CHAPTER 84 INFECTIVE NEUROPATHIES
While most peripheral neuropathies encountered by the clinical neurologist will have toxic or metabolic etiologies, it is very important to consider that the syndrome may be caused by an infection. Both bacterial and viral infections are known to cause peripheral neuropathies, as are the autoimmune sequelae of an infectious process. Most infective neuropathies have a distinctive clinical phenotype that will aid in its recognition, especially in the context of a patient’s medical and social histories. The recognition of an infective neuropathy has profound treatment implications, and may offer the rare opportunity to “cure” a peripheral neuropathy.
LEPROUS NEURITIS
Leprous neuritis is a true bacterial infection of peripheral nerves, and nerve invasion is a major hallmark of the disease. The disease has been known since biblical times, and archeological studies of human remains have documented that leprosy did exist in that era. Recent studies based on single nucleotide polymorphisms of the bacillus have pinpointed the origins of leprosy to East Africa, with subsequent spread to Europe and Asia before being reimported into West Africa by explorers.1 In earlier times, the disease was very common in Europe, especially in Scandinavia and England. In 1200 AD, there were some 200 “lazar” houses in the British Islands. There had been an endemic focus in the United States within 100 miles of the Gulf Coast of Texas, Louisiana, and Florida, and a smaller focus in the Midwest originating from Scandinavian immigrants. Now, there are only a few thousand cases in the United States, almost all of foreign origin.
There has been great recent progress in the control of this disease, which is now most common in underdeveloped countries. Newer methods of treatment, especially the introduction of multiple drug therapy (MDT), have resulted in a dramatic decline in active cases. There are now on the order of 300,000 active cases, whereas there were about 14 million cases 20 years ago.2 Many cases are cleared from the active rolls after therapy is given, without follow-up, but the newer drugs seem to be associated with only a small percentage of resistant or relapse cases. The plan of the World Health Organization (WHO) has been to reduce the caseload to such a low level (1 case per 10,000 population) that further transmission becomes unlikely.3 This idea harkens back to the observation that leprosy disappeared from most of Europe following the loss of more than a third of the population in the wake of the Black Plague. This was attributed to a critical decline in the number of infective cases in population centers.
The organism, Mycobacterium leprae, first seen in 1874 by G.H. Armauer Hansen in Norway, is the first bacterium that was associated with a human disease. M. leprae is less acid-fast than M. tuberculosis and requires the Fite modification for acid-fast staining. The ability to invade human nerves is unique, and recent studies of the bacillus have revealed that the actual site of nerve attachment and invasion is the alpha-dystroglycan moiety of Schwann cell myelin.4 The entire genetic sequence of the bacterium has also recently been elucidated, and demonstrates that the organism is highly specialized as an obligate intracellular human pathogen, and has lost many of the enzymatic functions that other acid-fast bacilli have maintained.5 These data may account for the failure to grow M. leprae on artificial media, and the difficulty to infect animals (mouse footpads and genetically susceptible armadillos). M. leprae has a highly thermosensitive growth rate: optimum cell division occurs once per 12.5 days at 27°C to 32°C. There is no growth at core body temperature, and therefore the viscera and central nervous systems are not involved in this disease. This feature limits leprosy to the skin, the anterior third of the eyes, the upper respiratory tract, and the testes. The incubation period varies from several weeks to several years. Children under 16 appear more susceptible to the disease, as are patients with certain types of immunosuppression. Although acquired immunodeficiency syndrome (AIDS) and leprosy are both very common in certain areas such as Africa, AIDS does not seem to increase the vulnerability or severity of coexistent leprosy. The disease is probably spread by infected nasal droplets (where bacteria remain viable for several days) and prolonged skin-to-skin contact.
Leprosy may manifest as a neuropathy, and a well-informed neurologist is capable of making a definitive bedside diagnosis, even in cases where the disease has been fully treated and only residual neurological deficits remain, or in the more rare patient who is trying to conceal the diagnosis. Early diagnosis is critical because one can expect to halt the progress of the neuropathy, and even obtain some degree of reversal. However, severe deficits may remain in advanced cases even after the patient is successfully treated. Cases may be misdiagnosed at medical centers in developed countries because the possibility of leprosy is not considered.
Although there is only one causative organism, the clinical picture of leprosy is wide and related to the host’s innate immune response to M. leprae. In most human populations, 90% to 95% of individuals are genetically equipped to clear the bacilli completely. When resistance is high but insufficient to entirely prevent the disease, “high resistance” tuberculoid or paucibacillary leprosy occurs. Tissue temperature has only a permissive role in shaping this clinical picture. Rather, local invasion by very few bacilli evokes a vigorous epitheloid granulomatous response, which destroys intracutaneous nerves as the lesion forms. The typical patient shows one or a very few asymmetrically dispersed, hypopigmented, anhydrotic skin lesions (Fig. 84-1). A dry patch with pain and temperature loss coinciding with the skin lesion is the diagnostic picture of paucibacillary leprosy (Fig. 84-2). The skin lesion shows central clearing and a slightly raised edge. The centers of such lesions are often clear of bacilli. For diagnosis, the skin biopsy sample should be taken at the elevated edge. Serial sections may be required to see just one or a few bacilli.
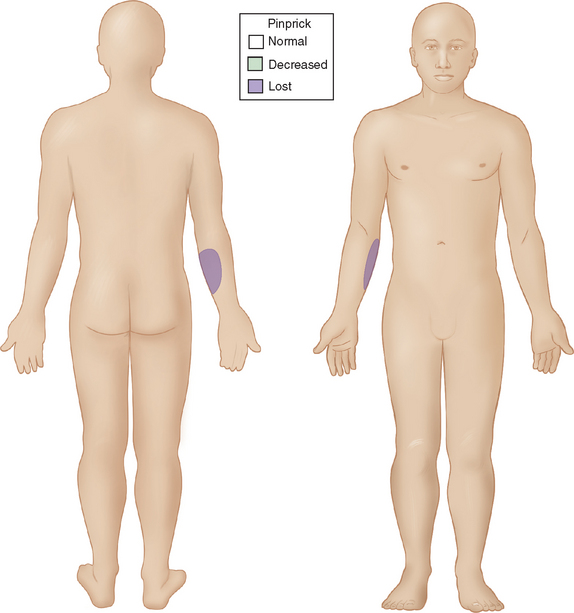
Figure 84-1 Sensory map of tuberculoid leprosy.
(From Sabin TD, Swift TR, Jacobson RR: Leprosy. In: Dyck PJ, Thomas PK, eds: Peripheral Neuropathy. Philadelphia: Elsevier Saunders. 2005, p 2088, Figure 91-3.)

Figure 84-2 Skin lesion of tuberculoid leprosy.
(From Sabin TD, Swift TR, Jacobson RR: Leprosy. In: Dyck PJ, Thomas PK, eds: Peripheral Neuropathy. Philadelphia: Elsevier Saunders. 2005, p 2085, Figure 91-2B.)
When the host has little inborn resistance to the invasion of bacilli, these become widespread and numerous, with hematogenous spread and reproduction in the cooler tissues. Thus, the skin lesions and nerve involvement are roughly symmetric. This form of leprosy is called lepromatous. The palpably enlarged nerves present in this form of leprosy narrow the differential diagnosis. The invasion of intracutaneous nerve networks is manifested by a pattern of temperature-linked sensory loss that starts in the coolest regions of the body, around the breast plate, tip of the nose, lobes and helices of the ears (Fig. 84-3). Once this temperature-linked pattern of sensory loss is discerned, the diagnosis becomes apparent.6 Over the years, the pattern progresses to “less cool” regions and results in very extensive sensory loss, sparing only areas over the carotid arteries, the anterior neck, armpits, inguinal folds, intergluteal folds, and the precordium (Fig. 84-4). The insulating effect of corium of the hands and feet make the tissue temperatures beneath these surfaces somewhat warmer, so that sensory loss tends to occur over the dorsa of hands and feet rather than over the soles and palms. The distribution of skin lesions is also temperature dependent, and roughly approximates the distribution of sensory loss. There are striking examples of small differences in temperature creating distinctive features on the sensory examination. Facial sensation becomes normal at the hairline because of the insulating effect of hair. For example, the old leprosy atlases depict men who followed the Samurai tradition of shaving their heads and experienced leprosy lesions in the scalp; when they let their hair grow back, there was destruction of the follicles except over the warm areas overlying the temporal arteries. The cooler hemiplegic side of a stroke victim showed more extensive sensory loss. Sensory-sparing underbelts, watchbands, and other snug garments have also been documented.
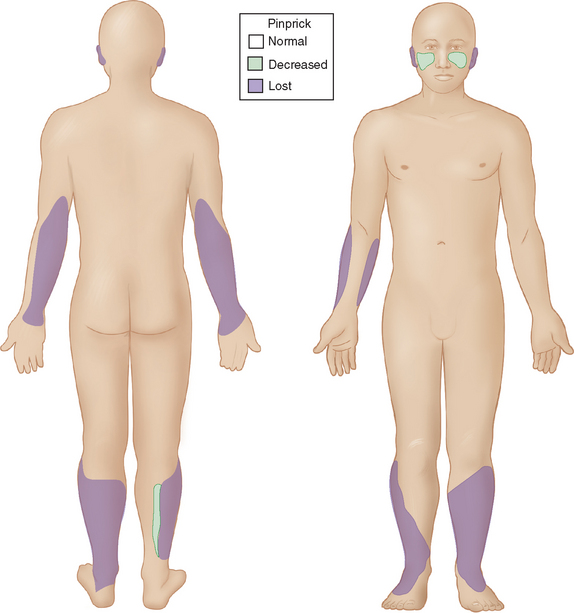
Figure 84-3 Sensory map of early lepromatous leprosy.
(From Sabin TD, Swift TR, Jacobson RR: Leprosy. In: Dyck PJ, Thomas PK, eds: Peripheral Neuropathy. Philadelphia: Elsevier Saunders. 2005, p 2090, Figure 91-5.)
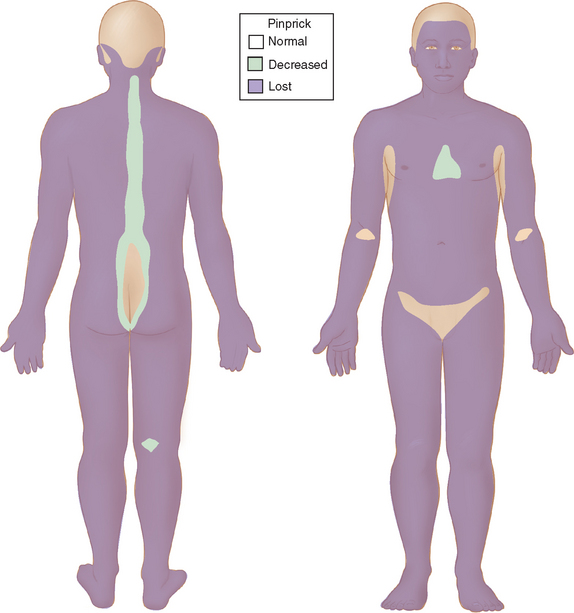
Figure 84-4 Sensory map of chronic lepromatous leprosy.
(From Sabin TD, Swift TR, Jacobson RR: Leprosy. In: Dyck PJ, Thomas PK, eds: Peripheral Neuropathy. Philadelphia: Elsevier Saunders. 2005, p 2091, Figure 91-6.)
The major named nerves, which run closest to the surface of the body, are also affected in a predictable fashion (Fig. 84-5). Thus, the deep peroneal branch to the extensor digitorum brevis of the foot and the ulnar nerve proximal to the olecranon groove are involved early. The median nerve segment from the wrist crease to where it is covered by the forearm flexor muscle group is affected later, with further sensory loss and paralysis of median-innervated intrinsic muscles. Foot drop ensues when the peroneal nerve is affected as it circles around the head of the fibula. Multiple branches of the facial nerve are involved, particularly affecting the medial corrugators of the forehead, the small twigs to the orbicularis oculi and to the muscles composing the nasolabial folds, so as to create a highly diagnostic, patchy paralysis described by Monrad-Krohn.7 If one actually severed the ulnar, median, and peroneal nerves at the sites affected by leprosy, the corresponding deep tendon reflexes would remain intact. The preservation of deep tendon reflexes in the presence of significant peripheral neuropathy is yet another very helpful diagnostic feature.
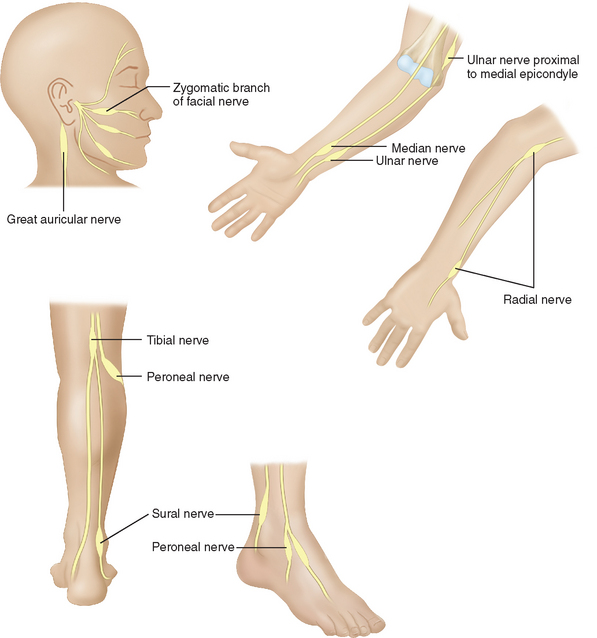
Figure 84-5 The most commonly affected nerves in leprosy.
(From Sabin TD, Swift TR, Jacobson RR: Leprosy. In: Dyck PJ, Thomas PK, eds: Peripheral Neuropathy. Philadelphia: Elsevier Saunders. 2005, p 2089, Figure 91-4.)
Although there are many intermediate forms between these polar types of leprosy, complex interplay between the two themes—tissue temperature and natural immunity of the host—can always be discerned. These cases are labeled dimorphous, borderline, or intermediate. Modern leprosy workers tend to divide all cases into paucibacillary and multibacillary for purposes of management. Among the high-resistance dimorphous cases, there is a group called pure neural leprosy. These patients have no skin lesions but extensive nerve damage, and they can be very difficult to diagnosis, even on sophisticated neurological services. A nerve biopsy may be helpful (the sural or cutaneous branches of the radial nerve are good sites), but a fascicular biopsy at a site of clinical involvement will have the best yield. Polymerase chain reaction techniques can also help in this situation.8
Alterations in immune response, known as leprosy reactions, occur in some patients. In high-resistance cases, there may be a sudden increase in cell-mediated immunity causing acute inflammation of existing lesions and rapid onset of deficits in neighboring and subjacent nerves that had already been invaded by bacilli. The nerve damage will be permanent unless this situation is rapidly recognized and treated with steroids. In multibacillary patients, there is an entity called erythema nodosum leprosum. Here, the circulating immune response goes awry and produces what resembles an autoimmune disease. Features of an Arthus reaction, including consumption of complement and arteritis, are present. Although there are systemic symptoms, the brunt of the damage occurs in the area of greatest bacillary density. Except for the distribution, the erythema nodosum looks the same as in other systemic diseases. Rapid, widespread nerve pain and dysfunction results from vasculitis of the vasa nervorum. This is a situation that must also be quickly recognized. The treatment of choice is thalidomide, but steroids can be used if thalidomide is contraindicated or not available.
When early diagnosis is made, most people require only antibacterial treatment. The most effective antibacterial regimen for M. leprae includes the drugs dapsone, clofazimine, rifampin, ofloxacin, and minocycline. The course of antibacterial therapy depends on whether the patient has the paucibacillary or multibacillary forms of leprosy. Paucibacillary patients receive 100 mg of dapsone daily with rifampin 600 mg monthly for 6 months. Multibacillary patients are given the same combination for 1 year, in addition to clofazimine 50 mg daily, with a monthy 300-mg dose of clofazimine. Shorter regimens used by WHO also make the patient noninfectious in a few days and have an extremely low relapse rate for both types of disease.9 The addition of rifampin has made the greatest difference in the antibacterial treatment of leprosy since the introduction of dapsone in 1940.
HUMAN IMMUNODEFICIENCY VIRUS
Human immunodeficiency virus (HIV) is associated with diverse peripheral nervous system complications (Table 84-1). The specific type of peripheral nervous system syndrome is dictated by the severity of the HIV infection, as determined by CD4+ cell counts.10 Prospective studies indicate that the incidence of symptomatic peripheral nervous system complications due to HIV is around 3%, and complications are more common in more advanced cases.11 If peripheral nervous system complications are assessed by clinical symptoms and electrophysiological tests, the incidence in prospective studies is much higher, at least 30%, and advanced HIV infection again poses a higher risk. Assessing the epidemiology of HIV-related peripheral nervous system complications is confounded by the fact that several common antiretroviral drugs used to treat HIV are themselves toxic to peripheral nerves.
TABLE 84-1 Peripheral Nervous System Complications From Human Immunodeficiency Virus Infection
HIV seroconversion may be accompanied by an acute peripheral nervous system process, most commonly unilateral but also bilateral facial nerve palsies.12 Guillain-Barré syndrome is known to occur at the time of HIV seroconversion, and Guillain-Barré syndrome may be the presenting feature of HIV infection. The Guillain-Barré syndrome associated with HIV is clinically and electrophysiologically identical to non-HIV Guillain-Barré syndrome,13 and is characterized by acute flaccid paralysis with diminution or loss of reflexes. However, instead of the albuminocytological dissociation of typical Guillain-Barré syndrome, the cerebrospinal fluid in HIV-associated Guillain-Barré syndrome often shows a pleocytosis. HIV serology may be initially negative for several weeks following seroconversion. If clinical suspicion for HIV is high, HIV viral load can be used for the diagnosis in the acute setting. The therapeutic approach and therapeutic response is similar in HIV-associated Guillain-Barré syndrome and in idiopathic Guillain-Barré syndrome.
The peripheral nervous system complications of early HIV infection, with CD4 cell counts above 500 cells/μL, are similar to the complications of HIV seroconversion, and are dominated by facial nerve palsies and Guillain-Barré syndrome. However, these peripheral nervous system processes are seen in a small minority of HIV patients.10
In moderately advanced HIV infection, with CD4 cell counts between 200 and 500 cells/μL, peripheral nervous system complications are due to immune dysregulation.10 Chronic inflammatory demyelinating polyneuropathy (CIDP) is known to occur in HIV, and, like Guillain-Barré syndrome, CIDP in HIV is clinically and electrophysiologically identical to non-HIV CIDP. Again, a mild mononuclear cerebrospinal fluid pleocytosis is often seen. Pathologically, CIDP in both HIV and non-HIV forms is characterized by macrophage-mediated demyelination. Although there are no therapeutic trials with HIV-infected CIDP patients, it is believed that they respond to treatment like non-HIV CIDP patients.14 Corticosteroids, plasmapheresis, and intravenous immunoglobulin are the usual therapies for CIDP. When immunosuppressant treatment is utilized, prophylaxis against opportunistic infections is warranted.10
Mononeuritis multiplex caused by vasculitis is known to occur with HIV infection of all severities, but especially in moderately advanced cases. The clinical syndrome is characterized by a progressive accumulation of individual nerve lesions, leading to multifocal sensory and motor derangement, with electrophysiological evidence of multifocal axonal neuropathies. Axonal degeneration is the most common pathological finding on nerve biopsy, with perivascular or endoneurial inflammatory infiltration. Although the etiology of mononeuritis multiplex in HIV is unknown, it may be due to the deposition of HIV-related antigen and antibody immune complexes in perineural vessels. Treatment with immunotherapy should be reserved for patients with disabling deficits, as all therapies have the potential of worsening the underlying immunodeficiency, and milder cases are known to improve spontaneously. When the degree of immunodeficiency from HIV is profound (CD4+ cell count less than 100) and mononeuritis multiplex is present, the suspicion of cytomegalovirus infection should be high, and these cases should be treated aggressively with ganciclovir, foscarnet, or both.15 Cytomegalovirus infection is discussed in further detail later.
Diffuse infiltrative lymphocytosis syndrome is characterized by CD8+ cell infiltration of visceral organs, resulting in enlarged salivary glands and sicca syndrome.16 Peripheral nerves can be infiltrated, resulting in polyneuropathy. This is usually a painful distal symmetric sensory polyneuropathy, which develops subacutely over weeks. Electrophysiological studies reflect an axonal process. Nerve biopsy reveals diffuse CD8+ cell infiltration of the epineurium and endoneurium. Highly active antiretroviral therapy is effective in diffuse infiltrative lymphocytosis syndrome.17
Several recent case reports have described motor neuron disease in the setting of HIV infection, with the potential for clinical improvement after the initiation of highly active retroviral therapy.18,19 These cases are of great interest because they may help us understand the basic mechanisms of motor neuron diseases in general.
Approximately one third of patients with AIDS will develop a clinically significant distal symmetric polyneuropathy (DSP).20 DSP is the most common peripheral nervous system complication of HIV infection, and is present on autopsy in nearly all patients who die from AIDS.21 Risk factors for the development of DSP include elevated HIV viral load, low CD4+ cell counts, and exposure to neurotoxic antiretroviral medications.
Nerve biopsies are not routinely performed in DSP. When obtained, nerve biopsies show distal axonal degeneration, affecting both unmyelinated and myelinated axons.21 Perivascular mononuclear infiltrates may be present.
The pathogenesis of DSP in HIV infection is not known. As direct neuronal infection is not believed to occur, recent research has focused on indirect mechanisms. Attention has been directed toward the HIV-1 envelope protein gp120. Current hypotheses propose indirect neurotoxicity from gp120 via chemokine receptors on Schwann cells and neurons.14
As with other painful neuropathies, treatment is largely symptomatic. There is some evidence that highly active antiretroviral therapy may mildly improve DSP.22,23 Symptomatic treatments have been based on drugs used in other painful sensory neuropathies (especially diabetic polyneuropathy), including amitriptyline, gabapentin, and lamotrigine. There is no evidence to suggest that any one of these agents is specifically effective in the DSP of HIV. Narcotics may be needed in refractory cases. As with all other aspects of HIV management, careful attention to drug-drug interactions is important when choosing a symptomatic therapy.
Several nucleoside analogue reverse transcriptase inhibitors are known to cause a toxic polyneuropathy, and this has been a frequent confounder in the study of DSP. The so-called “d-drugs”—ddC (dideoxycytidine), ddI (didanosine), and d4T (stavudine)—are all known to cause a dose-dependent toxic polyneuropathy.24 The clinical syndrome is identical to DSP, and usually develops after several months of treatment with a d-drug. Distal numbness and painful dysesthesias develop, and exam reveals distal sensory abnormalities with diminished or abolished ankle jerks. Electrophysiological studies demonstrate a distal sensory-predominant axonal polyneuropathy. Serum lactate levels may help in determining if a painful sensory polyneuropathy is drug-related or due to the HIV infection itself.25 Offending drugs should be stopped in all patients with DSP. “Coasting” may occur, whereby the patient’s symptoms continue or worsen for 6 to 8 weeks after removal of the toxic drug.10
Due to similar modes of transmission, co-infections with syphilis, hepatitis C, and human T-lymphotropic virus type 1 (HTLV-1) should be considered in the evaluation of peripheral nervous system syndromes in the HIV-infected patient, as they may act as confounders.10









