(1)
Department of Otorhinolaryngology Head and Neck Surgery, Asklepios Clinic Harburg, Eissendorfer Pferdeweg 52, 21075 Hamburg, Germany
Abstract
Laryngeal obstructive sleep apnea (OSA) is a rare condition. It occurs in adults and children. Laryngeal OSA has to be diagnosed endoscopically during sleep or sedation. In children, laryngeal OSA is caused by malformations, tumors, and laryngomalcia; the latter especially in preterm infants. In adults, laryngeal OSA mainly occurs in elder men due to a floppy epiglottis. More rare conditions are laryngeal and hypopharyngeal tumors and other disorders in this anatomical region. In children, laser surgery may help to provide tracheostomy. Various techniques have been described as being effective. In adults, treatment depends on the underlying illness.
Core Features
Laryngeal obstructive sleep apnea (OSA) is a rare condition. It occurs in adults and children. Laryngeal OSA has to be diagnosed endoscopically during sleep or sedation.
In children, laryngeal OSA is caused by malformations, tumors, and laryngomalcia; the latter especially in preterm infants.
In adults, laryngeal OSA mainly occurs in elder men due to a floppy epiglottis. More rare conditions are laryngeal and hypopharyngeal tumors and other disorders in this anatomical region.
In children, laser surgery may help to provide tracheostomy. Various techniques have been described as being effective.
In adults, treatment depends on the underlying illness.
The most frequent sites of obstruction are situated behind the soft palate and/or behind the tongue. Nevertheless, the larynx may contribute to the genesis of obstructive sleep apnea (OSA): As early as in 1981 Olsen et al. [522] described a case of OSA caused by a laryngeal cyst. Removal of the cyst yielded the disappearance of apneas. Since then, several case reports and small case series have been published, but it is still not possible to determine the concrete incidence of laryngeal OSA. Basically, there are two forms of laryngeal OSA: the pediatric and the adult form. In the following discussion, they will be considered separately.
9.1 Pediatric Laryngeal OSA
During childhood, malformations, complex malformation syndromes, tumors, or laryngomalacia may be considered as possible causes of a laryngeal OSA. In the case of newborns a further aspect can make matters worse: the immaturity of the respiratory control is often responsible for repetitive apneas and periodic breathing in early postnatal life. Consequences of this unstable breathing on blood gases and heart rate can lead to severe cerebral hypoxia and be life threatening, especially in preterm infants [160, 681, 702].
Malformations that lead to a laryngeal OSA have been documented in various case studies. Ruff et al. [632] describe the case of a previously healthy 13-year-old boy who developed OSA and bilateral vocal cord dysfunction secondary to type I Chiari malformation. He subsequently underwent a tracheostomy, a posterior fossa craniectomy, and C1-laminectomy. Four months after surgery he returned to school but still continued to require his tracheostomy. Two other case reports [59, 599] document that a congenital aplasia of the epiglottis may result in laryngeal OSA. Both children developed daytime sleepiness as a result of their OSA. One child underwent tracheostomy after she had developed heart failure. She was decannulated at the age of 7. Recently Chan et al. [100] presented an unusual case of a child with adenoid hypertrophy and occult supraglottic lymphatic malformation that manifested as laryngeal OSA.
Up to now, an epiglottic cyst [509], neurofibromas [673], and laryngeal papillomatosis [324] have been described as causes of OSA during childhood. We ourselves have recently treated a childhood OSA resulting from a hemangioma of the larynx of a 4-year old. The therapy consists in a resection or treatment of the tumors. Depending on tumor entity, size, and location, a temporary or permanent tracheotomy may become inevitable.
Laryngomalacia, or congenital laryngeal stridor, is a relatively benign, self-limiting condition first described in 1843 [40]. It seems to be the most common laryngeal congenital anomaly of all [290, 843]. It plays a significant role in the pathogenesis of laryngeal OSA in the case of the newborn, and especially for the preterm infant. In order to diagnose this dysfunction a fiberoptic laryngoscopy is essential. McSwiney et al. [457] described three anatomic abnormalities that cause laryngomalacia: (1) the epiglottis may be long and curled upon itself (the so-called omega-shaped epiglottis), and it prolapses posteriorly on inspiration; (2) the aryepiglottic folds may be short; and (3) the arytenoids may be more bulky than normal and prolapse forward on inspiration. Additionally, a mild subglottic edema may be present [843].
