58 Intracerebral Hemorrhage
Clinical Vignette
There are two forms of intrinsic cerebral hemorrhage, primary ICH, which has a predilection to affect the striatum, thalamus, midbrain, pons, and cerebellum, and subarachnoid hemorrhage (Chapter 57). ICH comprises approximately 10% of all strokes in the Caucasian population and up to 20% in the Asian population. Over the past several years, improved treatment of hypertension has decreased the number of patients experiencing ICH.
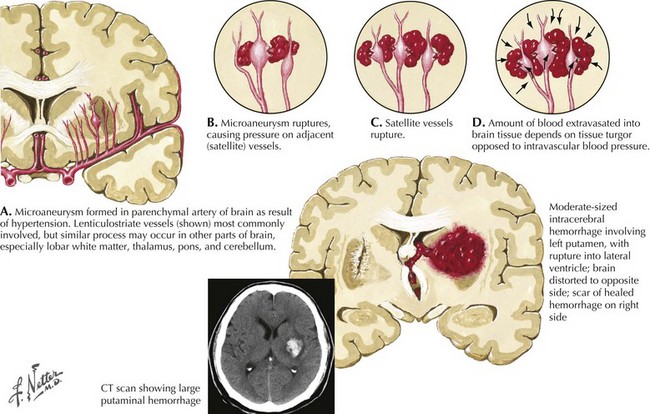
Pathophysiology of Hypertensisve Primary Ich
Intracranial hemorrhage is a rapidly evolving process that may progress over hours or days. The pressure effects of the initial hemorrhage lead to mechanical disruption and tearing of surrounding vessels with subsequent gradual expansion of the hematoma out from the original center. Rebleeding is the most feared early complication of ICH and occurs in approximately 40% of patients. Rebleeding usually occurs within the first 24 hours but, on occasion, has been reported up to a week later. The underlying pathological mechanism of primary hypertensive ICH is attributable to either the formation of miliary microaneurysms or primary arteriolar degeneration (lipohyalinosis and weakening of the blood vessel intima and media wall layers) (Fig. 58-1). The presence of miliary aneurysms is directly related to hypertension but is not necessarily the initial site of bleeding, and cases of hypertensive ICH outside the areas of microaneurysms have been noted. This suggests that degeneration of the arteriolar smooth muscle wall is likely an important factor in the evolution of ICH. Hypertensive intracerebral hemorrhages have a predilection to occur in the basal ganglia and the thalamus. The arterioles in these structures are likely more vulnerable to degenerative changes brought on by diffuse, large pressure pulses over time.
Clinical Presentation
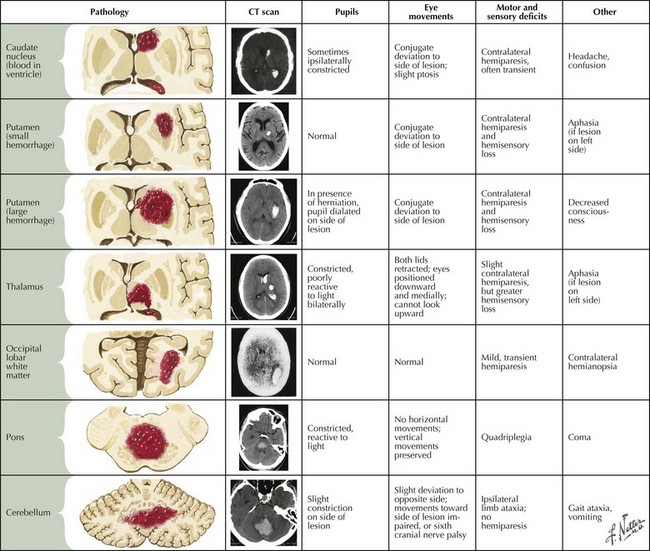
Intraparenchymal hemorrhages vary in presentation depending on the site of the bleeding (Fig. 58-2). In approximately 60% of patients, neurologic symptoms develop gradually or stepwise over a period of hours. To some extent, the location and size of the hematoma predict clinical outcome.
Deep Supratentorial Hemorrhage
Superficial Lobar Hemorrhages