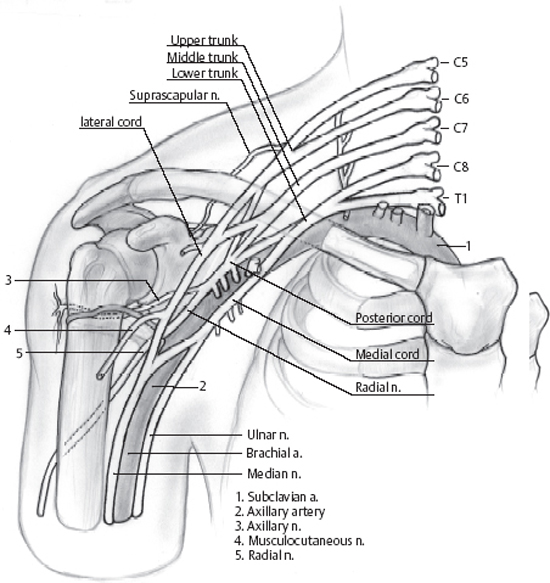
6 Medial Cord Injury A 32-year-old, right-handed man presented with a poorly defined history leading up to his neurological deficit. He had chronic lower back pain despite four operations. Immediately following the placement of an intrathecal morphine pump, he developed an allergic reaction with rhabdomyolysis involving the right arm and shoulder, acute renal failure, and right cerebellar and left frontal infarcts. He was in a coma for 2 days. When he awoke he noted that his whole right hand (particularly the ulnar three digits) felt like it was in boiling water, and he was unable to move the hand. The pain was refractory to medication and the neurological deficit remained unchanged for 5 months. Examination revealed trace or slightly better (grade 1–2) function in the right adductor pollicis (AddP), abductor digiti minimi, interossei, lumbricales, first dorsal interosseous, all flexor digitorum profundi (FDP), flexor digitorum superficialis (FDS), flexor pollicis longus, abductor pollicis brevis (APB), opponens pollicis, and flexor carpi ulnaris (FCU). He also had weakness of the lower portion of the pectoralis major. Strength was normal in the flexor carpi radialis (FCR) and pronator teres (PT). Upper limb motor function was otherwise normal. Sensation to pinprick was diminished in the ulnar three digits. Forearm and arm circumferences were symmetric. Reflexes were preserved in the upper limb. Percussion tenderness was present in the upper chest and radiated into the ulnar side of the hand. Electrodiagnostic studies demonstrated a right brachial plexopathy involving primarily the medial cord. The involvement of the pectoralis suggested a lesion of the medial cord at the junction of the lower trunk. There were absent sensory potentials in the right middle, ring, and little fingers, diminished in the thumb and index finger. The median motor response was absent and the ulnar motor response was diminished. F wave studies of the ulnar nerve were prolonged. Radial sensory response was normal. Needle electromyography showed complete denervation of the APB, a solitary unit in the AddP. Denervation was seen in the pronator quadratus, FCU, FDS, FDP, and pectoralis major. Normal potentials were seen in the PT and FCR. There was some regeneration in the pectoralis major, but none elsewhere. His neurological loss was primarily but not exclusively in the distribution of the medial cord. The mechanism of the injury was uncertain but perhaps was related to soft tissue swelling or the placement of a central line. Exploration of the brachial plexus with intraoperative nerve action potential (NAP) recordings was performed in the hopes of improving his function and pain. Supraclavicular dissection was performed to obtain control of the neural elements proximal to the zone of injury. Upper plexal elements were dissected initially. There was dense scar involving the lower trunk and lower trunk to medial cord. NAPs could be recorded in all elements. Over the first year, he regained grade 3 to 4 function of his hand intrinsics and extrinsics and the Tinel sign advanced ˜1 foot from the inferior aspect of the incision. At 5-year follow-up, he still complained of burning in the medial aspect of the hand (despite the use of antiepileptic medications) and occasionally still dropped objects. He had regained 4+ –5–/5 function in the affected hand intrinsic and extrinsic muscles and grade 4/5 sensation in the medial cord distribution. Predominant medial cord injury The medial cord is derived from the anterior division of the lower trunk. The divisions lie deep to the clavicle, whereas the cords lie in the infraclavicular region. The medial cord is medial to the axillary artery and lateral to the axillary vein (Fig. 6–1). The medial cord contribution to the median nerve typically passes superior to the axillary artery. The median nerve may be traced proximally to the medial cord, and the axillary artery can be identified safely in its typical pectoral network and the medial antebrachial and brachial nerves. These particular anatomical relationships may become distorted following trauma or previous surgery. The medial cord innervates all of the intrinsic muscles of the hand: the ulnar nerve and the hand (intrinsic) component of the median nerve. The lateral cord typically supplies the wrist/forearm motor component of the median nerve, but this may be variably supplied by the medial cord. The medial cord gives ulnar distribution sensation.
 Case Presentation
Case Presentation
 Diagnosis
Diagnosis
 Anatomy
Anatomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree



