Key Points in Neuroanatomy
The examination of the nervous system depends on knowledge of the anatomy, which underlies the clinical findings. Following are some key points of neuroanatomy to help localize and diagnose neurologic disorders.
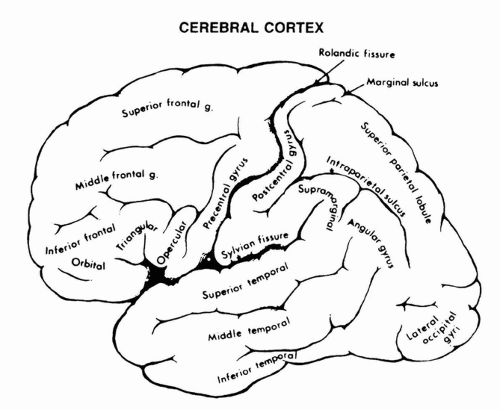
CEREBRAL CORTEX
The cerebral cortex comprises of four lobes for each hemisphere and each lobe has specialized functions (Fig. 34.1).
Frontal lobes participate in speech (the Broca area for speech is in the dominant hemisphere), movement (corticospinal tracts originate here), personality, and initiative. Frontal eye fields participate in conjugate eye deviation, so that lesions on one side cause the eye to deviate to the ipsilateral side. Signs of frontal disease: Broca aphasia (dominant), altered personality, utilization behavior (picks up and uses objects aimlessly), perseveration, altered judgment, apathy (abulia), apraxia, motor impersistence (give up on tasks, usually nondominant).
Temporal lobes participate in memory functions and auditory processing. For language, it is the dominant hemisphere; for music, it is usually the nondominant hemisphere. A unilateral temporal lesion may cause a contralateral superior quadrantanopsia as a result of involvement of optic radiations. Temporal lobe lesions may also cause memory loss; Kluver-Bucy syndrome (bilateral temporal lesions) of hyperorality, disinhibition of sexuality, hyperphagia; pure word deafness (can hear noises, but cannot understand speech, can read and speak normally), or Wernicke aphasia (dominant).
Parietal cortex participates in sensation, thus contralateral loss of cortical sensation occurs with lesions (two-point discrimination, identification of objects or numbers drawn in the hand). A mild hemiparesis may occur with parietal injury. Alexia, agraphia, left/right discrimination difficulty, and finger naming difficulty occur with a lesion in the left angular gyrus
of the parietal lobe (dominant hemisphere). Nondominant parietal lesions may cause visuospatial difficulty, dressing apraxia, a loss of awareness of the left side of the body, and topographic memory loss. Parietal lesions may also cause constructional apraxia (difficulty copying figures), ideomotor apraxia (inability to show motor acts such as throwing a ball, brushing their teeth), neglect (either of one side of body or one side of space). Nondominant parietal lesions may also cause an unawareness of a deficit on the opposite side of the body (anosognosia) and blunting of emotional responses or awareness of emotionality in others (aprosody).
Occipital lobes participate in vision. Lesions of the occipital lobe cause visual field loss, hallucinosis, or blindness. Altered recognition of objects or faces by sight also may occur. Patients with bilateral occipital lobe infarctions may be cortically blind (papillary reflexes are intact) but unaware of their blindness (Anton syndrome). Occipital lesions may also cause homonymous scotomas, visual hallucinations, palinopsia (image repeated more than once), prosopagnosia: difficulty naming faces, distortions of visual images, loss of color vision, or alexia
without agraphia (dominant lesion occipital lobe and posterior corpus callosum).
CIRCLE OF WILLIS
The anterior, middle, and posterior cerebral arteries supply the anteromesial cortex; the lateral frontal, temporal, and parietal lobes; and the occipital lobes, respectively. The internal carotid, and anterior and middle cerebral arteries are referred to as the
anterior circulation. The basilar artery supplies the upper brainstem, and the vertebral arteries supply the lower brainstem and cerebellum. These together are referred to as the posterior circulation. The anastomotic circle of Willis connects the anterior and posterior circulation through the posterior communicating arteries and the left and right circulations through the anterior communicating artery. The circle of Willis is frequently anatomically incomplete (Fig. 34.2).
anterior circulation. The basilar artery supplies the upper brainstem, and the vertebral arteries supply the lower brainstem and cerebellum. These together are referred to as the posterior circulation. The anastomotic circle of Willis connects the anterior and posterior circulation through the posterior communicating arteries and the left and right circulations through the anterior communicating artery. The circle of Willis is frequently anatomically incomplete (Fig. 34.2).
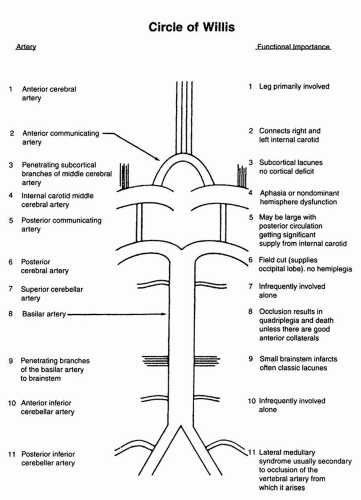 FIGURE 34.2. Cerebral circulation. |
EYE MOVEMENTS IN NEUROLOGIC DISEASE
The frontal eye fields exert a major influence on horizontal eye movement, each field being concerned with contralateral eye deviation. Thus, the right field causes eyes to move to the left. (The fibers cross in the pons and connect there to the extraocular muscles via the medial longitudinal fasciculus.) Both fields are constantly active, striking a balance; thus, when one is more or less active than the other, horizontal eye deviation results (Fig. 34.3).
A destructive lesion in the hemisphere or subcortex causes eyes to deviate toward the same side as the lesion. Thus, with a right-sided lesion, the eyes are deviated to the right. An excitatory lesion at the cortical level (e.g., a seizure) causes eyes to deviate to the contralateral side. A destructive lesion in the pons causes eyes to deviate to the side opposite the damage. Thus, with a left-sided lesion, eyes deviate to the right. Eye deviation secondary to hemisphere lesions, but not brainstem lesions, may be overcome by brainstem reflexes (e.g., doll’s eye maneuver).
Horizontal eye movements are served by the medial (third nerve) and lateral (sixth nerve) rectus muscles (Fig. 34.4). Inputs from the cortex and eighth nerve nuclei affect the paramedian pontine reticular formation, which drives the sixth nerve nucleus. This stimulates the ipsilateral lateral rectus and contralateral medial rectus, connecting with the latter through the medial longitudinal fasciculus. A lesion in the sixth nerve nucleus causes a paralysis of ipsilateral gaze (cannot bring the eyes to the side injured because of weakness in the ipsilateral lateral rectus and contralateral medial rectus).
Vertical eye movements are organized in the midbrain in a variety of nuclei. Thus disorders of up- and down-gaze suggest a midbrain lesion, and altered horizontal gaze suggests a pontine lesion. Convergence is also located in the midbrain and patients with midbrain lesions may have a combination of altered vertical gaze and loss of convergence.
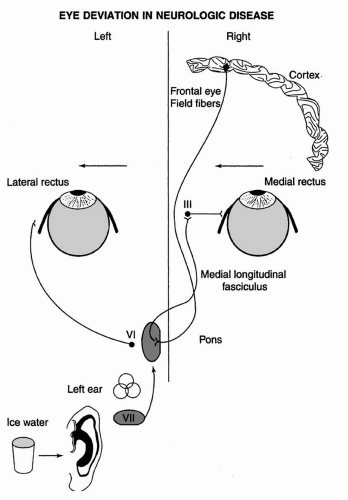 FIGURE 34.3. In the comatose patient with an intact brainstem, ice water in the left ear causes deviation of the eyes to the left. |
Various Eye Signs and What They May Indicate
There are a number of eye signs in neurology and each of them may suggest certain localizations or pathologies. For this reason it’s worth knowing the specific syndromes and what they may suggest.
Periodic alternating nystagmus: In the primary position (straight ahead) eyes beat to one side for a few seconds to a minute, slow
and stop beating, then begin to beat to the opposite side. This alternates every 2 minutes with a regular cycle. Indicates lesion of the flocculonodular lobe of the cerebellum, which may respond to lioresal.
Upbeating nystagmus: Jerk nystagmus evoked by upgaze. Seen in a variety of brainstem and cerebellar lesions, so localizes to the posterior fossa.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree