Chapter 18 Kyphoplasty
Indications
Kyphoplasty is performed in patients with recent vertebral fractures due to osteoporosis, angiomas, myelomas, metastasis, and so on, who present with pain refractory to conservative treatment including bed rest and drug treatment. The best results are obtained when the vertebral collapse has occurred recently—that is 3 months or less before the patient’s presentation [1,2].
Contraindications
Contraindications to kyphoplasty may be absolute or relative [1–3]. Absolute contraindications are as follows:
 Unstable fractures or neoplasms with involvement of the posterior vertebral wall (i.e., complex fractures with or without retropulsed fragments) and accompanying spinal canal compromise
Unstable fractures or neoplasms with involvement of the posterior vertebral wall (i.e., complex fractures with or without retropulsed fragments) and accompanying spinal canal compromiseRelative contraindications to the procedure are as follows:
Complications
There is an overall incidence rate of complications with this procedure ranges from 0 to 9.8% [4–9]. The most common is cement extravasation, which may be avoided with the following precautions [10]:
 Filling the void with thick, toothpaste-like cement using a low-pressure injection yields less cement leakage than filling the interstices of a fractured vertebra with thin, less viscous cement via a high-pressure injection, as is done in vertebroplasty.
Filling the void with thick, toothpaste-like cement using a low-pressure injection yields less cement leakage than filling the interstices of a fractured vertebra with thin, less viscous cement via a high-pressure injection, as is done in vertebroplasty. Adequate imaging with high-quality digital fluoroscopy, adequate cement opacification with sterile barium, and injection of cement which is not too liquefied can avoid leakage.
Adequate imaging with high-quality digital fluoroscopy, adequate cement opacification with sterile barium, and injection of cement which is not too liquefied can avoid leakage.Other, extremely rare complications of kyphoplasty are as follows:
Preoperative preparation
The imaging diagnosis would include the following:
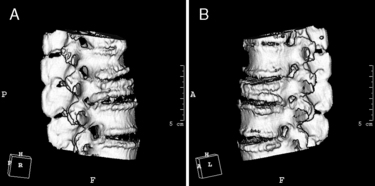
 Computed tomography (CT) scan with or without three-dimensional imaging to assess details of the bony architecture in cases of suspicion of a posterior cortical fracture (Fig. 18-1)
Computed tomography (CT) scan with or without three-dimensional imaging to assess details of the bony architecture in cases of suspicion of a posterior cortical fracture (Fig. 18-1) Magnetic resonance imaging (MRI) to detect signal change caused by bone edema at the level of a recent fracture (Fig. 18-2)
Magnetic resonance imaging (MRI) to detect signal change caused by bone edema at the level of a recent fracture (Fig. 18-2)Radiologic anatomy for kyphoplasty
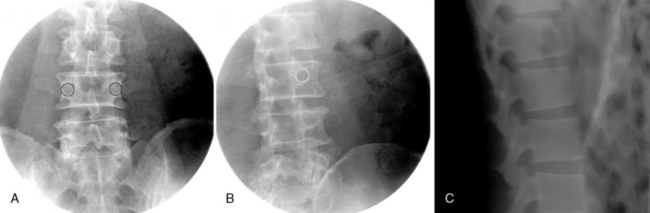
Radiologic landmarks for kyphoplasty should be identified as follows (Fig. 18-3)
Methods of kyphoplasty
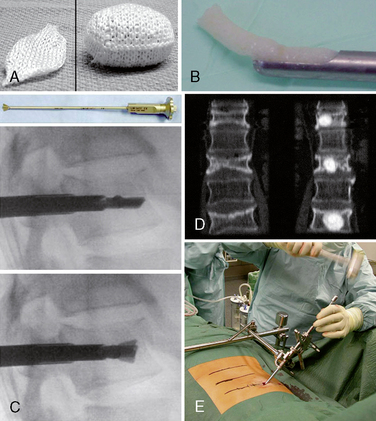
 Bone graft kyphoplasty: OptiMesh Deployable Grafting System (Spineology, Inc., St. Paul, MN) (Fig. 18-4)
Bone graft kyphoplasty: OptiMesh Deployable Grafting System (Spineology, Inc., St. Paul, MN) (Fig. 18-4)Instrumentation
Operating Room Setup
Figure 18-5 depicts the operating room setup for balloon kyphoplasty, consisting of the following:
Kyphoplasty Kit
Figure 18-6 illustrates the components of the balloon kyphoplasty system manufactured by Medtronic, Sunnyvale, CA, use of which is described in the procedure section of this chapter:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree