♦ Preoperative
Special Equipment
- Basic tray
- Hand tray, which contains finer bipolar forceps and self retaining retractors than a basic tray
- Sterile, malleable hand holder to maintain hand position with some wrist extension
Operating Room Set-up
- Surgeons are seated, facing each other, with the patient’s outstretched arm between them.
- Headlight
- Loupes
- Hand bipolar
Anesthetic Issues
- Monitored anesthesia care in most cases
- General anesthesia for uncooperative or extremely pain-sensitive patients
- Perioperative antibiotics (first generation cephalosporin)
- Pad patient appropriately
Miscellaneous
- A mini-open procedure is generally appropriate for all patients as a first procedure.
- Some practitioners choose to perform endoscopic carpal tunnel release in selected, nondiabetic patients.
- Reoperative carpal tunnel release requires a more extensive open procedure to safely identify normal nerve above and below the previous incision.
- In patients with bilateral disease, one side is performed at a time to ensure the patient has at least one completely functional hand during convalescence.
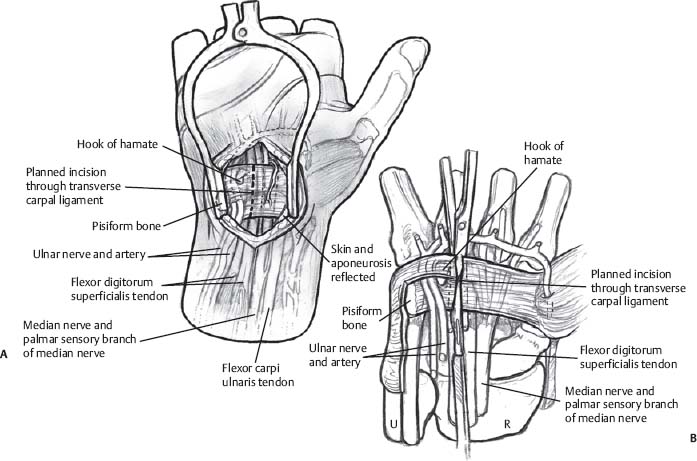
♦ Intraoperative (Fig. 154.1)
Positioning
- Patient is supine with arm outstretched on an armboard.
Planning of Sterile Scrub and Prep
- Chlorhexidine scrub of hand, wrist, and forearm, followed by alcohol paint, followed by Betadine paint that is allowed to dry
- An extremity drape is used to drape hand, wrist, and distal forearm into the field.
- Hand is then placed into the sterile malleable hand holder, with the wrist in moderate extension.
- A 2-cm incision is marked just distal to the distal wrist crease, in line with the radial aspect of the 4th digit; following a natural wrist crease is not necessary but avoiding injury to the more radially-placed palmar cutaneous and recurrent motor branches is.
Technique
- The incision is injected with local anesthetic (four parts lidocaine 0.5% with epinephrine, four parts bupivacaine 0.25%, one part sodium bicarbonate); some practitioners discourage the use of epinephrine in hand surgery; no tourniquet is necessary.
- Incise the skin with a no. 15 blade and place a self retaining retractor. Deeper dissection will reveal the palmar fascia; incise this next and place the retractor deeper to keep the subcutaneous fat out of the way; bipolar may be used to shrink some of the more problematic fat away.
- Incise the distal portion of the flexor retinaculum with a no. 15 blade until the median nerve is seen; use Metzenbaum scissors to completely divide the ligament proximally and distally.
- Have the assistant elevate the skin with a Senn retractor so that all bands of constrictive tissue, including fascia, may be divided for at least 3 to 4 cm proximally and 2 to 3 cm distally beyond the confines of the incision (for a total of 7 to 9 cm of nerve decompression).
- Irrigate, obtain hemostasis, and close with 5–0 nylon vertical mattress sutures.
♦ Postoperative
- Place a bulky dressing that enables the patient to move and use all of the fingers in the immediate postoperative period.
- Encourage patients to use the hand as soon as possible in the postoperative period; however, discourage heavy lifting (carrying groceries, weightlifting, etc.) or excessive force against the incision (push-ups, using hand tools, etc.) for 6 weeks or so postoperatively.
- Occupational therapy may begin 4 to 6 weeks postoperatively.
Only gold members can continue reading. Log In or Register to continue








