♦ Preoperative
Patient Evaluation
- Intrathecal baclofen (ITB) trial to assess response of spasticity or dystonia to test dose of baclofen delivered through lumbar puncture
- Neurologic evaluation: screening clinical criteria for appropriateness of therapy; can assist with determining extent of ITB therapy
- Physiotherapy evaluation: assist with screening assessment for spasticity; establish goals for post-ITB implantation
Review Imaging
- Presence of fusion mass, scoliosis, or other structural abnormalities may change the level of access to the intrathecal space
Special Equipment
- SynchroMed II implantable pump (Medtronic) for pediatric patients (20 or 40 mL capacity)
- Catheter with graded markings
- 14-gauge Tuohy needle
- Catheter passer/sheath
- Fluoroscopic x-ray machine
Anesthetic Issues
- General anesthesia
♦ Intraoperative
Positioning
- Patient in the left lateral decubitus position
- Most surgeons are right handed
- A significant number of patients have left upper quadrant gastrostomy tubes
- Use of a vacuum bean bag or tape can assist with maintenance of lateral position
- Most surgeons are right handed
- Subcutaneous pocket
- Epidermis is opened with a 8 cm horizontal incision approximately one fingerbreadth beneath the right costal margin
- Use needle tip electrocautery for opening subcutaneous tissue and fascia
- Fascia is opened between the external oblique muscle laterally and the abdominus rectus muscle medially to create a subfacial pocket.
- Epidermis is opened with a 8 cm horizontal incision approximately one fingerbreadth beneath the right costal margin
- Placement of intrathecal catheter (lumbar)
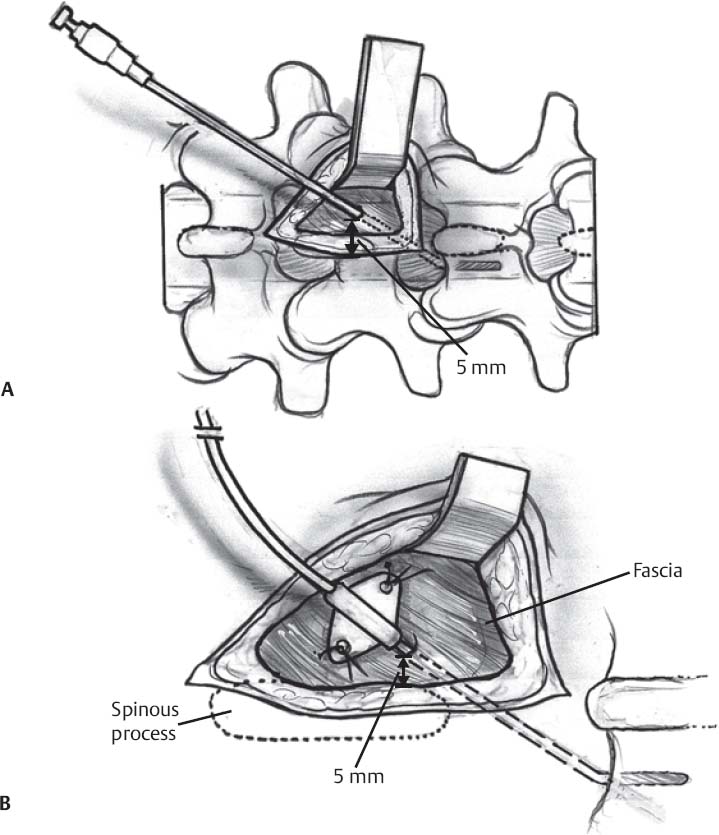
- Vertical skin incision at approximately at L4–L5 with dissection to level of lumbar fascia (Fig. 169.1A)
- Tuohy needle inserted 5 mm lateral to midline and directed obliquely one or two levels cephalad to access the intrathecal space (Fig. 169.1BA)
- Fluoroscopy is useful to direct the trajectory of the needle and to avoid multiple dural punctures
- The catheter is then placed at the appropriate level under fluoroscopic guidance.
- T10–T12 catheter tip position is used for spastic diplegia
- T1–T2 position for spastic tetraparesis
- C1–C2 for generalized secondary dystonia
- T10–T12 catheter tip position is used for spastic diplegia
- A pursestring suture is inserted into the fascia around the Tuohy needle, the needle and then the guidewire are removed, and the pursestring suture is tightened
- The catheter is secured with a nonabsorbable suture and silastic butterfly flap (Fig. 169.1B)
- Catheter placement in patients with fused spines requires preoperative planning. There are three possible techniques to address fusion.
- If there is an open interspace within the lumbar spine, placement can be done as described using fluoroscopic guidance.
- If the entire lumbar spine is fused, a hole in the fusion mass can be drilled, the catheter placed through the dura at the opening, and passed to the appropriate level.
- A cervical approach can be done through a 4 to 5 cm midline incision and limited laminectomy. The catheter is passed through a small dural opening and closed with a pursestring. The catheter tip is then advanced with fluoroscopy to the appropriate level.
- If there is an open interspace within the lumbar spine, placement can be done as described using fluoroscopic guidance.
- Tunneling and connection to subcutaneous pump
- Using a curved passer, the catheter tubing is tunneled anteriorly to the sub-fascial pocket.
- Cerebrospinal fluid (CSF) should be withdrawn from the end of the catheter after tunneling and ease of flow should be confirmed before attaching it to the pump.
- The catheter is then connected to the pump and secured with a nonabsorbable suture.
- The pump is then secured with nonabsorbable sutures within the pocket.
Wound Closure
- Pulse irrigation of wounds with saline solution; antibiotics or 100 ppm of iodine can be used if desired. Absorbable sutures for fascia and subcutaneous tissues, followed by Steri-Strips.
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree