Chapter 51 Lateral Extracavitary Approach to the Thoracolumbar Spine
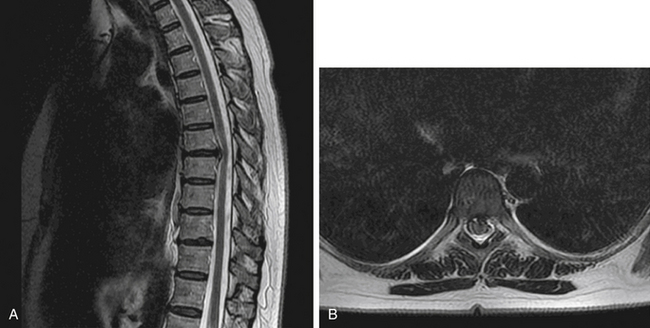
The lateral extracavitary approach (LECA) can be used in the thoracolumbar spine to access both the ventral and dorsal elements of the spinal column. Through this approach, discectomy, spondylectomy, fusion, and deformity reduction may be accomplished. In addition, other approaches, including transpedicular decompression and laminectomy, can be added to allow a 360-degree approach through one incision. LECA was first used as a derivation of lateral costotransversectomy in the treatment of tuberculous spondylitis (Pott disease) by Capener in 1933 and first reported by Seldon in 1935.1 It was also described in 1960 by Hulme, who advocated it as an alternative to laminectomy for ventral thoracic pathology, including disc herniation, secondary to the high incidence of poor surgical outcome of laminectomy attributed to inadequate exposure of ventral elements and the requirement of direct manipulation of the thoracic spinal cord and its extradural vasculature.2 The approach was further refined by Larson et al. at the Medical College of Wisconsin, and it has been applied to traumatic lesions, thoracic disc herniations, tumors, and other pathologic conditions1,3–7 (Figs. 51-1 to 51-5). This approach has recently been modified in a cadaver study to be used via minimally invasive retractor systems for deformity correction.8 Minimally invasive LECA has also been used successfully in thoracic disc herniation.9
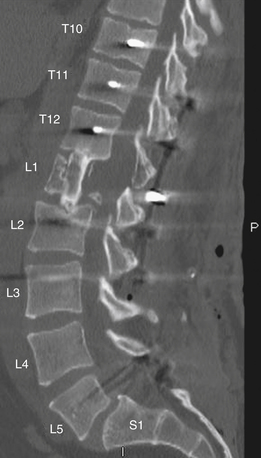
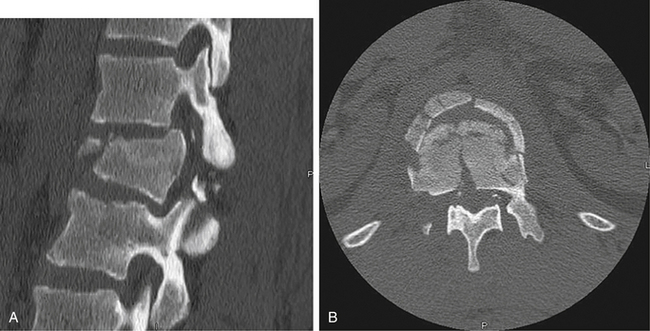
FIGURE 51-4 Postoperative sagittal CT reconstruction of the patient in Figures 51-2 and 51-3. The patient underwent a lateral extracavitary partial corpectomy of L1 with allograft and posterior instrumentation.

FIGURE 51-5 Anteroposterior radiograph demonstrating T10-L3 instrumentation in the patient from Figures 51-2 to 51-4.
This approach can be applied to ventral spinal lesions located between T1 and L5 and, if necessary, can be performed in a bilateral fashion for more extensive pathology.10 In addition to decompression and the removal of pathology, ventrolateral instrumentation can be accomplished through LECA with additional instrumentation placed dorsally as needed.
Operative Technique
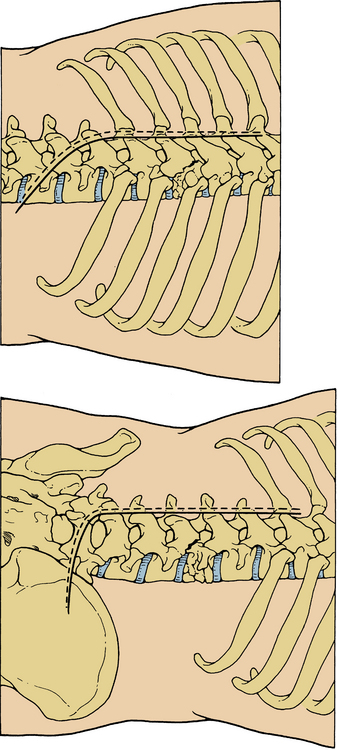
Following the induction of general anesthesia, the patient should have a Foley catheter placed and appropriate preoperative antibiotics administered. The Jackson table provides optimal padding and available positioning for LECA, and all pressure points should be checked after positioning. The patient should be safely secured to the table at all points because the bed will be rotated later in the case. For discectomy or fractures, the use of intraoperative monitoring is not essential; for deformity correction and tumor cases, such monitoring may provide an additional measure of safety. Following induction and proper positioning, the next step is appropriate fluoroscopic localization of the lesion. This is critical because the exposure provides a direct view of specific vertebrae, and extending the exposure more than one level in either direction can be difficult. It is imperative to have a clear understanding of the bony anatomy on radiograph before surgery to aid in localization. The typical anatomy of the rib and thoracic spine interface is also an important fact to keep in mind. In most patients a rib abuts disc space in the thoracic spine, and this rib typically corresponds to the caudal vertebrae at the segment.11 For example, at T7, the rib typically articulates with the T6-7 disc space. This anatomy holds true down to the T10-11 space. The 11th and 12th ribs typically articulate with the corresponding vertebral bodies below the disc spaces. It is generally advisable to count ribs in the thoracic spine from above and below and to compare this count with preoperative radiographs for confirmation.
Once the location has been confirmed and marked, attention is given to planning the incision. Various shapes have been used (Fig. 51-6), but the hockey stick–type incision is generally performed. The incision should generally extend from at least one segment cranial to the pathology to one segment caudal to it, with the caudal limb angling out toward the pathologic side with attention paid to the need for approaching the dorsal elements or placing instrumentation. For procedures involving dorsal fixation and fusion, the straight midline portion of the planned incision should extend to the segments to be included in the construct. In the case of single-level discectomy without a need for dorsal exposure, a paramedian incision may be used and may be as small as 5 cm in length.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree