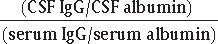
29 True or false: Amyotrophic lateral sclerosis (ALS) is the most common motor neuron disease, and also has the worst prognosis. True What is the typical age of onset and, subsequently, death? Mean age of onset is 60 (range 40–70); mean age of death is 641 Does it affect upper or lower motor neurons? Both; however, in patients in whom involvement is predominately LMN, mean age of onset is later, and latency to death is shorter (68 and 21 months, respectively)2 Are men or women more commonly affected by ALS? In patients <50 years of age, men are more commonly affected by a ratio of 2:1. After age 50, men and women are equally affected. Give examples of upper motor neuron signs. Hyperreflexia Spasticity Loss of dexterity Slow movements Presence of Babinski reflex Name the signs associated with lower motor neuron disease. Hyporeflexia Muscle atrophy Weakness Flaccidity Fasciculations Cramps Where does neuronal degeneration occur in ALS? Primarily in the anterior horns, corticospinal tracts, motor cortex, and hypoglossal nucleus Which functions are routinely spared by the disease? Sphincter function Extraocular muscle function Sensation Is there a genetic component to the disease? Yes; though most cases are sporadic, approximately 10% are autosomal dominant (AD). Are there any differences in the signs and symptoms of ALS in patients with the AD form of disease? Though the disease looks similar to the sporadic form, the AD form is more likely to begin with leg symptoms. Have any genes been identified as responsible for causing the AD form of ALS? Yes, approximately 20% of patients with inherited disease have a mutation in the Cu/Zn superoxide dismutase (SOD1) that results in protein misfolding and a resulting toxic gain-of-function.3 Has protein misfolding been identified in the sporadic form of disease? Yes, in most patients with sporadic ALS, abnormally high accumulations of the nuclear TAR DNA binding protein 43 are found in the cytoplasm of neurons and glial cells.3 How is ALS similar to HIV? An ALS-like syndrome may present in HIV-positive patients, and it has been theorized that ALS is also caused by a (yet unidentified) retrovirus; some authors suggest including HIV in the differential diagnosis of ALS3 Is there any pharmacological treatment for ALS? Riluzole, an inhibitor of presynaptic glutamate release, extends life by 2 to 3 months. What about experimental options? Current phase-3 studies include other antiglutamate agents, heat shock protein gene expression amplifiers, and drugs that increase mitochondrial function.4 Are there any nonpharmacological treatments for the disease that may improve outcome? • Noninvasive positive-pressure ventilation and/or mechanical ventilation • Nutritional intervention Multiple sclerosis (MS) is characterized by signs and symptoms that occur over what two variables? • Time (attacks are separated by at least a month, or symptoms have been progressing for at least 6 months) • Space, or location in the CNS (e.g., optic nerve and cervical spinal cord) What is the most common form of MS? Relapsing-remitting MS is found in approximately 85% of MS patients and is characterized by sporadic “flare-ups,” or attacks, with no progression of symptoms between such episodes. How do primary and secondary progressive MS differ from one another? • Primary progressive MS is progressive from the onset, with no relapses (approximately 15% of patients) • Secondary progressive MS occurs when a relapsing-remitting patient’s course turns progressive, with or without plateaus in symptoms (approximately 50% of relapsing-remitting patients develop secondary progressive MS). Are men or women more affected by MS? Women are more commonly affected, with a younger age of onset (20–35 years of age), whereas men tend to have a more malignant course that begins later in life (35–45 years of age).5 Is there a genetic component to MS? Yes; first-degree relatives have a 10- to 20-fold greater risk of developing the disease. Which HLA alleles are associated with MS? • HLA-DR2: general population • HLA-DR4: Mediterranean patients • HLA-DR15: Northern Europeans • HLA-DW2: Danish patients with relapsingremitting MS What are the major signs and symptoms associated with MS? • Spasticity • Optic neuritis/loss of vision • Weakness/tremor • Paresthesias • Ataxia • Dysarthria • Bowel/bladder dysfunction • Sexual dysfunction • Lhermitte’s sign • Uhthoff sign (heat intolerance transiently resulting in blurry vision) • Trigeminal neuralgia (bilateral trigeminal neuralgia is suggestive of MS) What is optic neuritis, and how would you expect it to present? Decreased central vision and red desaturation, typically unilaterally, and often painful. On ophthalmic exam, one would expect to see a red, swollen optic disk followed by disk pallor and a Marcus-Gunn pupil. Describe the CSF findings you would expect in a patient with MS. What is the IgG index? • Normal opening pressure • Mild protein elevation (typically 50–60) • Elevation of oligoclonal bands • Increased levels of tumor necrosis factor (TNF) and interleukin-6 (IL-6) • IgG index (aka Tourtellott formula): (CSF IgG/CSF albumin) (serum IgG/serum albumin) • Typically the IgG index >0.7 in patients with MS. How are visual evoked potentials useful in assessing MS? They are prolonged in 40% of possible MS cases, 60% of probable cases, 67 to 85% of definite cases, and 70 to 95% of optic neuritis patients (may remain abnormal for years after optic neuritis).5 How do somatosensory evoked potentials and brainstem auditory evoked potentials differ in their utility for evaluating MS cases? Both are prolonged in about half of possible and definite cases of MS, but brainstem auditory evoked potentials are prolonged in 93% of chronic progressive MS patients.5 What is the relationship between MS and the immune system? Patients with MS often have abnormalities of CD8 T cells, so fever, viral infections, and stress can increase attacks.6 Patients typically have a decrease in frequency of flare-ups while pregnant, but they may experience an increase in the postpartum period. What are the two major kinds of treatments offered to MS patients? Immune modulation therapy to minimize/suppress attacks, and symptomatic therapies to address specific symptoms Which drugs are most commonly used as immunomodulators? • Steroids (often a high dose followed by a slow taper for an acute exacerbation) • Interferons (interferon β-1b (Betaseron™), interferon β-1a (Rebif™, Avonex™), glatiramer acetate (Copaxone™), natalizumab (Tysabri™), especially for relapsing remitting MS • Chemotherapeutic agents, such as mitoxantrone, especially for secondary progressive MS Which treatment variable has been shown to have the greatest effect on prognosis in relapsing, remitting MS? Early treatment with immunosuppressant agents to minimize damage to myelin7 What causes myasthenia gravis (MG)? Polyclonal IgG antibodies against nicotinic cholinergic receptors at the neuromuscular junction MG is most commonly associated with abnormalities of what organ? Almost all patients with MG have thymus abnormalities: approximately 75% have lymphoid hyperplasia and approximately 15% have thymomas. Why is the thymus implicated in MG? AChR antibodies are synthesized by the B cells of the thymus. A 25-year-old patient presents to you with MG. Is the patient more likely to be male or female? Female; patients aged 10 to 40 presenting with MG are three times more likely to be female than male. What if the patient were 55? Then the patient is more likely to be male; he is also more likely to have a thymoma than a younger patient would be. True or false: MG commonly occurs in patients who have other autoimmune diseases. True; Graves’ disease and systemic lupus erythematosus (SLE) are common comorbidities. What are the three cardinal symptoms of MG? • Fluctuating weakness: typically waxes and wanes over the course of a day, but is marked by excessive fatigue with exercise
Motor and Demyelinating Disorders
29.1 Amyotrophic Lateral Sclerosis
29.2 Multiple Sclerosis
29.3 Myasthenia Gravis
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