In mild cases, attentive observation is still the method of choice. Improvement always occurs before 12-18 months of age, and the outcome of these patients is invariably good [457]. In more severe cases, either a tracheotomy or laryngeal surgery may become necessary.
9.1.1 Surgical Techniques
Three principle types of surgery for laryngeal OSA can be distinguished. These are employed depending on the individual anatomic situation of each child.
The technique first to be described consists in a partial resection of the epiglottis. Zalzal et al. [843] first described a case series of 10 patients who underwent epiglottoplasty. This procedure addresses both the epiglottis and the mucosa of the aryepiglottic folds and the arytenoids. The epiglottis is grasped with cup forceps, and scissors are then used to trim the lateral edges of the epiglottis and the aryepiglottis folds. The mucosa of the arytenoids and corniculate cartilages is trimmed in a similar fashion. The author described the bleeding as minimal. Perioperative antibiotics are recommended.
Golz et al. [237] perform partial laser epiglottidectomy both in infants and adults if the epiglottis is found to be unusually long and flaccid. This technique solely addresses the epiglottis. As we, the authors use a Kleinsasser laryngoscope, a Riecker-Kleinsasser chest support, and the CO2-Laser (continuous wave or superpulsed mode, 6-10 W). The extent of the resection was individualized for each patient in this series according to the anatomic abnormality causing the obstruction. The authors perform a U-shaped excision leaving the lateral sides of the aryepiglottic folds intact. Bourolias et al. [64] recently described their technique of reshaping the epiglottis with the CO2 laser.
The second principle technique is called supraglottoplasty. Its characteristic consists in the resection of supraglottal mucosa. Senders and Navarrete [657] differentiate between four types of laser-assisted supraglottoplasty depending on the individual laryngeal finding (Figs. 9.1–9.4). The authors use the CO2 laser adapted to a microscope micromanipulator (100-200 ms pulse sequences; 5-8 W). The authors excise either the supra-arytenoidal mucosa (arytenoidoplasty, Fig. 9.1), the mucosa of the aryepiglottic folds (aryepiglottoplasty; Fig. 9.2), the posterior edges of the epiglottis (epiglottoplasty; Fig. 9.3), or the lingual mucosal surface of the epiglottis (epiglottopexy; Fig. 9.4). Depending on the anatomical situation, every combination of the four techniques can be performed.
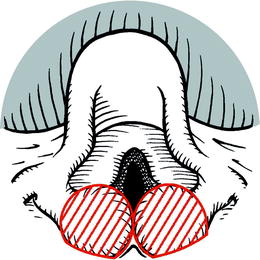
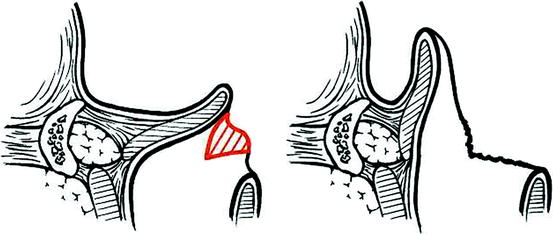
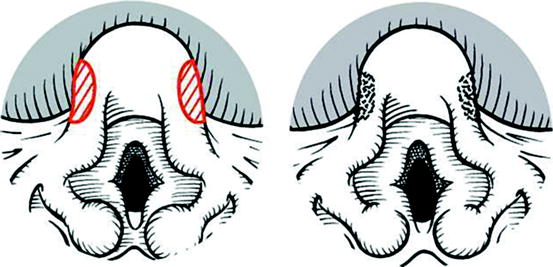
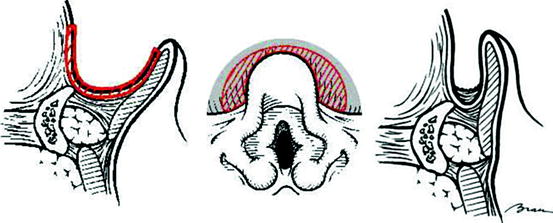
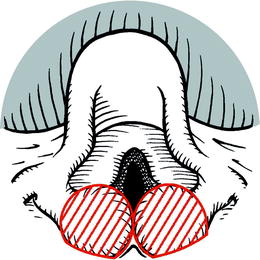
Fig. 9.1
Arytenoidoplasty according to Senders and Navarrete [657]. Coagulation of redundant mucosa of the arytenoids with a defocused laser beam
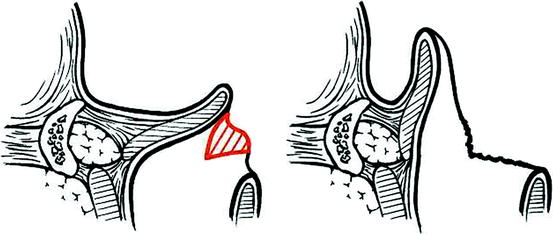
Fig. 9.2
Aryepiglottoplasty according to Senders and Navarrete [657]. Opening of a too short aryepiglottic fold
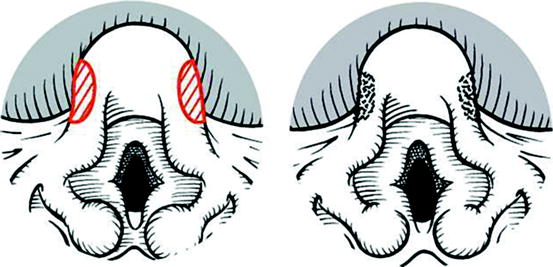
Fig. 9.3
Epiglottoplasty according to Senders and Navarrete [657]. Reduction of the too big epiglottis
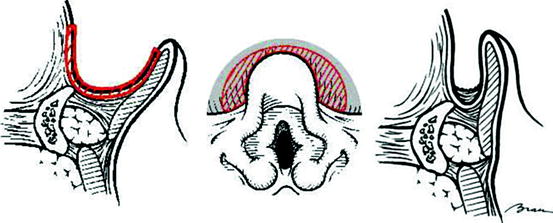
Fig. 9.4
Epiglottopexy according to Senders and Navarrete [657]. Scarring approximates the epiglottis to the base of tongue
The amount of redundant mucosa that should be resected is most suitably identified using the “suction test” [571]. Instead of the CO2 laser, laryngeal microinstruments can be used as well. We prefer the CO2 laser because of its additional hemostatic effect. For relatively minor cases we have found it advantageous to punctually vaporize the mucosa with a defocused laser beam, instead of excising it.
A third technique deals with the problem of the shortened aryepiglottal fold. Here the problem is not the redundant mucosa, which prolapses into the glottis during inspiration, but rather a too short distance between arytenoid and epiglottis root. We and other study groups [424, 656] treat these cases with a V-formed, 3-4 mm deep incision into both of the aryepiglottal folds. Already, intraoperatively the laryngeal entrance in the anterio-posterior dimenstion becomes visibly wider. For this procedure, we also prefer the CO2-laser (continuous wave or superpulsed mode; 6-8 W).
In principle, according to the individual anatomical situation, combinations of the three basic techniques are also possible. Toynton et al. [747] combined an incision of the arytenoid fold with a removal of redundant supraglottal mucosa.
9.1.2 Efficiency for SDB
Unfortunately, up to now no studies exist which present clean sleep lab data before and after larynx surgery. On the other hand, there are many therapy studies which use as primary variables the daytime symptoms of laryngomalacia. The following Table 9.1 summarizes the results of several recent studies.
It is difficult to compare the studies in Table 9.1 since they deal with different techniques, employ different success criteria, and in part treat very different kinds of patients. From a few of the studies [148, 657] it can be deduced that patients who have not been successfully treated with larynx surgery, are those who display significantly more frequently complex or additional malformations.
Table 9.1
Effectiveness of surgery for severe laryngomalacia in children
Author | N | Procedure | Follow-up | Success rate (%) | Definition of success | EBM |
|---|---|---|---|---|---|---|
Golz et al. [237] | 12 | Partial laser epigottidectomy | 14-52 months | 100 | Subsiding of stridor | 4 |
Senders and Navarrete [657] | 23 | Laser supraglottoplasty | No data | 78 | Immediate relief of symptoms avoidance of tracheotomy | 4 |
82.6 | ||||||
Toynton et al. [747] | 91 | Aryepiglottoplasty | 1 month | 54.9 94.5 | Relief of stridor improvement of stridor | 4 |
Reddy and Matt [593] | 106 | Supraglottoplasty | No data | 95.7 | Relief of symptoms | 4 |
Denoyelle et al. [148] | 136 | Laser supraglottoplasty | 3 days to 60 months | 79 | Relief of symptoms | 4 |
Zafereo et al. [842] | 10 | Laser supraglottoplasty | 2-29 weeks | 100 | Successful extubation | 4 |
90 | Significant improvement | |||||
20 | Complete resolution | |||||
All | 378 | 55-100 | C |
Due to the fact that these are solely retrospective studies, it needs to be mentioned that an evidence proof according to Cochrane criteria has as yet not been established. Nevertheless, we do feel justified to infer a tendency to the effect that for a high percentage rate children with a severe laryngomalacia can be spared a tracheotomy with the help of an individually adapted larynx procedure.
9.1.3 Postoperative Care and Complications
Despite the high success rate, in 11.6% of the cases an initial deterioration of the stridor and in 4.7% the necessity of a reintubation or tracheotomy (1.2%) must be anticipated. These risks further increase in those cases which do not present an isolated laryngomalacia but complex malformations [657]. In any case, we regard an observation of the children in an accordingly furnished intensive care unit during the first postoperative night as necessary. In cases where the parents or other supervising persons are present, a monitoring of the respiration may be sufficient. In any case, this procedure should be performed on an inpatient basis.
Most authors [148, 657] routinely use corticoid therapy (beclomethasone, 125 μg/kg) within the first 3-5 days postoperatively, as we do in our center. In contrast to other recommendations we do not routinely use anti-inflammatory drugs or antibiotics.
Overall, the complication rate of the described surgical procedures is quite low, and does not vary significantly between the various techniques. The overall complication rate is given as between 5.8 [747] and 7.4% [148]. There is no difference concerning the complication rate in patients with isolated laryngomalacia compared to those having additional congenital anomalies [148].
As minor complications, aspiration of early feeds (7.0%), granulomas (1.5%) that had to be removed under general anesthesia, significant edema (1.5%), minor intra-operative hemorrhage (1.2%), and a posterior fibrous web between the arytenoids (0.7%) which required division with microscissors or laser, have been described.
9.1.4 Indications and Contraindications
The diagnosis of the laryngeal OSA is performed with the help of an endoscopic examination. In the case of tumors and complex malformations the therapy depends on the primary disease. Laryngomalacia is a disease of the perinatal phase, and is especially salient in the case of preterm infants. In minor cases, waiting is the therapy of choice. A close cooperation with the child’s pediatrician is necessary.
In severe cases, an endoscopy needs to be employed in order to determine whether a shortening of the epiglottis, a removal of redundant supraglottal mucosa, an incision of the aryepiglottal fold, or a combination of the three procedures is indicated. In the case of a correct indication, in over 80% of the cases the children can be spared a tracheotomy or a decannulation becomes possible. We do not consider a minimum age restriction to be in effect for these procedures.
The alternative to a surgical procedure consists in a noninvasive respiration therapy [190].
9.2 Adult Laryngeal OSA
In contrast to children, laryngomalacia plays only a minor role in adults. The only exception to this is the so-called floppy epiglottis. The floppy epiglottis is a relatively rare anatomic finding in adults. Nevertheless, Catalfumo et al. [94] found this condition in 12 of 104 patients who failed a UPPP procedure. We relatively frequently observe a floppy epiglottis in older male patients [773]. One explanation for this may be the fact that apart from the pinna of the ear the epiglottis is the only organ of the head and neck consisting exclusively of elastic cartilage. Pellnitz [553] has shown a significant increase in the length, breadth, and weight of the epiglottis in males, while females show reductions for the same parameters. Histological study of 500 epiglottal specimens obtained at autopsy shows that size increases in the male epiglottis is due to secondary intercellular deposits of byproducts of the metabolism. There were sex-specific differences in the perichondrium. Pellnitz postulated specific hormonal influences in connection with these findings, since the growth of the larynx is considered a secondary sexual characteristic. Nevertheless, a floppy epiglottis has also been described in younger men and, rarely, in women [22, 820].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






