♦ Preoperative
Imaging
- Magnetic resonance imaging (MRI) with or without contrast
- Establishes rostrocaudal location
- Helps with axial plane location of tumor versus cord tissue
- Presence of cystic caps may suggest ependymoma
- May show additional lesions (e.g., tumor or syrinx) elsewhere
- Establishes rostrocaudal location
- Computed tomography: may show calcification (more common with ependymoma)
- Helpful if instrumentation may be needed
- Myelography: does not show intramedullary details
- May have risk if complete block; consider C1-2 puncture
Equipment
- Typical
- Standard spine equipment
- Microinstruments
- Microscissors
- Microforceps
- Microbipolar cautery
- Microsurgical suction tubes
- Microneedle drivers (Castroviejo)
- Microforceps
- Standard spine equipment
- Operating microscope with bridge
- Consider having available
- Ultrasonic aspirator with small tip (for debulking larger lesions)
- Intraoperative ultrasound (may be helpful for localization)
- Lumbar drain kit (for cases with higher risk of dural leak)
- Dural patch material (e.g., AlloDerm, suturable DuraGen)
- Dural sealant (e.g., Tisseel, DuraSeal)
- Intraoperative ultrasound (may be helpful for localization)
- Monitoring generally used
- Somatosensory evoked potentials
- Motor evoked potentials
- Sphincter electromyography may be helpful for some lesions (e.g., conus)
- Preoperative marking
- Consider using to aid intraoperative localization for areas that are harder to image intraoperatively (e.g., mid-thoracic)
- Somatosensory evoked potentials
♦ Intraoperative
Anesthesia
- General anesthesia, attention to monitoring
- Dexamethasone 10 mg intravenous at start of case
Positioning/Approach
- Prone position (generally have operative area flat and at the highest point)
- Posterior midline incision
- Wide laminectomy generally used
- Midline dural opening
- Dural retracting sutures (e.g., 4–0 Nurolon)
- Arachnoid dissection
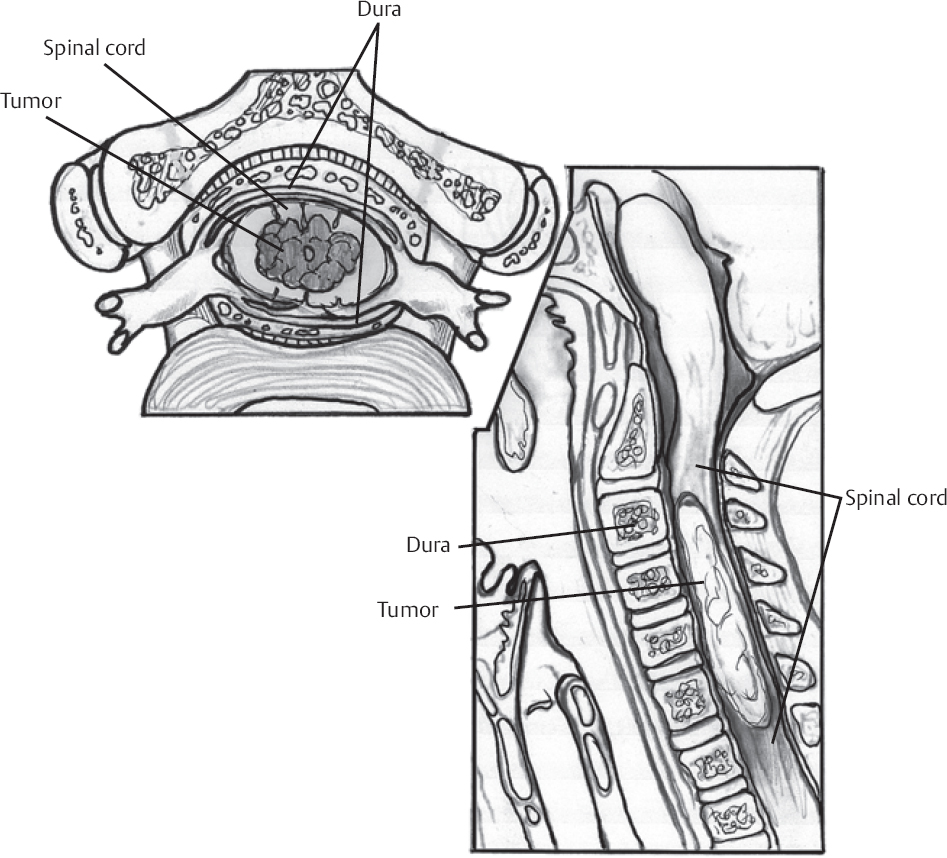
Tumor Resection (Fig. 132.1)
- Identify dorsal midline by visualizing exiting nerve roots bilaterally (cord often rotated by tumor)
- Identify tumor: usually identifiable below dorsal pia; ultrasound may be helpful
- Longitudinal pial incision (typically midline but can be paramedian; e.g., for lateral tumors that come to surface)
- Place pial sutures (5–0 or 6–0 Prolene) and gently secure laterally
- Drain cyst, syrinx, hematoma (if present)
- Biopsy tumor (recognize frozen section may be nondiagnostic)
- Internal debulking, with ultrasonic aspirator where appropriate
- Vessels clearly supplying tumor may be cauterized.
- Ventral vessels should never be cauterized, use Avitene, Surgicel, Gelfoam, or Surgifoam
- Since astrocytomas typically have poor plane, attempting to define planes to achieve full resection may be unsafe
Closure
- Watertight dural closure (with dural patch where needed)
- Consider using Duragen and/or Duraseal to reduce chances of postoperative cerebrospinal fluid leak
- Test dural closure with intraoperative Valsalva challenge
- The author generally avoids subfascial surgical drains but recognizes that there is some disagreement on this topic
- Consider muscle sutures to reduce dead space
- Meticulous fascial closure
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree