♦ Preoperative
Operative Planning
- Review imaging
- Computed tomographic (CT) scans of the head
- Identifies location of subarachnoidal hemorrhage (SAH) within cisterns, evidence of calcification of the aneurysm wall, presence of hydrocephalus, and cerebral infarcts
- If multiple aneurysms present, can determine which aneurysm ruptured based on distribution of subarachnoid blood in cisterns; ruptured MCA aneurysms tend to cast the ipsilateral sylvian fissure
- Identifies intraparenchymal or subdural hematomas that can be addressed during surgery
- Identifies location of subarachnoidal hemorrhage (SAH) within cisterns, evidence of calcification of the aneurysm wall, presence of hydrocephalus, and cerebral infarcts
- CT angiogram (CTA) with three-dimensional reconstructions: may be used as sole vascular imaging modality for preoperative planning in high-volume centers where reconstructions may be rapidly accrued.
- Six-vessel catheter-based angiogram: conventional alternative to CTA
- Identifies number of aneurysms and their sites of origin, breadth and shape of aneurysmal neck, orientation of fundus, relationship to and anatomy of M2 branches, and potential need for bypass
- External carotid circulation should also be imaged to assess collateral circulation and potential conduits for extracranial-intracranial bypass
- Identifies number of aneurysms and their sites of origin, breadth and shape of aneurysmal neck, orientation of fundus, relationship to and anatomy of M2 branches, and potential need for bypass
- Brain relaxation: if MCA aneurysm is ruptured and patient has sufficiently good Hunt-Hess grade (so as not to require ventriculostomy drainage prior to surgery), consider placing in the operating room for purposes of cerebrospinal fluid (CSF) release and in anticipation of likelihood of its necessity in the postoperative period.
- Computed tomographic (CT) scans of the head
- Micro-Doppler probe to grossly check patency of native vessels after clipping
- We recommend intraoperative angiography in which case the radiolucent Mayfield head holder should be used
- Conventional microsurgical set with microscope
Anesthetic Issues
- General anesthesia with oral endotracheal intubation
- Subclavian venous catheter for central venous pressure monitoring for patients with ruptured aneurysms
- Arterial lines for continuous blood pressure monitoring
- Femoral arterial sheath for intraoperative angiography after clipping or bypass
- Scalp needle electrodes for electroencephalographic monitoring in cases of burst suppression
- To maintain cerebral perfusion, keep patient euvolemic and normotensive. Moderate hypotension can be used during the dissection of the aneurysm.
♦ Intraoperative
Positioning
- Patient supine with roll under ipsilateral shoulder and head fixed in threepin Mayfield head holder, elevated above the heart, rotated 45 degrees contralateral to the incision, and slightly extended with the malar eminence as the highest point (Fig. 24.1)
- Neck flexed slightly to the contralateral shoulder to flatten orbital roof and the vertex lowered slightly
- Make certain endotracheal tube and materials securing it do not obstruct venous outflow in the neck
Incision and Craniotomy
- Mark a standard frontotemporal/pterional incision made completely behind the hairline from 1 cm anterior to the tragus to behind the widow’s peak
- Shave, scrub, and prep frontotemporal area with alcohol and Betadine; inject local anesthetic (lidocaine)
- If bypass is required—as in cases of complex or giant aneurysms—map out the superficial temporal artery (STA) on the scalp using Doppler ultrasound and avoid infiltration of scalp with lidocaine with epinephrine; isolate the STA and its adventitia along its full length for later use
- Start incision no more than 1 cm anterior to the tragus of the ear at the root of the zygoma (prevents injury to frontalis branch of cranial nerve [CN] VII) and extend behind hairline up to the midline
- Prepare a Yasargil skin flap to direct galeal flap anteriorly and temporalis muscle inferiorly so as not to obstruct field of view. For distal MCA aneurysms this will not be required. Separately dissect skin, staying deep to fat pad in keyhole region to avoid frontalis branch of CN VII; reflect inferiorly over rolled sponge, careful not to damage nerves reflected with skin flap; secure with fishhook retractors.
