Intervertebral Disk Disease
Intervertebral pathology of the pediatric spine is uncommonly encountered. The most frequent pathologies seen are herniated nucleus pulposus and diskitis/osteomyelitis, but other, less frequent diagnoses have been reported, such as inflammatory diskitis and conditions with neoplastic etiologies, such as chondrosarcoma and chordoma. Neoplastic conditions of the intervertebral disk space are extremely rare and are further discussed in another chapter. Pediatric disk pathology also includes adjacent processes that impact the disk space, such as spondylolysis and spondylolisthesis, which are further addressed in this chapter. Given the infrequent presentation of such pathology in children, diagnoses are often delayed, and a high index of suspicion should be raised to ensure a timely diagnosis.1–3
63.1 Developmental Anatomy and Embryology
The embryogenesis of the spine has been well described.4 At about 4 weeks of gestation, mesenchymal cells migrate medially from the sclerotomes to surround the notochord and form the perinotochordal sheath. The sheath differentiates into alternating dense and loose areas; the loose areas become the vertebral bodies, and the dense areas become the disks. The notochord regresses completely within the vertebral bodies but persists in the disks until it ultimately undergoes mucoid degeneration to form much of the nucleus pulposus. The peripheral cells of the nucleus blend with the perinotochordal mesenchyme to form the annulus fibrosus. By the end of embryonic development (8 weeks), the distinction between the disks and bodies is clear, and notochord segmentation and formation of the annulus have begun (▶ Fig. 63.1). By 24 weeks, the end plates can be identified, and fibroblasts have begun to invade the nucleus.5
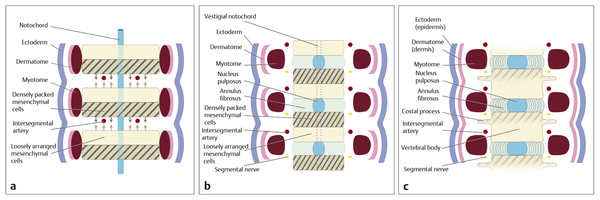
Fig. 63.1 Artist’s illustration of the embryologic development of the spinal column. The somites forming the vertebral bodies divide, with adjacent rostral and caudal halves fusing to form the vertebral body and thus create the intervertebral disk space.
(Printed with permission of Baylor College of Medicine.)
Both the annulus and the nucleus pulposus are well defined at birth. The annulus consists primarily of type 1 collagen fibrils. They are arranged in concentric lamellae that run obliquely between adjacent vertebrae and attach to either the vertebral bodies or the cartilaginous end plates. The annulus also contains a small amount of proteoglycan and a few cells. The nucleus pulposus is composed mostly of type 2 collagen fibrils and a few cells embedded in a hydrated proteoglycan matrix. The proteoglycan molecules consist of a protein core studded with glycosaminoglycans. Chondroitin sulfate and keratin sulfate are the glycosaminoglycans most commonly found in the disk. The proteoglycan molecules can bind to hyaluronate to create large aggregates; aggrecan is the predominant form.6 Other collagen subtypes are found throughout the disk, but they occur in small quantities.6,7 Blood vessels can be found in the disk for the first several years of life. They disappear gradually and are absent by early adulthood.8
With normal aging, changes occur in the composition of both the nucleus and the annulus.6,8–10 These changes are thought to be due to the mechanical stresses imposed on the disk as well as the relatively inefficient provision of nutrients to the cells in the disk caused by the poor vascularity of the area. Over time, there is progressive dehydration of the nucleus, and degenerative granules develop in the fibrocartilage. There are areas of neovascularity and chondrocyte proliferation. Tears can be found in the annulus and the end plate. In addition, the chemical composition of the disk changes.6,10,11 The amount of proteoglycan in the nucleus decreases. The large aggregate molecules fragment, more keratin sulfate is present, collagen subtypes change, and inflammatory mediators can be detected. Interestingly, some of these changes can reliably be seen as early as 11 years of age.8 Such long-term changes explain, at least in part, the increasing incidence of disk disease associated with aging. Nevertheless, degenerative disk disease does occur in some young people.
There is growing evidence that genetic factors play a significant role in the development of disk disease. Patients with a positive family history are up to five times as likely as are those without to have a herniated lumbar disk before the age of 21 years.12 Disease clustered in families has also been described. Scapinelli has reported eight siblings who had herniated lumbar disks; one of their parents also had disk disease. He suggested that, at least in some cases, an autosomal-dominant gene might cause disk herniation.13 Animal studies support this notion. Transgenic mice with mutations of the genes that produce either type 9 collagen or aggrecan have an extremely high incidence of disk disease.14,15 Similar findings have been reported in humans. For example, two Finnish studies reported variations in the collagen 9 alleles of persons with and without disk degeneration.16,17 Kawaguchi et al have described aggregan abnormalities in patients with multilevel disk degeneration.18,19 In addition, variations in the gene coding for vitamin D receptor and matrix metalloproteinase 3 have been linked to disk degeneration.20–23
63.2 Degenerative Disk Disease
Disk herniation is usually a pathologic process associated with degenerative disease and is assumed to be multifactorial, influenced by environmental and genetic factors.24 Disk herniation also occurs in the pediatric population, but the incidence is much lower than in adults.1 The number of cases requiring surgical treatment is 5.5 per 100,000 person-years in the population less than 25 years old, compared with 128 cases per 100,000 person-years in the 40- to 45-year-old age group.25
63.2.1 Clinical Presentation
The clinical presentation of lumbar disk herniation in children is similar to that described in adults; common symptoms, in up to 50% of patients, include lumbar radiculopathy out of proportion to low back pain and motor and/or sensory loss1,26–30 (▶ Fig. 63.2). However, it is not clear that the findings in adult disk herniation can be applied to a similar management strategy in the pediatric population because the structural properties of disks and environmental exposures differ between children and adults.1,31
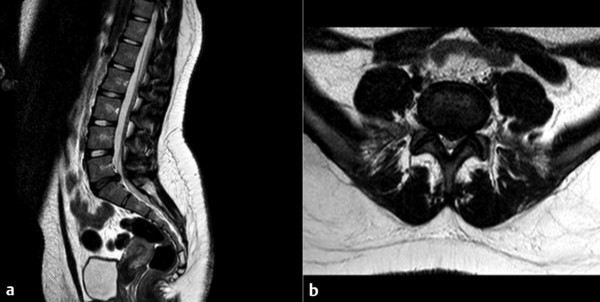
Fig. 63.2 (a) Midsagittal and (b) axial magnetic resonance images of the lumbosacral spine show a central disk herniation at L5–S1 associated with a “black” degenerated disk.
63.2.2 Treatment
Recent reports have indicated that cohorts of adult patients who undergo surgical or conservative treatment for lumbar disk herniation exhibit similar long-term outcomes, but the outcome is unknown in children because the treatment has not been studied in the pediatric age group.32 In the largest series of pediatric patients undergoing lumbar microdiskectomy to date, Cahill et al1 noted that although pediatric patients may not respond as well to conservative treatment as adults do, a significant proportion of them still do respond; therefore, one should attempt conservative therapy before considering surgery unless neurologic motor deficits require a more urgent operation. There have been limited reports of case series encompassing traditional open diskectomy and modern microdiskectomy in pediatric patients.1,28–30,33,34
Our small case series of six children35 indicates that minimally invasive surgery for lumbar disk herniation in the pediatric population is a safe and efficacious procedure. The average blood loss was minimal, and the majority of patients were discharged home on the same day as surgery or the first postoperative day. The lumbar incision is about 22 mm in length, a reported cosmetic benefit. Patients are usually mobile several hours after surgery, although we limit strenuous physical activity for 12 weeks. Athletes were able to return to competitive sports after this period of activity restriction. In our series, there were no postoperative complications, including cerebrospinal fluid leak or recurrence of disk herniation; however, this may be due to the small number of patients who have undergone minimally invasive surgery and our lack of long-term follow-up.
Although there were no complications in our pediatric series, early postoperative complications reported by others in the literature include wound hematoma (1 to 4%) and delayed wound healing (3%).26,32,35 Postoperative infection, such as wound infection and diskitis secondary to lumbar spine surgery, is rare in children and adolescents.29,36,37 There have also been reports of narrowing of the disk space, foraminal stenosis, and adjacent disk degeneration after diskectomy in the pediatric population, similar to results found in the adult population.27,37–40 Moreover, the rate of reoperation can be as high as 24% after extended follow-up.26,33,41
63.3 Traumatic Disk Disease
Posterior vertebral rim fracture, a fracture of bone fragments at the posterior rim of the vertebral end plate with an associated disk herniation, has been given several names: posterior marginal node; limbus fracture; fracture of the vertebral rim, ring, or end plate; epiphyseal dislocation; and apophyseal ring fracture42–49 (▶ Fig. 63.3). The mechanism of vertebral end plate fractures is not completely known. However, most authors have postulated that the pathogenesis of these fractures is trauma or strenuous physical activity.

Fig. 63.3 (a) Midsagittal computed tomographic scan of the lumbosacral spine shows an L1–L2 apophyseal ring fracture associated with disk herniation. (b) Midsagittal and (c) axial T2-weighted magnetic resonance images of the lumbosacral spine demonstrate L1–L2 disk herniation and significant lumbar canal stenosis.
63.3.1 Clinical Presentation
Young patients may present with a back injury50 associated with disk herniation. The intervertebral disk is attached to the end plate by Sharpey fibers, and the end plate is separated from the remainder of the vertebral body by a cartilaginous growth plate that is replaced by bone only at 18 to 25 years of age. After the apophyseal ring of the end plate ossifies in the immature spine (typically between the ages of 10 and 15 years), this cartilaginous junction is relatively weak and susceptible to compressive and tension stresses.51,52 Disk herniation through the cartilaginous plate and fracture or fragmentation of the ring apophysis can occur together in response to shearing or recurrent stress.53,54
Conventional X-rays and/or computed tomography (CT) may define the bone fragment, associated disk herniation, vertebral defect, and the severity of underlying spinal stenosis.53,55,56 Magnetic resonance (MR) imaging may also show the avulsed fragment and a defect in the posterior vertebral rim. Associated disk degeneration and herniation are usually present, and the spinal canal may be stenotic.54,55,57 The Epstein classification55 of posterior vertebral rim fractures, although seldom applied, demonstrates the range of radiographic appearances of these injuries. Type I fractures are simple avulsions of the posterior cortex of the end plate; they are so thin that no obvious defect is present in the vertebral body, although an arcuate fracture fragment is visible. Type II fractures are similar in position but include medullary bone and a defect in the vertebral body. Type III fractures are small and lateral. Type IV fractures run the full height of the vertebral body and extend to both vertebral end plates50,55 (▶ Fig. 63.4).
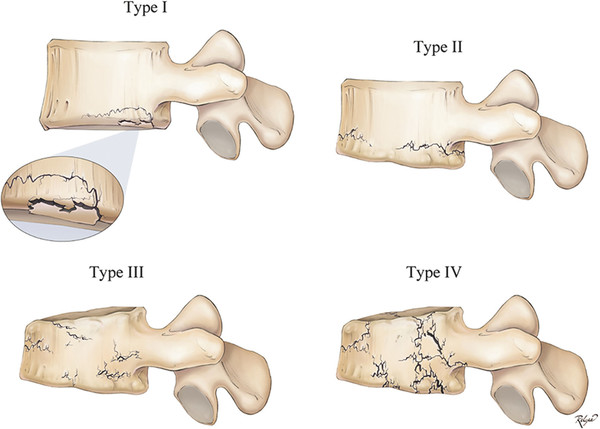
Fig. 63.4 The Epstein classification of posterior vertebral rim fractures. Type I fractures are simple avulsions of the posterior cortex of the end plate—so thin that no obvious defect is present in the vertebral body, although an arcuate fracture fragment is visible. Type II fractures are similar in position but include medullary bone and a defect in the vertebral body. Type III fractures are small and lateral. Type IV fractures run the full height of the vertebral body and extend to both vertebral end plates.
The differential diagnosis includes ossification of the posterior longitudinal ligament, disk calcification, osteophyte formation, and disk herniation. The most important diagnostic features are the vertebral defect and the bone fragment.
This condition usually affects patients in adolescence and early adulthood, with a male-to-female ratio of 2:1.55 The true incidence of end plate fractures associated with disk herniation remains unknown, but the condition is increasingly becoming recognized.58 Vertebral rim fractures may be asymptomatic. Symptomatic patients may initially present with back and leg pain, reduced lumbar movements, and restricted straight leg raise, similar to adolescents with disk herniation; motor and bowel and bladder dysfunction are usually late findings.53,55,56 Older adult patients may present with neurogenic claudication due to pre- or coexisting lumbar stenosis.55
63.3.2 Treatment
Not all patients with a posterior vertebral rim fracture require surgery. In a series of 21 patients,59 57% responded well to conservative treatment. However, if a patient has symptoms of radiculopathy or neurogenic claudication, the treatment of choice has been diskectomy with removal of the fracture fragments.42,55 In this case, the standard diskectomy exposure may not allow adequate removal of the fracture fragments or decompression of the spinal canal, increasing the risk of surgery. Based on our experience, we advocate simple decompressive laminectomy alone to treat pediatric patients who have neurogenic claudication associated with posterior vertebral rim fractures. Our patients experienced good relief of preoperative symptoms and a satisfactory functional outcome. Overly aggressive laminectomy that weakens the pars interarticularis and subsequently destabilizes the vertebral column should be avoided.
63.4 Inflammatory Disk Disease
Pediatric idiopathic/ inflammatory intervertebral disk calcification is an uncommon entity. It affects the intervertebral disks and adjacent vertebral body and musculoligamentous structures, resulting in local pain or sensorimotor disturbances.60 The etiology of pediatric idiopathic/inflammatory intervertebral disk calcifications is unknown, although associated fever, pain, and stiffness suggest an inflammatory condition. The clinical course is usually benign and self-limited, with the fever and pain resolving spontaneously within weeks or months61–71; calcification of the disk space is seen at the end of the inflammatory phase.
63.4.1 Clinical Presentation
A recent review72 of pediatric idiopathic/inflammatory intervertebral disk calcification found a male predominance (male-to-female ratio of 8:5). Most patients are between 5 and 12 years of age. The lower cervical spine is most frequently affected, with 50% of the cases of intervertebral disk calcification occurring in the cervical spine.65 In particular, almost all patients with cervical lesions (99.8%) are symptomatic, whereas all patients with lumbar lesions are asymptomatic.
Abnormal levels of inflammatory markers are found in half of the patients who undergo laboratory examination. The erythrocyte sedimentation rate (ESR) is the most sensitive indicator, elevated in more than 90% of patients. Considering also that more than 70% of symptomatic patients had muscle pain, an inflammatory etiology for pediatric idiopathic/inflammatory intervertebral disk calcification seems likely.
63.4.2 Treatment
In a review of the literature with more than 300 reported cases of pediatric idiopathic/inflammatory intervertebral disk calcification, only 7 patients were treated with surgery.71,73–77 Most surgically treated patients had a good outcome except for 1 patient with a permanent neurologic deficit.75 On the other hand, all patients who were treated conservatively showed good functional outcome. Neither the surgical indication nor the purpose of surgery has been established in the treatment of pediatric idiopathic/inflammatory intervertebral disk calcification. Nerve root or spinal cord compression by a calcified disk may not be considered an absolute indication for surgical intervention.78 Conservative management seems to be the mainstay of the treatment for pediatric idiopathic/inflammatory intervertebral disk calcification except in the uncommon patients presenting with acutely progressive and severe neurologic deficits.60
63.5 Spondylodiskitis/Osteomyelitis
Pathogens commonly encountered in children include Staphylococcus aureus, followed by Streptococcus pneumoniae and Salmonella species.2,79 Although various hypotheses of trauma and inflammation have been proposed, disk space infection is commonly thought to arise from infection at a prior site that has spread via three possible routes: hematogenously, by direct innoculation, or by direct extension. Almost 50% of children will have had a prodromal illness related to their disk space infection,80 and immunosuppression is a reported risk factor. In children, blood vessels are present in the annulus fibrosus, and the vessels within the vertebral body typically are anastomotic, but as in adults, there are no vessels or lymphatics within the nucleus pulposus. These anatomical variations have been proposed as a reason for the preferential localization of bacterial infections to the intervertebral disk space.
Spondylodiskitis is less commonly encountered in children than in adults and has a bimodal distribution (0 to 2 years and older than 10 years). It affects mainly the thoracic and lumbar spine.79–81 Diagnosis can often be delayed up to 4 to 6 months as a consequence of the low incidence and vague presentation in children.2,3 Most commonly, children present with back pain, but nonspecific symptoms are often the only presentation, frequently without fevers. Very young children with diskitis often may refuse to walk, show regression of ambulatory motor skills, display the Gowers sign, or refuse to sit.82,83 Several authors have proposed categories of symptoms for children presenting with diskitis: back pain, hip and leg pain, meningeal symptoms, abdominal symptoms, and “irritable child” syndrome.81,84 If epidural extension is present, children may present with neurologic compromise as well.
Laboratory values (complete blood cell count, ESR, C-reactive protein [CRP]) and blood cultures should be routinely obtained, but they are often normal or only mildly elevated.80 Blood cultures will often be positive early in the course of the illness, but given the delay in diagnosis, often only 50% are diagnostic. Very early in the course, plain radiographs may be negative because it typically takes 2 weeks to a month before disk space narrowing becomes apparent.3 The initial evaluation should include MR imaging of the entire spine with contrast. Both MR images and bone scans will reveal the abnormality, but MR imaging generally demonstrates the problem somewhat earlier.85 Technetium 99 bone scans will identify the problem 7 to 12 days after the onset of symptoms but are nonspecific, and distinction between inflammatory and neoplastic processes is required.86,87 Given the vascular supply in the pediatric spine, bacterial infections typically involve the disk space, and the isocenter of the infection can often be localized to the intervertebral disk space. If the disk spaces appear relatively preserved or uninvolved, concern for tuberculous infection should be raised88 (▶ Fig. 63.5).
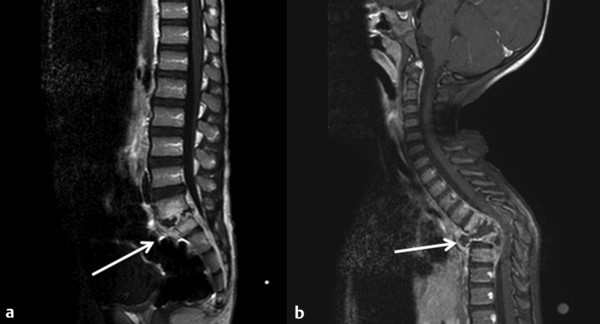
Fig. 63.5 (a) Sagittal postcontrast magnetic resonance (MR) image of the lumbar spine showing a pyogenic infection centered at the disk space with epidural extension (white arrow). (b) Sagittal postcontrast MR image of the thoracic spine of a patient with a tuberculous infection shows relative preservation of the adjacent disk spaces but significant involvement of the vertebral bodies (white arrow).
In the pediatric population, the treatment is controversial because most spondylodiskitis infections have a relatively benign course. If a pathogen is not identified, a CT-guided biopsy should be considered before the initiation of antibiotic treatment unless clinically contraindicated (declining or unstable clinical condition). However, given the self-limiting and indolent course of the infection in children, this is also controversial; many authors will treat an infection empirically and biopsy only a refractory case. Some authors advocate no treatment with observation only because the course is often self-limiting.89,90 More routinely, however, a course of intravenous antibiotics followed by oral antibiotics for 6 to 8 weeks is prescribed. Given the relatively high incidence of vertebral body wedging and loss of disk space height, the adjuvant use of immobilization through a cast or brace has been proposed by some authors. Surgery can also be considered for patients with refractory and progressive infections not responding to antibiotics, but those with nondiagnostic biopsies can typically be treated with broad-spectrum antibiotics for the duration of therapy. Epidural extension with neurologic compromise should be treated with emergent decompression and evacuation of the infection.
Given the usually self-limited course, outcomes for this pathologic entity are excellent.79,80 Kayser et al reported 10-year or longer follow-up in 20 children and noted that 80% had no symptoms with a “freely mobile spine,” whereas the remaining 20% had focal kyphosis and some restriction of spinal movement. All patients had radiographic narrowing of the disk space, and 40% had some degree of fusion across vertebrae.79
The reported indolent and self-limiting course, as well as the high incidence of nondiagnostic blood cultures and CT-guided biopsies, may be partially due to the inclusion of nonpyogenic infections. An entity known as chronic recurrent multifocal osteomyelitis (CRMO) or nonbacterial osteomyelitis (NBO) should be distinguished from spondylodiskitis/osteomyelitis. It is often associated with a syndrome of SAPHO (synovitis, acne, pustulosis, hyperostosis, and osteitis).91 Typically, CRMO is multifocal. Patients are often healthy between episodes, with symptoms extending beyond 6 months.92–94 Young girls between the ages of 4 and 14 years are more often affected (5:1), but the etiology is poorly understood.95,96 Most patients have palmoplantar pustulosis or psoriasis. Patients may have minor diagnostic criteria of normal or mildly elevated laboratory values (CRP, ESR), hyperostosis, other autoimmune diseases, and an associated family history. Radiographic images can mimic those of osteomyelitis, but other long bones are typically involved, such as the clavicle. Bone biopsies are sterile but demonstrate evidence of inflammation and/or sclerosis or fibrosis.92 Standard therapy involves the use of nonsteroidal anti-inflammatory drugs, but alternate medications, such as oral steroids, methotrexate, and bisphosphonates, have been reported with positive early results.97–100
63.6 Spondylolysis
Spondylolysis is to an abnormality in the pars interarticularis that is typically due to a stress or fatigue fracture. It is classified into five categories based on the presumed etiology: dysplastic, isthmic, degenerative, traumatic, and pathologic.101 The dysplastic and isthmic subtypes are most often represented in the pediatric population; dysplastic types are often associated with other osseous abnormalities and an elongated pars interarticularis, whereas isthmic subtypes are due to repeated trauma. The natural history is poorly understood, but it is generally thought to be nonprogressive. Fredrickson et al reported an incidence of 4.4% in asymptomatic schoolchildren at 6 years of age, which increased to 6% by 18 years of age.102 The increasing incidence may be related to mechanical motion and repeated stresses accrued with age. Increasing forces loaded onto the facets with hyperextension movements of the spine are believed to contribute to the development of spondylolysis. An increasing incidence (up to 47%) of spondylolysis among participants in elite athletic activities such as gymnastics, tennis, diving, and weight lifting has been reported.103–105 Furthermore, a hereditary predisposition appears to contribute to a higher frequency among family members, but specific genes have not been identified.106,107
Patients often present with low back pain after exacerbation with activity that does not resolve in an appropriate time frame. As the pathology progresses, focal hypertrophy of the synovium or an inflammatory reaction at the pars defect can develop that may extend to involve the adjacent nerve root, causing radiculopathic symptoms or signs. Patients may also have associated spondylolisthesis that may progress, further contributing to back pain.
The radiographic evaluation of a patient thought to have spondylolysis should begin with anteroposterior, lateral, and oblique radiographs (▶ Fig. 63.6). If only anteroposterior and lateral films are obtained, approximately 20% of defects are missed. The classic description of spondylolysis is that of La Chapelle—a radiolucency in the neck of a Scottish terrier (“Scottie dog sign”) seen on oblique views. If plain radiographs are nondiagnostic, CT of the lumbar spine is routinely then performed, followed by a bone scan. If the patient’s symptoms are long-standing (longer than 1 year), a bone scan is less likely to be useful. Read recommends single proton emission computed tomography (SPECT) for adolescents suspected of having spondylolysis because of this technique’s superior resolution and sensitivity.108
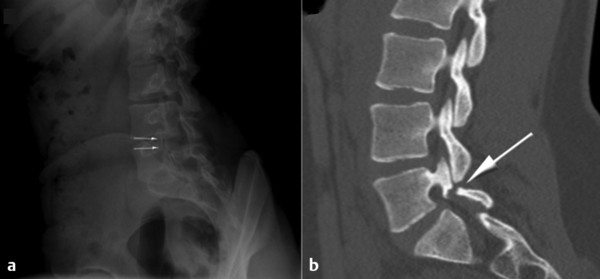
Fig. 63.6 (a) Oblique lumbar radiograph showing the pars defect (arrows) across the neck of the “Scottie dog.” (b) Sagittal computed tomographic scan showing the pars defect highlighted by the arrow.









