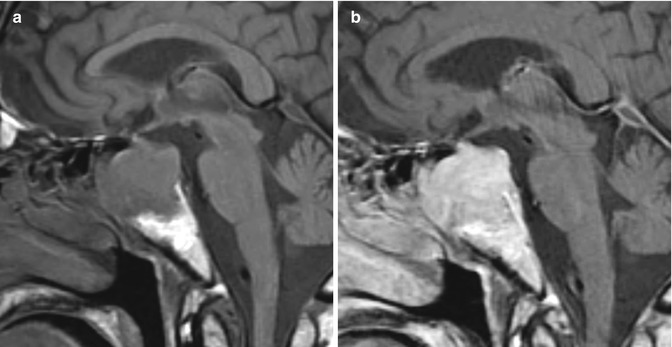
Fig. 22.1
Ipilimumab-induced hypophysitis. The patient has a history of metastatic melanoma treated with ipilimumab. Initial sagittal post-contrast T1 MRI (a) shows a normal pituitary gland and stalk. Sagittal and coronal pre- and post-contrast T1-weighted MR images (b–e) obtained 4 months later after implementation of ipilimumab show interval diffuse enlargement and homogeneous enhancement of the pituitary gland and stalk. Sagittal post-contrast MRI (f) obtained 4 months later after discontinuing ipilimumab shows interval decrease in size of the pituitary gland and stalk
22.4 Differential Diagnosis
Differential considerations for ipilimumab-induced hypophysitis include metastatic melanoma to the sella, other forms of hypophysitis, pituitary adenoma, craniopharyngioma, germinoma, and lymphoma. Certainly, clinical history and parameters will be helpful in formulating an appropriate differential diagnosis follow-up may be appropriate and decrease in size of the lesion will have indicated that ipilimumab was indeed the etiology.
Metastases: Overall, metastases to the sella are relatively rare, but can mimic ipilimumab-induced hypophysitis (Fig. 22.2). However, intrasellar metastases generally portend widespread systemic disease and are frequently synchronous with leptomeningeal and parenchymal brain metastases. Furthermore, unlike ipilimumab hypophysitis, melanoma metastases are frequently hyperintense on T1-weighted images, are heterogeneous due to intratumoral hemorrhage, and are parasellar (Fig. 22.3).
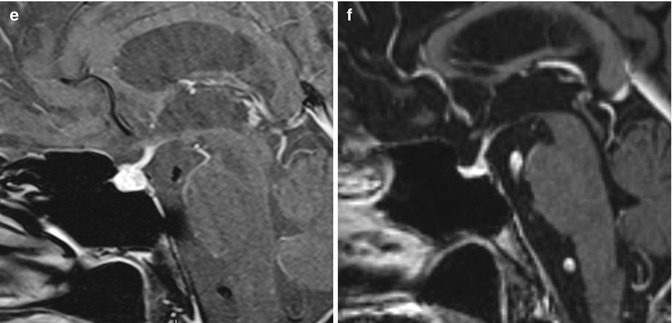
Fig. 22.2
Metastasis (lung cancer). Coronal post-contrast T1-weighted MRI shows a homogeneously enhancing mass within the sella
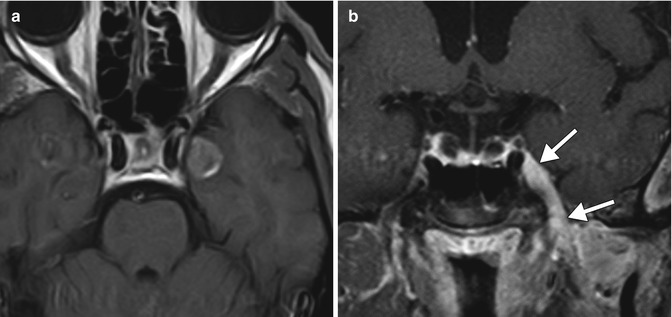
Fig. 22.3
Melanoma metastases in the parasellar region. Axial post-contrast T1-weighed MRI (a) shows a heterogeneously enhancing intraparenchymal melanoma metastasis within the left uncus. Coronal post-contrast T1-weighted MRI (b) in a different patient shows perineural extension of melanoma (arrows) along the left trigeminal nerve in the masticator space across the foramen ovale into Meckel’s cave and the cavernous sinus
Other causes of hypophysitis: Lymphocytic and granulomatous hypophysitis can both be considered forms of autoimmune hypophysitis that result from a variety of etiologies besides ipilimumab. For example, IgG4-related disease is a recently recognized systemic inflammatory condition that can manifest as hypophysitis (Fig. 22.4). Typically, autoimmune hypophysitis appears as low signal on T2-weighted images and enhances diffusely with variable degrees of pituitary and or infundibular enlargement. In addition, associated loss of the posterior pituitary bright spot is common and favors the diagnosis of autoimmune hypophysitis over pituitary microadenomas. Nevertheless, autoimmune hypophysitis can mimic nonsecreting pituitary adenomas on MRI. Indeed, approximately 40 % of patients with hypophysitis are misdiagnosed as having pituitary macroadenoma and undergo unnecessary surgery.
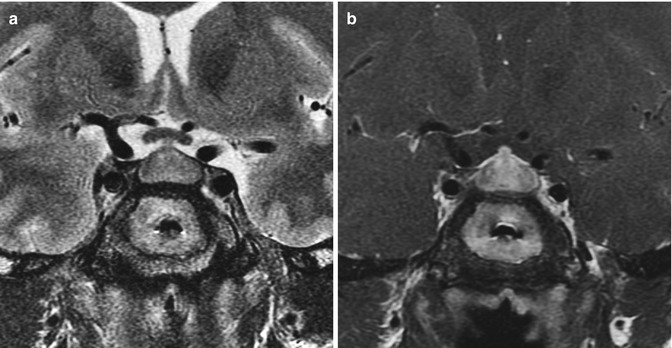
Fig. 22.4
IgG4-related hypophysitis. Coronal T2-weighted (a) and coronal T1-weighted (b) MR images show diffuse enlargement of the pituitary gland and infundibulum
Pituitary adenoma: Adenomas are the most common sellar mass and patients with melanoma treated with ipilimumab can certainly present with an underlying pituitary adenoma. Adenomas can have variable imaging appearances but generally demonstrate enhancement. In particular, microadenomas display delayed enhancement with respect to the normal pituitary gland and can be identified as a discreet mass. Enhancement tends to be more heterogeneous in macroadenomas compared with ipilimumab-induced hypophysitis. While macroadenomas can extend into the suprasellar cistern, the infundibulum itself usually does not enlarge as it does with hypophysitis. Macroadenomas can also occasionally be invasive, extending into the sphenoid sinus (Fig. 22.5). Interestingly, the presence of mucosal swelling in the sphenoid sinus favors the diagnosis of adenoma over autoimmune hypophysitis.