Fig. 1
Line of the right eyebrow skin incision started at the midpupillary line and extended laterally. On the left, the supraorbital nerves are represented
The fronto-temporal incision behind the hairline allowed forward tilting of the frontal scalp, being very careful at the proximal part of the temporal muscle. The frontal galea may be tilted up to the orbital rim and the temporal muscle incised at a distance from the temporal line was pushed according to an arciform incision up to the Sylvian fissure.
Craniotomy. The burr hole (single) under the temporal muscle was made at the point of contact with the zygomatic arch. A high speed craniotome determined a straight cutline parallel to the orbital rim from the lateral to the medial position, taking into account the lateral border of the frontal paranasal sinus. A superior c-shaped line-up to the initial hole cut out a small bone flap of 3 cm wide and 2 cm high.
Intracranial steps. The opening dura is made in a curved fashion with its base at the cranial base (Fig. 2). The brain relaxation was patiently obtained by suction of the cerebrospinal fluid (CSF) after opening the chiasmatic and carotid cisterns or the Sylvian fissure. Self-retaining spatulas were used as brain protectors rather than brain retractors. This approach provided, with the help of several cotton balls placed laterally, a correct visualization of the anterior communicating artery complex and the supraclinoid carotid artery area (Fig. 3). With correct brain relaxation, we could open the Sylvian fissure without trauma to the frontal lobe and reach the principal aneurysm location on the middle cerebral artery.
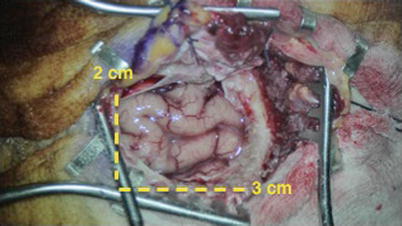
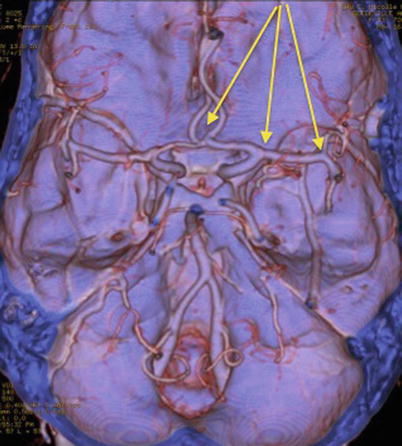
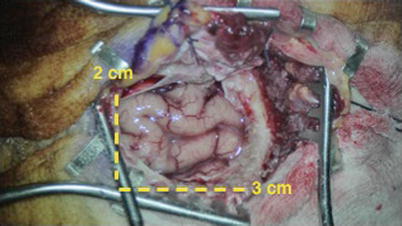
Fig. 2
After removal of the bone flap and durotomy, the frontal lobe and the cranial base are exposed
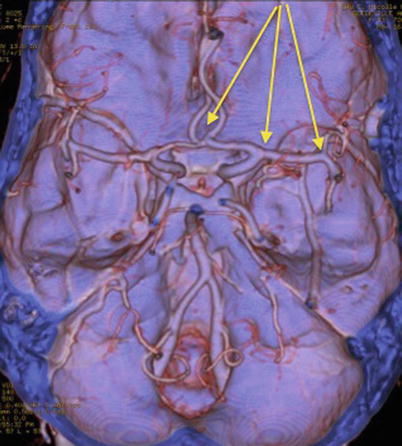
Fig. 3
An angioscanner shows the anterior part of the Circle of Willis and the arrows give the optical view from the mini supraorbital approach to the principal location of intracranial aneurysms
Dural closure and bone flap reconstruction. After aneurysm clipping, the dura mater is closed in a watertight fashion with repair of all defects. The bone flap is replaced and fixed with craniofix©. An autologous osseous graft is interposed between the borders of the craniotomy and the bone flap, recovered by the frontal galeal flap. The temporal muscle is suspended to the zygomatic arch and the skin closed with a subdermal resorbable suture.
Indications, advantages and limitations
This mini-invasive approach is indicated for patients with an unruptured aneurysm, for patients with aneurysmal subarachnoid hemorrhage (SAH) without intracranial hypertension, and especially for elderly patients. In those over age 70, the absence of intracranial hypertension related to the frequent cortical atrophy combined with the reduced operating time favored this approach. The choice of the side was determined by the prediction of the easiest clip application. For an aneurysm on the major bifurcation of the middle cerebral artery, we must take into consideration the relationship between the middle cerebral artery and the sphenoidal wing as well as the length of the M1 segment.
Advantages
This minicraniotomy gives quick and direct access to the aneurysm, reducing the time of the operation [14]. The reduced trauma to the temporal muscle eases the cosmetic reconstruction. The small detachment of the dura mater from the vault decreases the risk of postoperative epidural intracranial hematoma [2, 10, 16]. Moreover, a ventricular drainage through the keyhole is possible. The cosmetic results are excellent after replacement of the bone flap by craniofix® and interposition of osseous bone auto graft into the continuity solution between the bone flap and the osseous vault.
Limitations
The volume of the surgical exposure is smaller than the pterional approach [7, 8]. The intracranial hypertension, whether caused by intraparenchymatous hematoma or cerebral edema, is a formal contraindication to performing this approach. A small craniotomy may cause hinging of the herniating brain against the bone margin. The ventricular catheter may be difficult to put in the frontal horn of the lateral ventricle. In cases of intraoperative rupture of aneurysm, the habit and the control by succor is a key to the success.
How to avoid complications and specific perioperative considerations
Astute patient selection remains the major key point. A perfect preoperative analysis of clinical and iconographic characteristics should allow to better define the most appropriate surgical indications. The absence of intracranial hypertension is the first argument for indication for this procedure. The exposure of the zygomatic arch is crucial to cutting off the flap just at the point of contact with the orbital rim. The second point is to obtain proper brain relaxation before starting the aneurysm dissection. In the case of vascular rupture, it is recommended to never take off the succor in order to control bleeding and to avoid the collection of blood under the brain that is responsible for cerebral hernia.
On the preoperative imaging (cerebral angioscanner and/or cerebral angiography), various points must be checked:
The aneurysm morphology and projections
The symmetry analysis of the anterior communicating artery complex
The lateral extension of the frontal paranasal sinus
The length of M1 segment
The relationship between the sphenoidal wing and the major bifurcation of the MCA
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