- Incise temporalis muscle along the superior temporal line and posterior margin of the skin incision using monopolar cautery, leaving a superior tuft of muscle to allow reapproximation of the temporalis muscle and fascia upon completion of the procedure; reflect muscle flap inferiorly with skin flap exposing McCarty’s keyhole and frontal zygomatic process
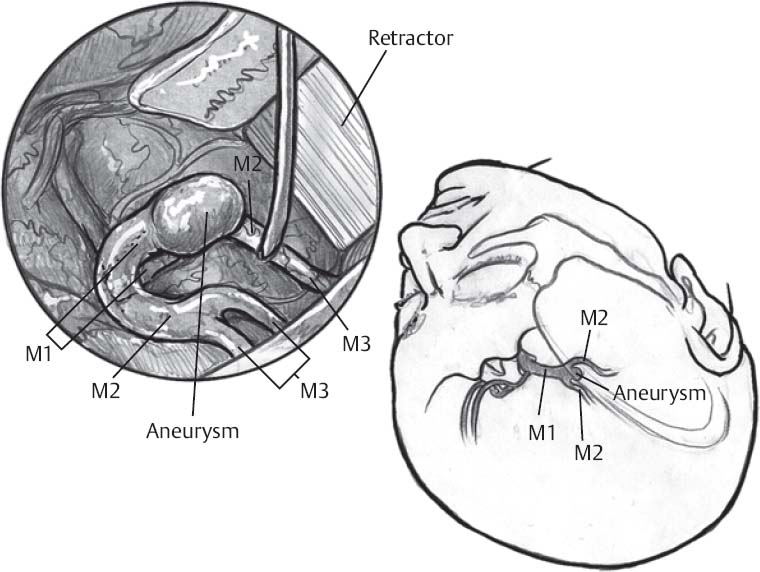
Fig. 24.1 Schematic of surgical treatment of middle cerebral artery aneurysm.
- Use craniotome to place burr holes in the keyhole region, the temporal squamous bone slightly above the root of the zygoma, and at the posterior margin of the incision at the height of the temporalis muscle
- Turn a standard pterional bone flap with the superior tuft of temporalis muscle included
- Remove temporal squamous bone with rongeurs and drill down the lateral roof of orbit and lesser wing of the sphenoid bone until the orbitomeningeal artery is visualized; allows better exposure of the proximal sylvian fissure and gentler retraction of the temporal lobe
- Place Surgicel and narrow Cottonoids around margins of the craniotomy and wax all bony margins
- Open dura in a crescent moon-shaped fashion centered over the sylvian fissure to minimize venous run-in; place dura on stretch with sutures and cover with moist patties
- Bring in operating microscope for use from here on
- Use craniotome to place burr holes in the keyhole region, the temporal squamous bone slightly above the root of the zygoma, and at the posterior margin of the incision at the height of the temporalis muscle
Surgical Approach
Transsylvian Approach
- We favor a wide splitting of the sylvian fissure with early CSF release and brain parenchyma softening, minimal brain dissection, removal of hematoma if present, wide exposure of the MCA bifurcation after proximal internal carotid artery (ICA) control
- Note: MCA aneurysms typically occur at the bifurcation and may adhere to the temporal lobe, so proceed gently with retraction so as not to avulse the dome
Procedure
- Dissect sylvian fissure (superficial exposure) 3 cm distal to the anterior lip of the inferior frontal surface of the fissure with an arachnoid knife; venous drainage typically runs parallel to the sylvian fissure and is associated with temporal surface. Small cortical veins within the sylvian fissure can be sacrificed without great concern if needed.
- Open arachnoid anteriorly from the point of entry using sharp and blunt dissection and identify an M3 segment of the MCA on the lateral aspect of the frontal and temporal lobes and follow it proximally with sharp dissection; the thin wisps of arachnoid can be cut sharply
- Open fissure with gentle retraction on both the frontal and temporal lobes (Fig. 24.1)
- Dissect along M2 segment to expose the lateral lenticulostriate vessels, limen insula, aneurysmal neck, and finally the M1 segment; arteries within the sylvian fissure either run frontally or temporally and can be reflected in their respective directions
- The ICA should be identified for good proximal control
Transtemporal Approach
- Advantages: smaller craniotomy, provides direct approach to essential anatomy, good visualization of the inferior M2 trunk, less brain retraction, and less manipulation of M1
- Disadvantages: minimal release of CSF, more tissue resection required, and often exposure of fundus before gaining proximal control. We almost never use this approach.
Procedure
- Can remove slightly less bone from the lateral orbital roof and lesser wing of the sphenoid bone
- Make 3 to 4 cm corticectomy in the superior temporal gyrus centered 2 cm posterior to the anteriormost aspect of the sylvian fissure
- Use a subpial resection of the superior temporal gyrus to enter the horizontal portion of sylvian fissure to allow visualization of M2 segments of MCA
- Dissect from distal to proximal within the sylvian fissure to identify the M1 segment, lenticulostriate vessels, and the aneurysm neck and fundus
Clip Application
Guidelines
- Apply clips parallel to parent vessels whenever possible
- Minimize torque on M1 and M2 segments to lower risk of vessel stenosis and ischemia
Saccular Narrow-necked Aneurysms
- Least common form found in this region
- Clip placement should ideally be parallel to M1 and M2 segments; on occasion clip may be placed perpendicular to the proximal and distal vessels
- Usually include either a portion of the M1 or M2 vessel wall in their necks
- Common anatomic variations in this region necessitate complete dissection of the neck and fundus of the aneurysm and surrounding vessels
Fusiform Aneurysms of the MCA Bifurcation
- Often requires bypass procedures to reconstitute flow in the distal M2 segments; use cerebral protection during the bypass
- If only one M2 branch involved in the fusiform aneurysm, use end-to-end anastomosis between the involved M2 segment and the normal M2 segment
- If all M2 segments are involved in the fusiform aneurysm, may need to use STA-MCA bypass; place proximal clip on STA, transect distal end to appropriate length, dissect adventitia away from distal end, irrigate vessel with heparinized saline, and anastomose to M2 branch with running 10–0 Prolene sutures (Ethicon; a suture placed at each pole of the anastomoses with one run along the frontal and one along the temporal surfaces)
- Rubber dam placed under the recipient vessels will allow visualization of the suture
- Intraoperative angiography used to evaluate bypass before closure of craniotomy
- Closely oppose the galea during closure to avoid leakage of CSF because dura cannot be closed tightly in this situation
Using Temporary Clips
Guidelines
- None of the clips should limit the surgeon’s view
- Proximal M1 clip should be placed first, followed by distal clips if needed
- Try to maximize flow within the lenticulostriate vessels
- Clips should not be placed in region of atheroma (could result in embolic complication)
- Distal temporary clips should be removed first before removing proximal temporary clip
Potential Uses
- Useful in cases of aneurysm rupture, or in large/complex unruptured aneurysms, facilitating complete dissection of the aneurysm, softening of aneurysmal neck to allow clip placement, and aneurysmorrhaphy
- Required if opening the aneurysm is needed to collapse its contents and allow proper clip closure
- Removal of large thrombus: remove with ultrasonic aspirator, micropituitaries, or sharp dissection
- Removal of calcified plaque: surgical removal or crush with hemostat
- Removal of large thrombus: remove with ultrasonic aspirator, micropituitaries, or sharp dissection
Reexamination and Closure
- Confirm patency of native vessel visually and with the use of an intraoperative micro-Doppler; readjust the clip(s) if necessary
- Can use intraoperative angiography is desired; in this case, remove brain retraction system, cover exposed brain with damp Cottonoids without radiopaque markers, and cover the surgical exposure with soaked lap sponge
- Once obliteration of aneurysm is confirmed, puncture fundus with 26-gauge spinal needle to rule out residual filling and remove any mass effect
- Leave papaverine soaked Gelfoam over manipulated arteries
- Maintain thorough hemostasis using bipolar cautery
- Apply abundant irrigation to wound and close dura with 4–0 Nurolon sutures
- Secure bone flap with microplates and screws
- Reapproximate the temporalis muscle and fascia, as well as the galea, with interrupted sutures
- Close skin with a nylon suture or staples
- Place a catheter and Jackson-Pratt drainage bulb during scalp closure for postoperative wound drainage; usually maintained for 24 hours
- Maintain thorough hemostasis using bipolar cautery
♦ Postoperative
- Continue perioperative antibiotics for 24 hours
- Closely monitor the patient’s serum electrolytes and cardiopulmonary status in the intensive care unit
- Subacute neurological deterioration (several hours postoperatively) not related to seizures, hemorrhage, or persistent brain edema may be due to M2 occlusion or stenosis from clip rotation following closure or swelling of sylvian fissure
- Urgent CT scan to rule out hemorrhagic complication
- Expeditious angiography to confirm vessel patency
- Immediate evacuation for any hematomas of significant size
- Urgent CT scan to rule out hemorrhagic complication
- Delayed hydrocephalus should be managed with ventricular drainage followed by placement of CSF shunt, if necessary
- Meticulous vasospasm watch in cases of aneurysmal rupture
< div class='tao-gold-member'>
Only gold members can continue reading. Log In or Register to continue








