61 Lateral XLIF Fusion Techniques
Introduction
Demands of mobility and quality of life have increased in the elderly segment of society over the past decades. A rising number of elderly patients suffering from adult degenerative scoliosis may be eligible for surgical treatment.1 The prevalence of adult scoliosis rises with age: from 4% before age 45 years, to 6% at age 59 years, to 15% in patients older than 60 years.2
Adult scoliosis is defined as acquired deformity in the skeletally mature patient with a Cobb angle of at least 10 degrees in the coronal plane due to asymmetric disc and facet joint degeneration. It is associated not only with severe back and/or leg pain but also with complicated surgical outcomes.9
All nonoperative treatments should be exhausted before considering surgical treatment. Usually, the surgical procedure is focused on two aims. The first aim is to decompress the comprised neural elements in cases of symptomatic spinal stenosis, and the second is to balance and stabilize the spine in the coronal and sagittal planes when there is imbalance.4 Today a wide variety of approaches—anterior, posterior, or a combination—are available to achieve fusion, but all include significant operative morbidity.5 Newer implants have improved cosmesis and correction, obtaining better results; however, the elderly patient is not a candidate for this kind of surgery because of the higher risk of complications and generally poorer bone quality in this population.6
The eXtreme Lateral Interbody Fusion (XLIF) approach may offer various clinical advantages over more traditional techniques for treating adult degenerative scoliosis.7 This less invasive procedure realigns the endplates to a horizontal position through bilateral annular release, placement of a large implant across the disc space spanning the ring apophysis, and the effects of ligamentotaxis. The XLIF technique restores disc and foraminal heights, indirectly decompressing the neural elements, and promotes stabilization through an anterior intervertebral fusion stopping progression of the curve.
Clinical Study
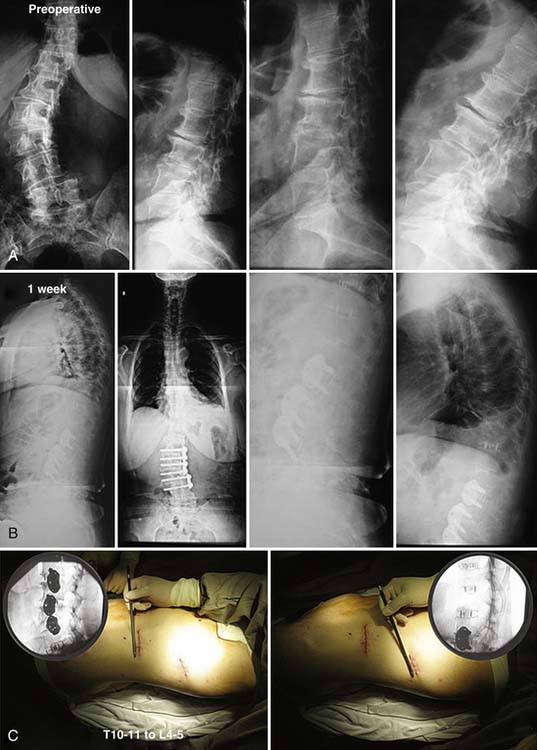
In a larger patient series, 23 patients have 3-year follow-up (FU). Mean age is 66 years (range, 39 to 88). Three to seven levels were treated between T10 to L5. Three of these needed lateral plate fixation (Figure 61-1).
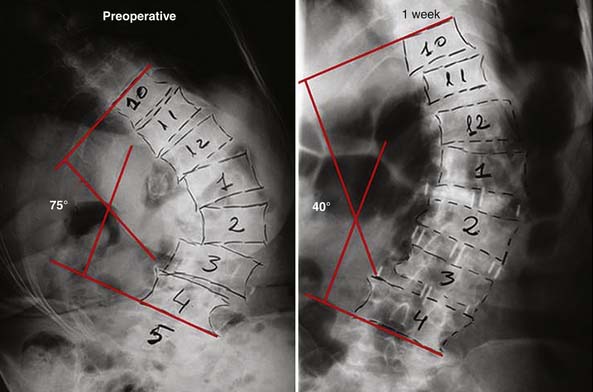
The procedures were performed without major complication in an average of 121 minutes and with <50 ml blood loss. Mean hospital stay was 40 hours. After 3-year FU, one patient (4%) presented with pseudarthrosis according to Food and Drug Administration (FDA) fusion criteria.7 Three patients (12%) had subsidence at 6-month FU, but all were asymptomatic. Visual Analogue Scale (VAS) pain scores improved from an average of 8.1 preoperatively to 3.3 at 3-year FU.Oswestry scores improved from an average 47.8 preoperatively to 22.8 at 3-year FU. Coronal and sagittal alignments improved from average Cobb angles of 16 degrees preoperatively to 7.4 degrees at 3-year FU, and average lordosis angles of 37.8 degrees preoperatively to 48 degrees at 3-year FU. The mean preoperative Cobb angle was not high because in our earliest series we were not treating large curves. Currently, using the XLIF approach we can treat curves up to 90 degrees, with very good clinical results (Figure 61-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree