagnostic utility in meningitis. Only used to rule out other intracranial processes prior to lumbar puncture. Indications for undergoing CT imaging prior to lumbar puncture: adult patients who are >60 years of age; immunocompromised state; presentation with focal neurological deficits, new-onset seizures, papilledema, abnormal mentation, or history of central nervous system (CNS) disease.
b. Lumbar puncture
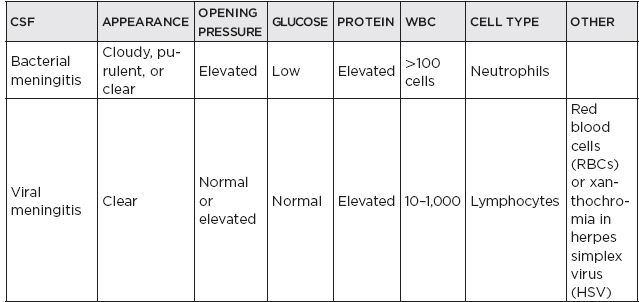
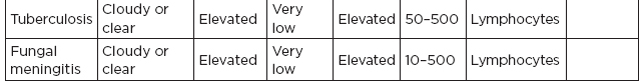
i. Initial cerebrospinal fluid (CSF)
(A) Elevated opening pressure
(B) White blood cell count (WBC): 100 to 10,000 cells/mL, predominantly polymorphonuclear cells
(C) Glucose: <20 mg/dL or <40% of serum glucose
(D) Protein usually elevated, >100 mg/dL
ii. Gram stain: yield low to 20% if treated with antibiotics
iii. Culture: within 48 to 72 hours after institution of antibiotic therapy, the CSF culture is usually negative; blood cultures may be positive in 50% of cases.
7. Treatment
a. Supportive care
b. Antibiotics
i. Always administer immediately if cannot readily perform spinal tap; administration may produce sterile cultures but associated changes in CSF (if necessary, may need to follow CSF parameters).
ii. Empiric treatment
(A) Typical empiric treatment
(1) Ceftriaxone: 2 g q12h
(2) Vancomycin: 30 to 45 mg/kg/day, adjusted to renal function
(a) If Listeria suspected (in those <3 months old or >60 years old (y/o); immunosuppressed, alcoholic), add ampicillin 2 g IV q 4 hours.
(B) Prophylaxis with rifampin for contacts if meningococcal or Hemophilus influenza meningitis
iii. Antibiotics for specific types of bacterial meningitis
ORGANISM | ANTIBIOTIC | DURATION |
Streptococcus pneumoniae | Ceftriaxone and vancomycin | 10–14 days |
Group B streptococcus | Ampicillin | 10–14 days |
Neisseria meningitidis | Ceftriaxone or cefotaxime | 7 days |
Listeria monocytogenes | Ampicillin | 21 days |
Haemophilus influenzae | Ceftriaxone or cefepime | 7 days |
Pseudomonas aeruginosa | Ceftazidime or cefepime | 21 days |
c. Role of corticosteroids: a large randomized trial showed the beneficial effects of 0.15 mg/kg IV q 6 hours for 4 days, in conjunction with antibiotics, for suspected or proven meningitis due to S. pneumoniae; in kids: dexamethasone, 0.15 mg/kg/day, q6h for 4 to 7 days, should be used in conjunction with antibiotics for suspected or proven H. influenzae type B to reduce hearing loss.
d. Droplet precautions need to be undertaken until organism is identified.
8. Recurrent meningitis
a. Evaluate for cranial or spinal defect permitting reentry
b. Evaluate for immune deficiency (i.e., HIV)
c. Differential diagnosis
i. Behcet’s syndrome
ii. Sarcoidosis
iii. Mollaret’s meningitis
II. Viral Infections of the Nervous System
A. General
1. A wide range of neurological manifestations, including meningitis, encephalitis, cerebellitis, CN involvement, myelitis, ganglionitis, and polyradiculitis
2. Most viral infections are mild or asymptomatic.
3. Viral meningitis is more common than bacterial meningitis.
4. Etiologies
a. Enteroviruses cause 90% of viral meningitis.
b. Herpesviruses and arboviruses are the most common causes of encephalitis.
5. Clinical features
a. Malaise, anorexia, myalgia, low-grade fever, vomiting, or headache
b. Physical examination reveals photophobia, somnolence, or irritability, and meningeal irritation.
c. Systemic features to assess include rash, pharyngitis, lymphadenopathy, arthritis, parotid gland enlargement, and hepatosplenomegaly.
d. Seizures and altered mentation in encephalitis
e. Transverse myelitis with flaccid weakness, reduced/absent reflexes, sensory loss, and bladder dysfunction
f. Other neurological manifestations include CN involvement, extrapyramidal symptoms, cerebellitis, acute inflammatory demyelinating polyneuropathy (AIDP), and acute flaccid paralysis.
g. Reye’s syndrome
i. Seen in infection with varicella zoster virus (VZV; chicken pox) and influenza viruses
ii. Develops between ages 2 and 15 years
iii. Strong correlation with aspirin use
iv. Clinical
(A) <72 hours after viral illness
(B) Begins with continuous vomiting followed by increasing lethargy, hypoglycemia, and hyperammonemia with liver failure (and dysfunction of clotting factors)
(C) Death and neurologic sequelae are related to increased intracranial pressure (ICP)
v. Treatment
(A) Supportive care, with strict control of electrolytes and treatment of clotting dysfunction
(B) Observation/treatment of increased ICP
vi. Prognosis depends on severity of increased ICP; mortality is 10% to 30%.
6. Diagnostic procedures
a. Serology—elevated virus-specific antibodies
b. Lumbar puncture for CSF
i. Lymphocytic pleocytosis (10–1,000/mm3), mildly elevated protein, and normal glucose and normal opening pressure
ii. Polymerase chain reaction (PCR) available for HSV, HIV, cytomegalovirus (CMV), enteroviruses, adenoviruses, Epstein–Barr virus (EBV), VZV, and flaviviruses
c. Neuroimaging
i. CT: may be normal in encephalitis
ii. MRI
(A) More sensitive than CT
(B) T2 prolongation or enhancement of cortex in encephalitis; T2 prolongation or cord swelling in myelitis
(C) Distinguish viral encephalitis from acute disseminated encephalomyelitis
d. Electroencephalography (EEG)
i. Viral meningitis: normal or nonspecific abnormalities
ii. Encephalitis: slowing of background rhythms and focal or diffuse epileptiform discharges
(A) HSV-1 encephalitis often presents with temporal slowing or periodic lateralizing epileptiform discharges.
7. Specific antiviral treatment
VIRUS | MEDICATION |
Herpes simplex virus | Acyclovir |
Varicella zoster virus | Acyclovir, valacyclovir, famciclovir |
Cytomegalovirus | Ganciclovir, foscarnet, cidofovir |
Subacute sclerosing panencephalitis | Isoprinosine |
HIV | Highly active antiretroviral therapy regimen (see Section II.B.9) |
B. Specific viral infections of the nervous system
1. Herpes viruses
a. Herpes simplex virus 1 and herpes simplex virus 2
i. HSV-1: causes 90% to 95% of HSV encephalitis
(A) Usually adolescent/adult
(B) Transmitted via oral mucosa
(C) Most common nonepidemic encephalitis and fatal sporadic encephalitis in the United States
(D) Remains latent in the trigeminal ganglia with reactivation and retrograde transmission to the central nervous system (CNS) in two-thirds of cases
(E) Exhibits propensity for the orbitofrontal cortex and temporal lobes
ii. HSV-2
(A) Usually neonate
(B) Transmitted sexually or via birth canal to infant
(C) Involves the brain diffusely via hematogenous transmission
(D) Causes 70% of neonatal HSV infections
(E) Common cause of aseptic meningitis in adult women; may not have concurrent genital herpetic lesions
iii. Clinical features
(A) HSV encephalitis
(1) Prodrome of headache, fever, malaise, or vomiting followed by confusion, personality and behavioral changes, focal or generalized seizures, short-term memory dysfunction, and focal deficits, including weakness and aphasia
(2) Two presentations
(a) Can be rapidly progressive, with coma and death within 2 weeks
(b) Indolent, with hallucinations, headache, memory loss, and behavioral disturbances
(B) Other manifestations
(1) Bell’s palsy
(2) Acute myelitis
(3) Rhombencephalitis/brainstem encephalitis
(4) Aseptic meningitis
(5) Mollaret’s meningitis—recurrent episodes of benign lymphocytic meningitis, common in women; most are caused by HSV-2 infection.
iv. Diagnosis
(A) CSF
(1) Lymphocytic pleocytosis, moderately elevated opening pressure and protein content with normal glucose. Elevated RBC count and xanthochromia may be seen due to hemorrhagic necrosis.
(2) HSV PCR: 99% sensitive and 95% specific. False negatives can occur in the first 72 hours of the illness.
(B) Neuroimaging
(1) MRI brain: restricted diffusion and hyperintensities on T2-weighted sequences in frontal regions, mesial temporal lobe, insular cortex, and cingulate gyrus, with or without gadolinium enhancement. Hemorrhagic changes may be seen. Negative MRI does not rule out HSV encephalitis.
(C) EEG: slowing, periodic lateralizing epileptiform discharges (PLEDs), or frank epileptiform discharges
(D) Pathology
(1) Hemorrhagic encephalitis with neuronal destruction
(2) Predilection for frontal and temporal regions
(3) Cowdry A inclusions
(a) Intranuclear, solitary large viral inclusions with halo due to margination of chromatin
(b) Seen in HSV, VZV, CMV, and subacute sclerosing panencephalitis
v. Treatment
(A) HSV-1 encephalitis: acyclovir, 10 mg/kg q8h for minimum of 14 to 21 days
(B) HSV-2 in neonates: acyclovir, 20 mg/kg q8h for 21 days
vi. Prognosis
(A) Mortality of untreated cases is 70%; mortality for acyclovir-treated neonates is 15%.
(B) Survivors usually have permanent neurologic complications.
b. Varicella zoster virus
i. Primary VZV infection—chicken pox
(A) Peak incidence between ages 5 and 9
(B) Respiratory transmission; typically causes no neurological symptoms.
(C) Postinfectious encephalitis or cerebellitis can occur. In immunocompromised individuals it can cause meningitis or encephalitis.
(D) Reye’s syndrome can be seen in children who receive aspirin.
ii. Reactivation of VZV: after primary VZV infection, the virus persists in a latent state in the dorsal root ganglia
(A) Shingles (herpes zoster)
(1) Virus reactivates and migrates via axon to the skin, producing shingles, erythematous, maculopapular rash that progresses to vesicles associated with radicular pain in a dermatomal distribution
(2) More common among the elderly or immunocompromised
(3) T5 to T10 dermatomes most commonly affected; can be disseminated in immunocompromised individuals
(4) Treatment is acyclovir 800 mg oral 5 times a day for 7 days. Early initiation of treatment reduces pain associated with acute zoster.
(5) Post-herpetic neuralgia can occur, especially in elderly. Gabapentin, pregabalin, and other anticonvulsants, antidepressants, and topical agents are used for treatment of neuralgic pain.
(6) Live attenuated varicella vaccine has been approved for adults >50 years of age to prevent shingles and post-herpetic neuralgia.
(B) Zoster ophthalmicus: due to involvement of first division of trigeminal ganglion; can be associated with VZV vasculopathy/vasculitis
(C) Ramsay-Hunt syndrome: lower CN VII palsy with associated vesicular eruption in the auditory canal
(D) Meningitis and myelitis can occur
(E) Encephalitis is associated with large-vessel vasculitis and can cause focal infarctions. It is usually associated with ipsilateral zoster ophthalmicus. In immunocompromised individuals, small- and medium-sized vessels are involved, causing deep infarctions.
(F) AIDP and brachial plexus neuritis
iii. Diagnosis
(A) Isolation of VZV from the oropharynx or skin lesions
(B) VZV-specific antibodies in the CSF
(C) PCR studies of CSF or vesicular fluid
iv. Treatment
(A) Patients with CNS involvement are treated with IV acyclovir 10 mg/kg q 8 hours for 7 to 14 days with pulse steroids for 3 to 5 days.
(B) Supportive care
c. Epstein-Barr virus
i. Fifty percent of children under age 5 and 90% of adults have had EBV infection.
ii. Acute illness is usually asymptomatic; can present as nonspecific febrile illness or infectious mononucleosis.
iii. Neurologic complications in <1%
(A) Aseptic meningitis—most common acute neurologic complication
(B) Encephalitis
(C) Optic neuropathy
(D) Other cranial neuropathy
(E) Cerebellitis
(F) Acute transverse myelitis
(G) AIDP
(H) Small-fiber sensory or autonomic neuropathy
(I) Primary CNS lymphoma in immunocompromised patients
iv. Diagnostic testing
(A) In meningoencephalitis, brain MRI may be normal or show T2 prolongation involving the basal ganglia, thalamus, white matter, or cerebral cortex.
(B) Diagnosis of EBV infection is usually established serologically but can also be detected in the CSF by PCR.
v. Treatment
(A) Supportive care
(B) No controlled treatment trials available
d. Cytomegalovirus
i. Most adults are seropositive for CMV and are asymptomatic.
ii. Can cause acute and latent or persistent infection
iii. Acquired by body fluid transmission, blood transfusion, organ transplant, etc.
iv. Common in immunocompromised host, including HIV-infected patients and post-transplantation (>40%–90% of transplant recipients)
v. Clinical manifestations:
(A) Congenital CMV infection
(1) Most common congenital infection
(2) Infection occurs in the first trimester. Infection can also occur perinatally during passage through infected birth canal or breastfeeding.
(3) Ranges from asymptomatic infection in 90% to disseminated disease.
(4) Systemic: jaundice, petechial rash, hepatosplenomegaly, or intrauterine growth retardation
(5) Neurologic: encephalitis, retinitis and optic atrophy, microcephaly, microgyria, seizures, abnormal tone, sensorineural hearing loss (CMV infection is the most common cause of congenital deafness).
(6)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




