INTRODUCTION
This chapter reviews a range of laboratory and imaging investigations with which an old age psychiatrist should be familiar. Physical illness has been shown to be present in 20-80% of psychiatric patient populations surveyed1. Physical illness of relevance to the presenting psychiatric symptoms is reportedly in the range 9-46%1. Concomitant medical disorder was found in up to 63% of psychiatric patients presenting to an emergency department2. However, a retrospective study demonstrated that only 0.8-4.0% of abnormal tests were clinically significant1 (defined as those that contributed to a diagnosis of a medical disorder not identified by history taking and physical examination and which led to a medical consultation or changed further management). Accordingly, some have argued against using routine batteries of tests1,2.
The older adult population may be an exception to this, as the chances of a physical illness presenting primarily with psychiatric symptoms is increased. Examples include delirium (infections, metabolic abnormalities, polypharmacy); dementia (thyroid disease, B12 deficiency); psychosis (substance withdrawal/toxicity, space occupying lesions in the brain); depression (anaemia, thyroid disease, some drugs, malignancy); mania (stroke, drug side effects); anxiety (thyroid disease, cardiac arrhythmia); and perceptual abnormalities (visual defects, migraine, temporal lobe epilepsy, withdrawal from drugs). Further, mental disorder may contribute to the onset of new physical illness or deterioration in an existing one due to factors such as self-neglect or cognitive difficulties.
Investigations should be guided by findings from history taking, mental state examination and relevant physical examination. Unlike in general medicine, the role of laboratory and other investigations is mainly supportive and to rule out an organic aetiology of psychiatric presentations. However, there are several other reasons for conducting physical investigations in the older patient (Table 23.1).
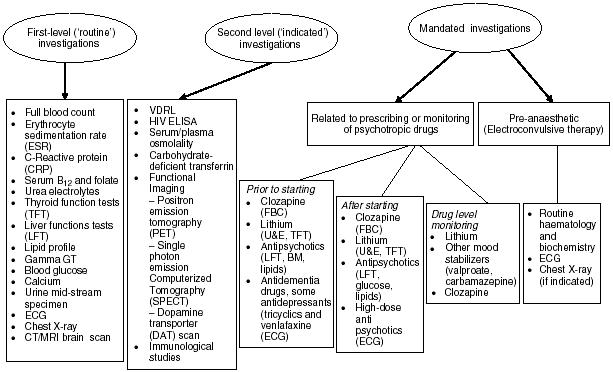
Ancillary investigations can aid diagnosis, especially in the dementias and in delirium. Many older patients have known physical comorbidity that requires further evaluation or are at high risk of common morbidities, which can affect management (ischaemic heart disease, anaemia, etc.). Because of self-neglect, those with dementia and depression may suffer under-nutrition and require investigation for this. Last, some psychiatric procedures and medication require preand/or post-testing (Figure 23.1).
Investigations may therefore be classified as primary or ‘routine’ (most patients receive them), secondary (indicated only in patients with certain clinical characteristics) and mandated (patients meeting certain criteria must have them) (Figure 23.1). The limitations of this approach should be recognized. Some tests (e.g. for neurosyphilis, see below) will show abnormal results very rarely but with important clinical implications. Others (e.g. full blood count or plasma viscosity) will often be slightly abnormal and of uncertain significance. A good deal of skill is required to interpret results in relation to a particular patient.
An example of an investigation of immediate relevance to management is a patient with a history of depression now presenting with what appeared to be a recurrence but also with recent confusion and difficulty in walking. On computerized tomography (CT) brain scan he was found to have a glioma. In another instance a patient with dementia deteriorated with poor appetite and weight loss. Investigations revealed anaemia and a markedly raised C-reactive protein, found on further testing to be due to inflammatory bowel disease. Here investigations helped clarify whether it was dementia or comorbid pathology causing physical deterioration. Sometimes investigations are of uncertain relevance. An example is a patient presenting with late-onset psychosis and who was found to have a sodium of 125mmol/l due to the syndrome of inappropriate antidiuretic hormone secretion (SIADH; see below) and a raised thyroid stimulating hormone (TSH) level caused by not taking thyroxine for former radio-iodine treated thyrotoxicosis. Optimizing these abnormalities made no obvious difference to her mental state, which improved only after the introduction of an antipsychotic agent. This also illustrates that even when there is an apparently obvious physical cause for an observed mental state, it is often necessary to treat psychiatric comorbidity as well as optimizing the management of physical disorder.
The full blood count (FBC) and differential count help detect various conditions, including anaemia (low haemoglobin, low red cell count, micro/macrocytosis), infections (raised white cell count, neutrophilia), allergies or parasitic infections (eosinophilia), blood malignancies (raised cell count, abnormal cells in blood smear) and effects of drugs on particular cell lines (neutropenia or
Table 23.1 Reasons for conducting investigations in old age psychiatry
To rule out causative organic physical illness To aid in the diagnosis of some psychiatric conditions (e.g. dementia) To assess secondary physical effects of the presenting psychiatric disorder To help assess the impact of known medical co-morbidities To screen for common co-morbidities not obvious at presentation but likely to affect management To screen prior to the commencement of some medications and procedures To monitor drug levels in the blood To monitor potential side effects of prescribed drugs |
agranulocytosis with clozapine). The erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP) are non-specific tests that can point to infection, inflammation, anaemia, malignancy, temporal arteritis and autoimmune conditions. The ESR rises with advancing age and so becomes more difficult to interpret.
The incidence of psychiatric symptoms with B12 deficiency has been reported to vary between 4% and 50% depending on the population studied3. A correlation between serum cobalamin level and measures of cognitive function has been noted in some studies, although this has been disputed in those aged over 604. Deficiency of folate may be more likely to cause depressive symptoms and a low B12 has been linked to psychosis5. The true nature and reversibility of a B12 deficiency-induced dementia has been debated. In addition, deficiency of folate has been linked to poorer response to antidepressant treatment6. Confirmatory tests for the aetiology of vitamin B12 deficiency include gastric parietal cell antibodies, intrinsic factor antibodies and the Schilling test.
Routine biochemistry may detect electrolyte disturbances, dehydration and abnormal organ functioning (kidney, liver). The commonest psychiatric presentation of most of these is delirium. In addition, biochemical investigations are used to monitor the metabolic side effects of antidepressants or antipsychotics (e.g. SIADH and abnormal liver function tests [LFT]) and mood stabilizers (urea and electrolytes and thyroid function with lithium). SIADH is characterized by hyponatraemia (levels below 125mmol/l are usually symptomatic), low serum osmolality and inappropriately elevated urine osmolality. SIADH can develop early after initiation of drug therapy, especially with selective serotonin re-uptake inhibitors (SSRIs). Increasing age, female gender and medical co-morbidities are risk factors.
Transient asymptomatic rise in LFT is not uncommon during the first few weeks of prescribing psychotropic drugs. Gamma glutamyl transpeptidase (y GT) is elevated in liver disease, pancreatic disease, obesity and enzyme induction by drugs or alcohol, and 52% of alcohol dependent patients have been reported to have high yGT7. Due to its low specificity, y GT is not indicated as a screening test for alcohol misuse. More specific is the carbohydrate-deficient transferrin (CDT) enzyme immunoassay.
A random glucose above 11mmol/l suggests diabetes. Hypoglycaemia can cause delirium and can be seen in depressed diabetic patients who take their medication but neglect to eat.
Thyroid function testing (TFT) should be performed because of the well-known association of depression and hypothyroidism, easily overlooked in the elderly, and because ‘apathetic hyperthyroidism’ can be mistaken for depression. Patients on lithium should undergo TFT every six months. Raised corrected serum calcium can indicate malignancy (metastasis, multiple myeloma and lung cancer) and these patients may present with depressive symptoms. Iron studies including serum ferritin and total iron binding capacity are performed to help diagnose the type of anaemia (iron deficiency, sideroblastic or anaemia of chronic disease).
Because of the risk of the metabolic syndrome, fasting lipid screening is important in patients receiving antipsychotics. Waist measurement is a simple test of risk for this syndrome and there are international guidelines on waist measurement8.
Mid-stream urine (MSU) assessment is usually carried out to assess patients with confusion. In a sample of 68 patients Gregory et at? reported an overall percentage of significant results in 3.1% of their review of general psychiatry patients. Kolman9, though, studied older patients and found positive test results in 21% of patients. Noncontaminated samples are hard to obtain from patients with delirium or dementia.
The patient’s age correlates with the frequency of abnormal findings on chest X-ray10. A review of 746 psychiatric admissions11 identified that the 9% of patients who had a significant X-ray finding also had concomitant physical signs and symptoms. Chest radiology of all patients presenting with psychiatric symptoms is not warranted, and clinical suspicion remains the best yardstick. It should always be performed on patients at risk of conditions like tuberculosis (homeless persons, alcohol/drug misuse and patients with HIV infection) and (ex-) smokers with weight loss.
Chest radiography is usually performed routinely as a preanaesthetic screening tool prior to patients receiving ECT (some centres perform it on a mandatory basis on patients aged above 35).
Endoscopy and barium X-ray tests of the gastrointestinal system may be indicated for patients with weight loss and microcytic anaemia. These investigations are sometimes poorly tolerated by psychiatric patients so advances in CT imaging are important. Helical CT scanning of the abdomen with oral contrast, besides being rapid and non-invasive, can identify a range of pathologies of the gut and other structures.
Syphilis
The Venereal Disease Research Laboratory test, commonly known as the VDRL test, is a screening test for syphilis that measures antibodies to the spirochete Treponema pallidum in the blood or cerebrospinal fluid (CSF). The newer test analogous to this is the rapid plasma reagin (RPR). Treponema pallidum haemagglutination assay and the fluorescent Treponema antibody tests (TPHA/FTA ABS) are highly specific for Treponema antigens and are used at some centres as confirmatory tests, especially of CSF.
Clinically significant results were found in 0.3% (0-0.6%) of psychiatric patients routinely screened1. A retrospective study of all inpatients (mean age 74.5) undergoing syphilis screening in a UK hospital12 revealed that 16 of 423 tests were positive (3.8%). In four of the seven patients who received treatment, syphilis was identified as a likely contributor to the psychiatric presentation. The authors suggested that routine screening of elderly patients was justifiable where an organic aetiology was suspected, especially in dementia. Hilton13, though, highlighted the importance of considering local epidemiology, risk factors, neurological/neuropsychiatric features and ethics prior to the routine screening of patients. In the guidance on dementia issued by the National Institute for Health and Clinical Excellence (NICE), routine testing for syphilis is not recommended14.
Immunology
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree