Chapter 101 Intramedullary Spinal Cord Lesions
Surgery, once used for the diagnosis of intramedullary spinal cord tumors alone, now represents the most effective treatment of benign well-circumscribed tumors (which constitute the majority of intramedullary neoplasms).1–9 Long-term tumor control or cure, with preservation of neurologic function, can be achieved in most patients with microsurgical removal alone.2,5,10 The benign nature of most intramedullary neoplasms, advances in microsurgical techniques, early clinical diagnosis with MRI, and the ineffectual or inconsistent treatment response of most intramedullary tumors to radiation therapy largely account for the expanded role of surgery in the management of these lesions.4,11,12 Therefore, optimization of surgical treatment is the key to successful management of patients with intramedullary masses. This includes early diagnosis and aggressive primary treatment, the avoidance of technical and judgmental errors and their associated complications, and a strict adherence to contemporary microsurgical technique.
Patient Evaluation
The predominant benefit of surgery for an intramedullary tumor is prophylactic. Preservation, rather than restoration, of neurologic function is the most likely outcome after successful surgical treatment. In fact, significant improvement of a severe or long-standing preoperative neurologic deficit rarely occurs after a technically successful surgical excision. Surgical morbidity is also greater in patients with more significant preoperative deficits. This creates a therapeutic irony in which the risk of surgery is actually less in patients with minimal or no objective neurologic deficit. Thus, early clinical diagnosis and, if possible, definitive initial treatment are critical to successful clinical management of most intramedullary tumors. A therapeutic dilemma arises, however, in the asymptomatic patient in whom an incidental intramedullary spinal cord lesion has been discovered. A posterior column deficit is a common consequence of a dorsal median myelotomy; thus, some degree of morbidity often accompanies even the most successful surgical removal.13 In completely asymptomatic patients, therefore, observation with serial clinical and radiologic follow-up may be an appropriate management strategy. This is also true for patients with conditions such as neurofibromatosis or von Hippel-Lindau disease.
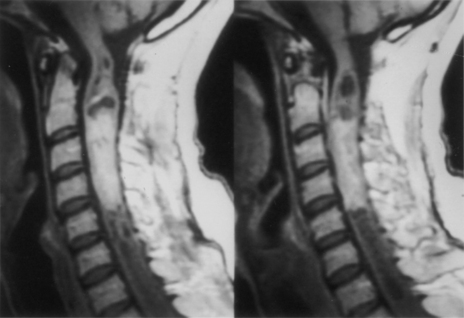
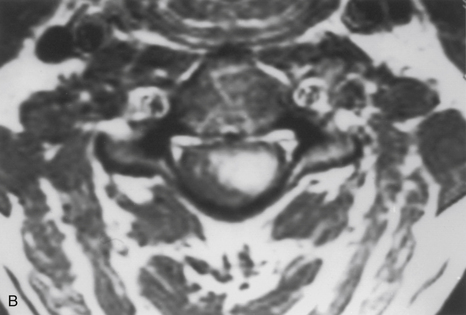
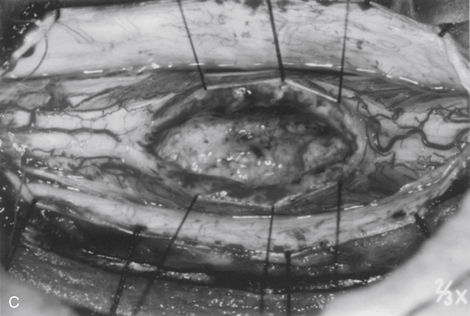
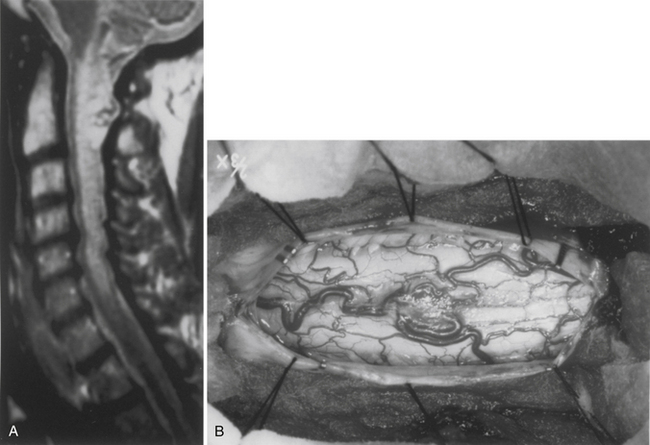
Because of the slow growth rate of benign tumors and the availability of MRI, most patients with intramedullary tumors are diagnosed before the onset of significant neurologic deficit. Gadolinium-enhanced MRI is the procedure of choice for imaging and preoperative evaluation of an intramedullary tumor. Spinal cord enlargement and tumor enhancement are the characteristic findings (Fig. 101-1). Polar cysts are often present. Ependymomas are usually symmetrically located and exhibit uniform tumor enhancement, whereas astrocytomas are associated with a more variable appearance with respect to tumor margins and enhancement patterns (Fig. 101-2). Prediction of these tumor types on MRI appearance is often inaccurate, predominantly because of the variability of presentation on MRI scans, and is therefore avoided because it may unfairly influence the surgical objective. Hemangioblastomas usually appear as intensely enhancing eccentric masses or nodules. There is often diffuse spinal cord enlargement that may extend a considerable distance from the tumor (Fig. 101-3). The cause of this tumor enlargement is most likely vasogenic edema.14
Patient Selection
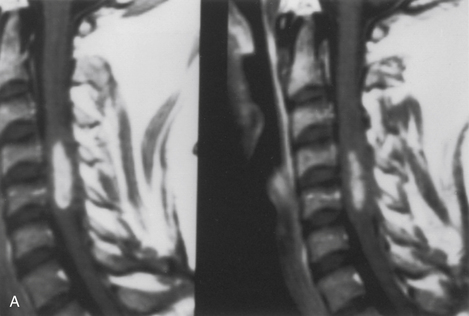
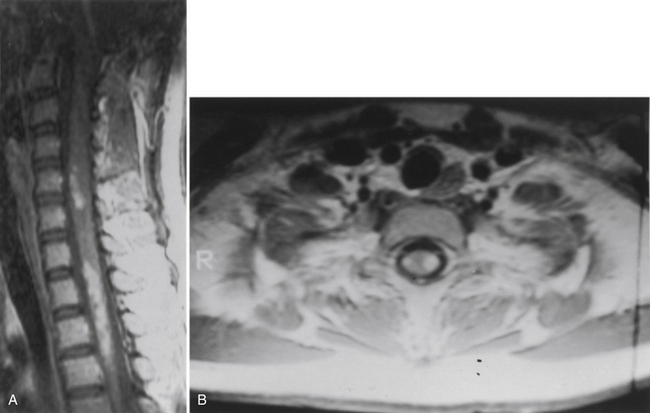
Whereas early diagnosis is routinely achieved with gadolinium-enhanced MRI, the sensitivity of MRI has far exceeded its specificity. Acute inflammatory conditions or demyelinating conditions such as multiple sclerosis or transverse myelitis are exquisitely imaged with MRI. These are not surgical lesions, and biopsy for diagnosis usually reveals only a nonspecific inflammatory response. This rarely provides a specific diagnosis, a prognosis, or treatment options. In most cases, patients with these conditions can be distinguished on the basis of clinical presentation and MRI appearance. These patients usually have symptoms of either acute or subacute onset of significant neurologic deficit. MRI typically shows patchy or focal gadolinium enhancement that may be confined to the white matter (Fig. 101-4). Spinal cord enlargement is subtle or, more likely, absent. In contrast, patients with benign intramedullary tumors usually experience a significant spinal cord enlargement with minimal, if any, objective neurologic deficit. Thus, a patient who shows symptoms of an acute or subacute onset of a significant neurologic deficit in the absence of obvious spinal cord enlargement usually harbors a nonsurgical inflammatory lesion.
Surgical Objectives
The most important factor influencing the surgical objective is the nature of the tumor–spinal cord interface. This interface can be assessed accurately only through an adequate myelotomy, which extends over the entire rostrocaudal extent of the tumor. Benign tumors, such as ependymomas and hemangioblastomas, although unencapsulated, are noninfiltrative lesions that typically exhibit a distinct tumor–spinal cord interface. Gross total removal is the treatment of choice in these cases. Astrocytomas are more variable. Unlike the consistently benign histology, circumscribed nature, and natural history of ependymoma and hemangioblastoma, astrocytomas are much more variable with respect to histology, physical characteristics, and natural history. Although some benign astrocytomas are well circumscribed and allow gross total resection, most exhibit variable infiltration into the surrounding spinal cord. This is often reflected in a gradual transition zone between the tumor and spinal cord. There is rarely a definitive dissection plane. Thus, whereas gross total resection may be achieved in some cases, the extent of removal is uncertain and poorly defined in most cases. Furthermore, more peripheral dissection beyond what is clearly tumor tissue risks loss of neurologic function from the resection of infiltrated, yet functionally viable, spinal cord parenchyma. The surgical objective for spinal cord astrocytomas remains unclear. Specifically, a correlation between the extent of resection and tumor control has not been definitively established.15,16 Because preservation of neurologic function, rather than complete tumor resection, is the more prudent treatment objective in these cases, tumor removal is limited to tissue that is clearly distinguishable from the surrounding spinal cord. Therefore, the extent of tumor removal varies. Diffusely infiltrative tumors without a definite mass are biopsied, whereas gross total resection may be possible in well-circumscribed examples. Variable degrees of resection account for the remainder of astrocytomas.
Cavernous angiomas are congenital vascular malformations that may appear as intramedullary mass lesions. Most of these lesions are well circumscribed and can be completely excised.17
Biopsy results may be particularly helpful in some instances. Identification of a histologically malignant tumor, for example, independently signals an end to the procedure because aggressive surgery is of no benefit for malignant intramedullary neoplasms.18 In other cases in which the tumor–spinal cord juncture may not be apparent, the confident histologic identification of an ependymoma reassures the surgeon that a plane must exist and that surgical removal should continue.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree