Chapter 23 Injuries to the Cervical Spine
• The cervical spine is mobile and highly prone to traumatic injury.
• Early immobilization of the cervical spine and its thorough evaluation with imaging allow identification of a cervical injury and minimize further injuries related to the clinical evaluation of patients.
• The clinician should always search for clinical and imaging signs of ligamentous injury.
• Injuries can be classified as bony, ligamentous, or both according to various classification schemes described in the text. The type of injury and its degree of stability dictate the intervention, which may include conservative management with external immobilization or aggressive management, including open or closed reduction, or internal stabilization and fusion.
• Spinal cord injury may present in a delayed fashion. In all cases of incomplete spinal cord injury, early reduction, when appropriate, should be considered.
The cervical spine is the most mobile portion of the spine and the most common site of spinal injuries. The relative traumatic involvement of different spinal levels is shown in Table 23.1. Nearly 12,000 to 14,000 spinal cord injuries occur each year in the United States.1–6 Cervical spine trauma accounts for almost 1.5% of all pediatric trauma admissions.7 Nearly 10,000 patients die each year as a result of an injury to the spinal cord.5,8–11
TABLE 23.1 Incidence of Adult Spine Injuries
| Spinal Segment Level of Injury | Incidence |
|---|---|
| Cervical | 60% |
| Thoracic | 8% |
| Thoracolumbar | 20% |
| Lumbar | 10% |
| Sacral | 2% |
The most common mechanisms of injury to the cervical column are motor vehicle accidents, falls, and sports. Teens and young adults ranging in age between 15 and 30 are the most frequently injured population.2,5,12–14 Falls account for 18% to 30% of cervical spine injuries in the younger age group (<8 years) and for 11% in the older age group (>8 years). Sports injuries are more prevalent in the older group (20-28%) and uncommon in the younger group (3%).15,16 Nonaccidental trauma and penetrating injuries are also found in small numbers of very young children and adolescents, respectively.
The cause of spinal injury varies with age, and particularly with gender. Males are three to four times as likely to sustain an injury as females. Fractures are the most common injury pattern in all age groups, although ligamentous disruptions and dislocations are more prevalent in the young. Upper cervical spine injuries (C1-C4) are almost twice as common as lower cervical injuries (C5-C7).1,17–19 Subluxation injuries without fracture and spinal cord injuries without radiographic abnormality (SCIWORA) are less common in adults and are more likely to occur in younger patients.17,18,20
Neurological Injury
As many as 15% of patients who sustain a traumatic spinal injury will sustain a neurological injury as a result.5,14 Injuries to the cervical spine, in particular, result in a much higher incidence of injury to the spinal cord than injuries at any other spinal level. The incidence of spinal cord injury ranges from 2% to nearly 100% of cervical spine injuries, depending on the cervical level involved, with an incidence of 40% to 60% overall (Table 23.2).1,2,5,8–12,21,22 The incidence of spinal cord injury associated with cervical fractures is likely to be underestimated because some patients may die before reaching medical attention. This situation is particularly true of atlanto-occipital dislocations, in which 25% of patients may die as a result of respiratory arrest before evaluation.4,5,14
TABLE 23.2 Cervical Spine Injury and Neurological Deficit
| Injury Level | Incidence of Neurological Deficit |
|---|---|
| Atlanto-occipital dislocation | Up to 100% |
| Atlas | 1-2% |
| Axis | 10% |
| C3-T1 | 6% |
| Unilateral cervical facet dislocation | 60% |
| Bilateral cervical facet dislocation | Up to 100% |
The level and mechanism of the spinal injury, the force involved, and the patient’s age and medical status have important influences on the extent of neurological injury following trauma. In particular, conditions such as ankylosing spondylitis or Down syndrome, which have a significant effect on the relative rigidity (or laxity) of the spinal column, may predispose affected individuals to neurological injury.5,14 Furthermore, the status of the patient after spinal injury can influence neurological injury, mainly through the deleterious effect of hypotension or hypoxia.3,5,13,14 The American Spinal Cord Injury Association (ASIA) scale23 is a clinical assessment tool that offers a detailed overview of the extent and type of spinal cord injury in an efficient and easy to apply format (Fig. 23.1).
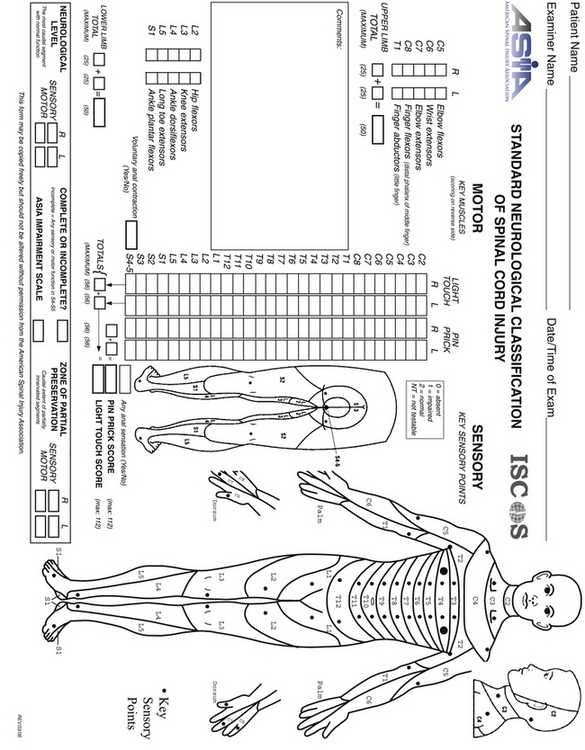
FIGURE 23.1 The American Spine Injury Association (ASIA) scale for spinal cord injury.
(Used with permission from the American Spinal Injury Association.)
General Principles
Given the significant incidence of spinal injury, clinicians must maintain a high index of suspicion for potential spinal injury in all trauma patients. All trauma patients should be immobilized until an appropriate and thorough evaluation of the spine for fractures or instability is completed. Ideally, immobilization should be initiated at the trauma scene and maintained during triage, resuscitation, and primary and secondary surveys. The primary trauma survey places special emphasis on the airway, breathing, and circulation (ABCs of resuscitation). In patients improperly immobilized, the primary survey can exacerbate existing cervical spine injuries in nearly 10% of the cases.4,5
In 2002 the Joint Section on Disorders of the Spine and Peripheral Nerves of the American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS) published specific evidence-based guidelines for the management of acute cervical spine and spinal cord injuries.24 We have adopted these guidelines and discuss them here.
Imaging
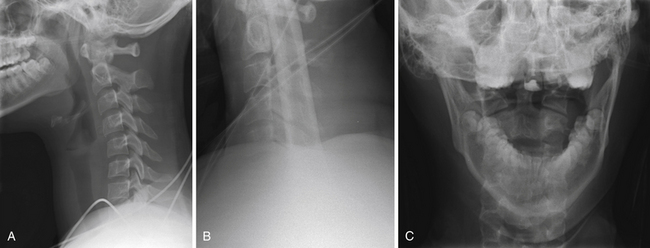
In a trauma situation, the evaluation for cervical injury usually begins with a cross-table lateral radiograph (Fig. 23.2A). A swimmer’s view may be added to visualize the cervicothoracic junction and the top of the T1 vertebral body (Fig. 23.2B).5,14,25 The combination of a cross-table lateral and swimmer’s view has an 85% sensitivity and a negative predictive value of 97% for fracture.25,26 An open-mouth odontoid view should be obtained to assess the C1-C2 vertebrae and articulations and is particularly valuable for assessment of the odontoid process (Fig. 23.2C). If an open-mouth view cannot be obtained for whatever reason, the pillar (oblique) view can be utilized to demonstrate the odontoid process. The anteroposterior view is often ignored by inexperienced clinicians, but it can identify injuries with a rotatory component, such as unilateral facet dislocations, that may not be readily apparent on lateral films. With the use of the anteroposterior, lateral, and open-mouth odontoid views, the sensitivity and negative predictive values of the series are 92% and 99%, respectively.25–27 Adding oblique views to the standard series does not increase the sensitivity.28
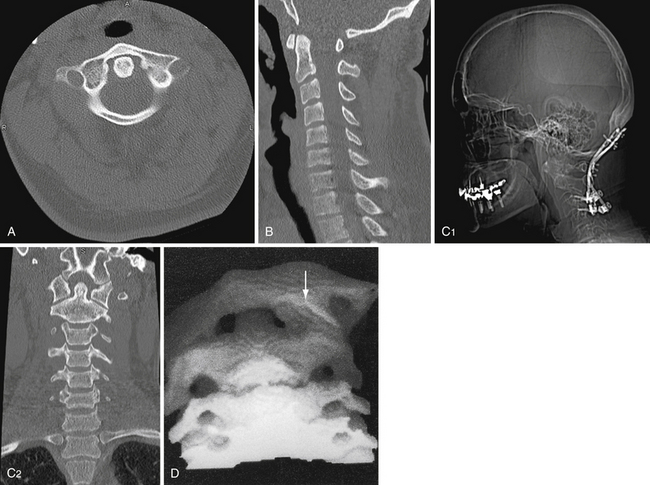
The use of computed tomography (CT) has become commonplace in the evaluation of the trauma patient and is particularly useful for evaluating the occipitocervical and the cervicothoracic junctions. However, the routine use of CT in the trauma setting is difficult to recommend as there have been no direct comparisons with plain radiographs.29,30 Areas identified as possible injury on plain radiographs should be further investigated with CT with fine sections through the suspicious area (Fig. 23.3A).14,25 Reconstructions in the sagittal and coronal planes may further help define the nature of the injury (Fig. 23.3B and C).25 Determining the level of trauma may be difficult in SCIWORA patients. In these cases, the neurological examination is critical in evaluating the appropriate level to be studied.17 The evaluation can also be conducted by the use of magnetic resonance imaging (MRI).31 Approximately 10% of patients with a cervical spine fracture have a second associated, noncontiguous vertebral column fracture; therefore, a complete radiographic assessment of the entire spinal column is warranted.5,14 The exceptions to early CT after the initial lateral radiographs have been obtained are patients with an obvious facet fracture-dislocation injury.21 These patients may benefit from early reduction of the fracture and realignment of the cervical spine as long as rostral injuries, especially injuries to the craniocervical junction, are ruled out. Three-dimensional CT can be useful in the evaluation of complex cervical spine fractures and particularly in operative planning (Fig. 23.3D).32
The debate over the most appropriate workup for cervical spine injury in an asymptomatic trauma patient has resulted in several guidelines to minimize the cost and radiation exposure to patients.33 According to the Guidelines from the AANS/CNS Joint Section, trauma patients who meet the following criteria do not require x-ray evaluation of the cervical spine: (1) normal neurological examination and a Glasgow Coma Scale (GCS) score of 15, with no delayed or inappropriate responses, (2) not intoxicated, (3) no neck pain or midline tenderness, and (4) no significant distracting injury such as long-bone fracture or visceral injury.34 Symptomatic patients who do not meet these criteria should undergo a full radiographic assessment of the cervical spine.
Alternatively, the Canadian C-spine rules can be applied as a guideline to minimize the use of radiographs in the evaluation of alert and stable trauma patients when cervical spine injury is a concern.31,35
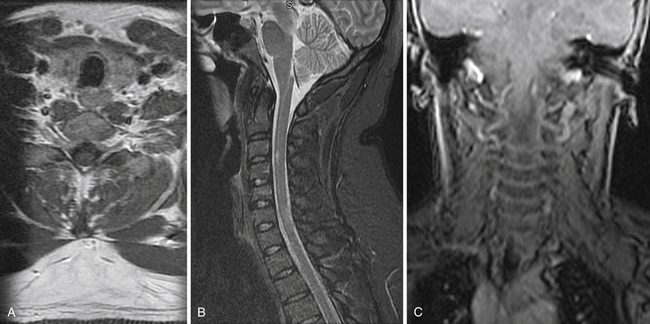
MRI is an extremely useful tool in the assessment of patients with a cervical spine injury and may identify injuries, such as disk herniations and ligamentous injuries, not seen on plain radiograph or CT. MRI provides a longitudinal assessment of the spine and spinal cord with views in the axial, sagittal, and coronal planes (Fig. 23.4).5,10,14,25,36–38 MRI may be the only imaging modality on which an abnormality is found in patients with SCIWORA, because ligaments, soft tissues, and neural elements can be imaged with superior detail. Hematomas within the spinal canal will not be identified on plain radiograph and may even be missed on CT but are readily identified on MRI.10,37,39 Although MRI is extremely sensitive for ligamentous injury, it cannot be used alone to diagnose an “unstable” injury.35
In the case of cervical trauma but no demonstrable fracture or dislocation injury on the initial standard cervical spine x-ray and CT studies, flexion and extension lateral cervical spine views are important additions to the radiographic assessment. Dynamic flexion-extension views may determine the presence of subluxation injuries or abnormal ligamentous laxity in patients who have persistent post-traumatic neck pain.5,14 In the obtunded or unconscious patient, flexion and extension may be performed under fluoroscopy and may detect a previously unrecognized injury, although its clinical significance is uncertain.40,41 Fluoroscopy is probably indicated only in patients with high-risk injuries such as high-speed motor vehicle accidents, falls over 3 m, major associated injuries, or vehicle crashes involving a death at the scene, because low-risk injuries have only a 0.2% incidence of cervical spine injury.42 MRI can be performed in flexion and extension, a technique that may be useful in identifying positional subluxation or compression of the cervical spinal cord in select cases.25,37,38
Management
Atlanto-Occipital Dislocation
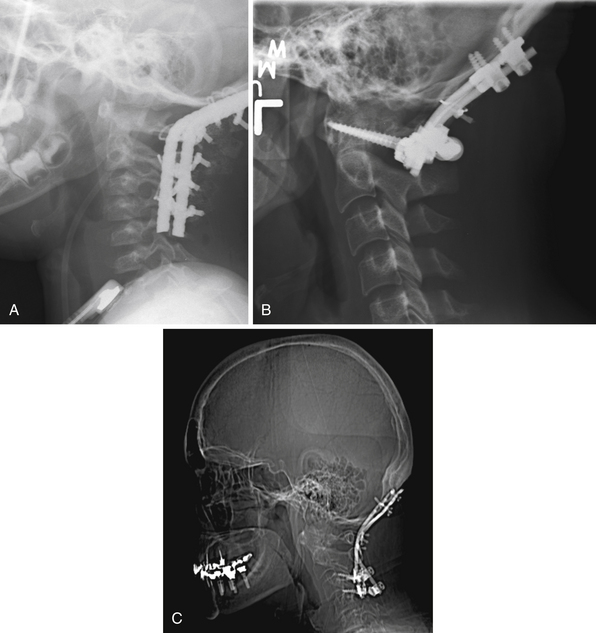
Traumatic atlanto-occipital dislocation (AOD) is associated with a high incidence of neurological morbidity and mortality.39,43–48 The mechanism and amount of force required to disrupt the atlanto-occipital junction are often fatal to victims of this type of injury. Historically, AOD injuries were deemed uncommon. More recent autopsy reports indicate that AOD accounts for 6% to 8% of all traffic fatalities. Of cervical spine injury-related deaths, 20% to 30% are the result of AOD.49–51 Given recent advances in the diagnosis and management of AOD, as many as 20% of survivors with this type of injury have a favorable functional outcome if therapy and immobilization are instituted promptly (Fig. 23.5).35,39,43–47
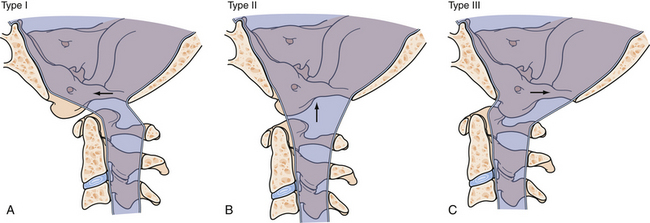
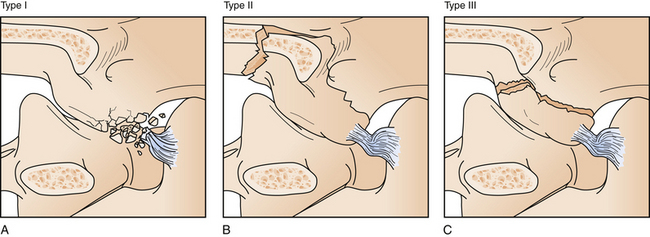
A classification scheme for the types of AODs describes anterior (type I), longitudinal (type II), and posterior (type III) dislocations based on the movement of the occiput with respect to the cervical spine (Fig. 23.6).
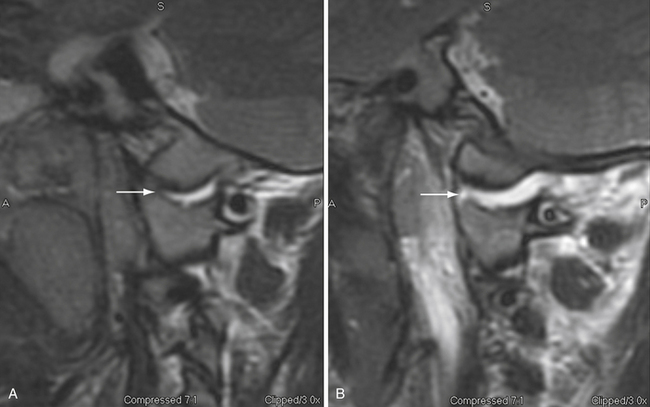
On the basis of class III evidence, The Guidelines for the Management of Acute Cervical Spine and Spinal Cord Injuries recommend applying the Harris method to a plain lateral cervical radiograph to recognize AOD. Since the publication of these guidelines, several groups have documented the use of CT as the diagnostic imaging of choice in patients suspected of having AOD.31,52–54 Based on these studies a basion-dens interval (BDI) (with 10 mm as the cutoff) and the occipital condyle-C1 interval (CCI) (>4 mm is abnormal) are the diagnostic tests of choice.53 It should be emphasized that AOD is a highly unstable injury and can be missed on any imaging modality if normal alignment is temporarily restored. MRI can be an important adjunct in the diagnosis of this condition.35
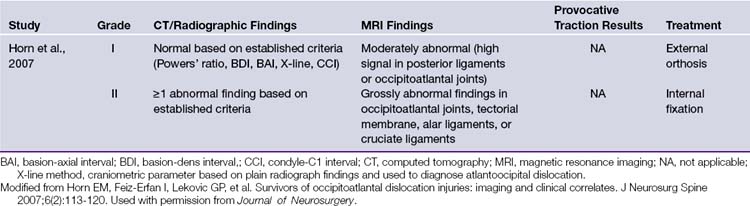
Our treatment paradigm for AOD is based on the recommendations from the largest published series of AOD patients (Table 23.3). Grade I injuries are those with “normal” BDI and CCI (Fig. 23.7) and equivocal MRI findings such as high posterior ligamentous or occipitoatlantal signal and mild to no signal change at the occipitoatlantal joint. In this population, nonoperative management with a halo or collar is adequate. Grade II injuries are defined by a minimum of one abnormal finding on CT-based criteria or grossly abnormal MRI findings in the occipitoatlantal joints, tectorial membrane, or alar or cruciate ligaments. Effective surgical stabilization of these patients requires open reduction and internal fixation (ORIF) from the occiput to the upper cervical spine.39,43–45 Fixation can be achieved with one of several types of instrumentation (Fig. 23.8) and must be supplemented by allograft or autogenic bone to provide long-term stability.
Occipital Condyle Fractures
Occipital condyle fractures (OCFs) are frequently missed on plain radiographs. With almost universal use of CT scans of the occipitocervical junction in the evaluation of trauma patients, these injuries are now being recognized with increased frequency.55 The true prevalence of OCF is unknown, but most authors have concluded that it is probably more common than typically realized.4,5 The reported incidence of OCF ranges from 4% to 19%, with a mean age of presentation of 32.4 years (range, 7 months to 88 years) and a male predilection of 2:1.56
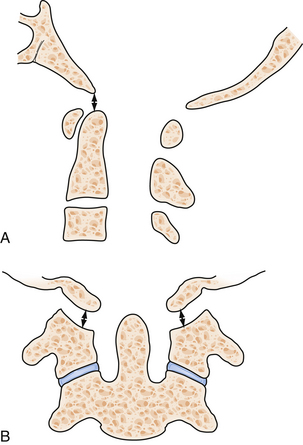
OCFs commonly occur as isolated injuries.28,29,57 The presence of a retropharyngeal hematoma on a lateral cervical radiograph may be the only clue that serious craniovertebral insult has occurred.58–60 Based on CT-based anatomical studies, Anderson and Montesano have classified these fractures (Fig. 23.9).61 Type I fractures (axial load and comminuted fractures) and type II fractures (extension of a skull-base fracture) are usually considered stable if isolated. Thus, symptomatic treatment is indicated and may include external immobilization in a collar.62 Type III injuries (avulsion of a condylar fragment by the alar ligament) may be unstable and require rigid external immobilization in a collar or halo or even ORIF, if other injuries such as atlantoaxial instability are present.62 Patients not treated may develop lower cranial nerve palsies, which still have a significant chance of resolving with immobilization.63
The need for surgical intervention to treat OCF is rare, and conservative management of all isolated OCFs is generally supported, even in cases of brainstem compression with neurological injury. Bilateral OCF can represent a unique presentation of AOD and needs to be evaluated carefully.35
Atlas Fractures
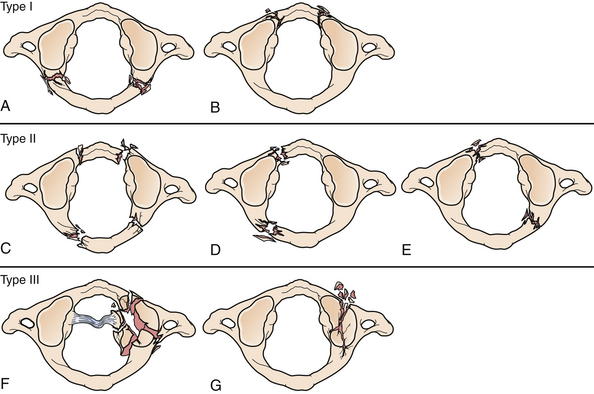
The atlas is the first cervical vertebra (C1) and bridges the occiput with the axis, the second cervical vertebra (C2), and the rest of the cervical spine.64 The position of the atlas and its ring shape make it vulnerable to a number of different fracture patterns. Fractures of the atlas account for 3% to 13% of all cervical spinal injuries.65,66 Injuries to C1 are mostly isolated, but 40% to 44% are associated with fractures of C2.65 Owing to the wide spinal canal at the level of C1, a neurological injury in the region is rare. Atlas fractures can be observed in various patterns and multiple classification schemes exist. The one used most commonly is the classification first presented by Jefferson67 and later modified by Gehweiler and associates68 (Fig. 23.10). In this modified classification scheme, type I fractures involve only the posterior arch. Only the anterior arch is involved in type II fractures. In type III fractures the posterior arch is fractured bilaterally, and there is an associated unilateral or bilateral anterior arch fracture. The classic Jefferson fracture is a type III atlas burst fracture. In this case the lateral masses are displaced laterally. The classic Jefferson fracture is the most frequent fracture pattern of C1, and it is caused by axial loading of the atlas. Type IV fractures involve the lateral mass, and type V fractures are transverse anterior arch fractures. Congenital abnormalities of the C1 ring can be mistaken for a fracture in some cases and MRI can be used in these cases to assess the affected area for edema within the bone.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree