♦ Preoperative
- Review imaging (magnetic resonance imaging [MRI])
- Define rostral and caudal extent of the lesion
- Note location within the cord: myxopapillary ependymomas occur primarily at the conus and are histologically and clinically distinct
- Note enhancement pattern, presence of calcium, or hemorrhage within the lesion on noncontrast computed tomography and MRI; although benign lesions, ependymomas have a higher incidence of bleeding than other intra-medullary tumors
- Note presence of syrinx
- Review patient’s clinical course to ascertain chronicity of neurologic symptoms; ependymoma usually have a more indolent course than high-grade astrocytoma
- Review patient’s past medical and family history for genetic disease
- Von Hippel-Lindau disease is associated with intramedullary hemangioblastomas
- Neurofibromatosis type I is associated with intramedullary astrocytoma
- Neurofibromatosis type II is associated with intramedullary ependymoma
- Von Hippel-Lindau disease is associated with intramedullary hemangioblastomas
Equipment
- Basic spine tray
- High-speed drill (Midas Rex with AM-8 bit)
- 1- and 2-mm Kerrison punches
- Operating microscope with bridge
- Somatosensory evoked potential (SSEP) or direct evoked motor potential (DMEP) monitoring set-up
- Ultrasonic aspirator
- Microinstruments
♦ Intraoperative
Posterior Cervical Approach
- For lesions of the cervical cord or cervicothoracic junction
Posterior Thoracic Approach
- For lesions of the thoracic cord, cervicothoracic junction, or thoracolumbar junction
Posterior Lumbar Approach
- For lesions of the lumbar cord, thoracolumbar junction, or conus
Tumor Resection (Fig. 133.1)
- Standard laminectomy exposing the level above to the level below the lesion with patient in prone position
- Laminoplasty is performed in pediatric patients in an effort to foster long-term spinal stability
- Dura is opened in the midline and tented with 4–0 silk sutures laterally to the paraspinal muscles
- The operating microscope is brought into position
- The cord is inspected for any obvious signs of tumor
- Most intramedullary ependymomas are not apparent on the surface
- Typically, the tumor is first encountered at the site of maximal cord enlargement
- Ultrasonography may be used to confirm location of tumor or syrinx
- Most intramedullary ependymomas are not apparent on the surface
- Midline myelotomy is performed through the posterior median septum
- The dorsal midline is located between the two flanking dorsal root entry zones, which should be exposed
- The septum is also demarcated by the small veins exiting from the midline
- The dorsal midline is located between the two flanking dorsal root entry zones, which should be exposed
- The myelotomy should be carried over the entire rostral-to-caudal extent of the lesion
- The myelotomy is deepened with careful use of microforceps or dissectors
- Syrinxes, cysts, or sites of hematoma should be drained
- After identifying the entire dorsal aspect of the tumor, place pial traction sutures and weight them down with clamps to provide superior and lateral traction
- The extent and method of tumor resection will vary, depending on the pathology
- Ependymomas usually have a smooth, reddish gray, glistening tumor surface
- Traction on the surface of the tumor is used against the countertraction of the pial sutures
- Fibrous adhesions and feeding vessels between the spinal cord and tumor are cauterized and divided
- Internal decompression of larger tumors can be achieved with ultrasonic aspiration or laser
- The ventral and lateral margins of the tumor may be developed after central debulking
< div class='tao-gold-member'>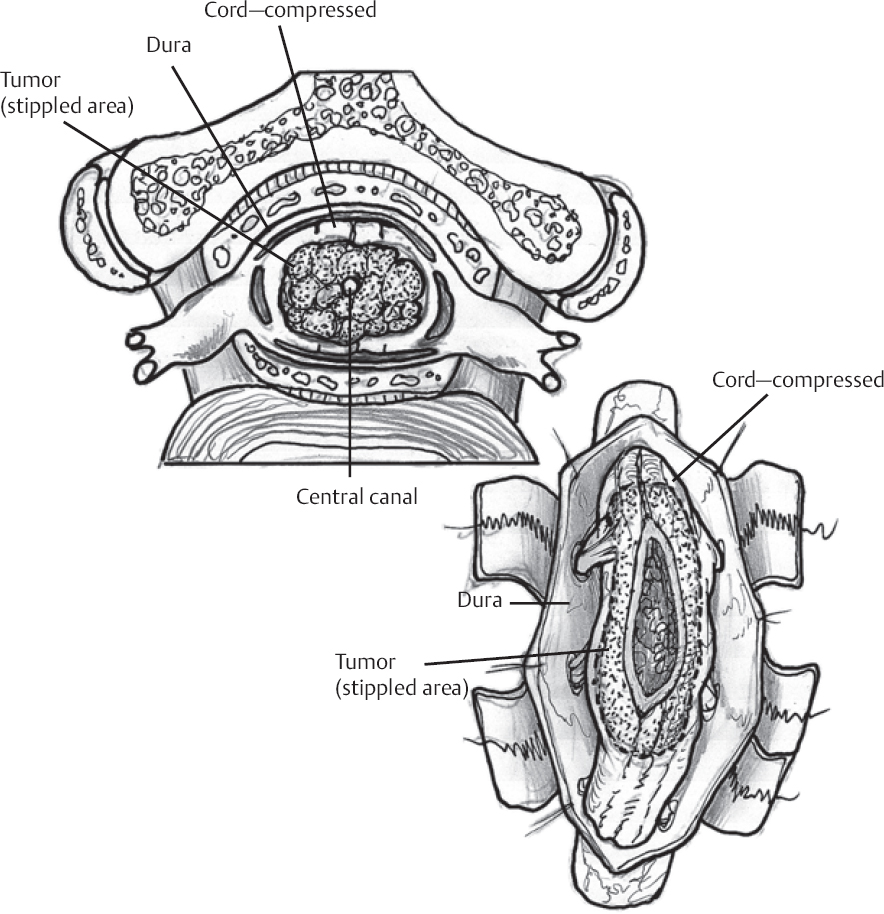 Only gold members can continue reading. Log In or Register to continue
Only gold members can continue reading. Log In or Register to continue
- Ependymomas usually have a smooth, reddish gray, glistening tumor surface








