Multiple Brain Hyperintensities (T2/FLAIR), Common
Gary M. Nesbit, MD
DIFFERENTIAL DIAGNOSIS
Common
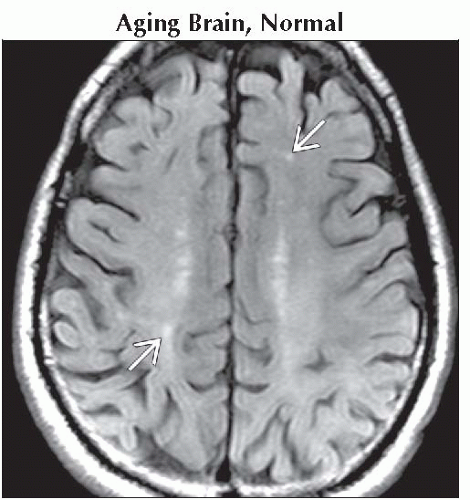
Aging Brain, Normal
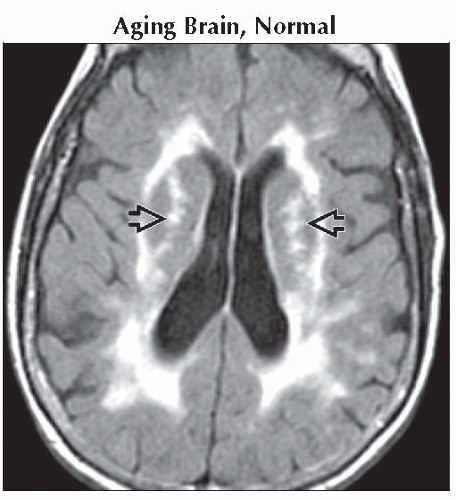
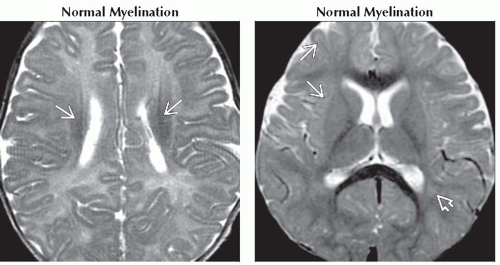
Normal Myelination
Reactive Astrocytosis (Gliosis) & Encephalomalacia
Atherosclerosis, Intracranial
Neurofibromatosis Type 1
Myelin Vacuolization
Enlarged Perivascular Spaces
Mucopolysaccharidoses
Lacunar Infarction
Chronic Hypertensive Encephalopathy
Acute Hypertensive Encephalopathy, PRES
Cerebral Infarct, Subacute
Cerebral Infarct, Chronic
Hypotensive Cerebral Infarct
Cerebral Edema, Traumatic
Cerebral Contusion
Diffuse Axonal Injury (DAI)
Multiple Sclerosis
Metastases, Parenchymal
Lymphoma, Primary CNS
Radiation and Chemotherapy
Periventricular Leukomalacia
ESSENTIAL INFORMATION
Helpful Clues for Common Diagnoses
Aging Brain, Normal
White matter (WM) hyperintensities are normally seen
Rule of thumb: 1 per decade to age 50
Increase in number & size is exponential from age 50 to 100 years
Due to gliosis, leukoariosis, & enlarged perivascular spaces (PVS)
Normal Myelination
T2 hyperintense myelin at birth, except posterior fossa, optic radiations, & corticospinal tracts
Corpus callosum (CC) myelinates from 4 to 9 months, splenium to genu
Parietal & frontal myelination from center to periphery until around 2 years of age
Reactive Astrocytosis (Gliosis) & Encephalomalacia
Brain’s only response to insults: Infectious, stroke, trauma
Gliosis is T2 hyperintense without mass effect, encephalomalacia often associated
Encephalomalacia is a “hole” that follows CSF signal, often surrounded by gliosis
Atherosclerosis, Intracranial
Results in distal emboli or hypoperfusion infarcts
Variable infarct location, depends upon vessel involved
Neurofibromatosis Type 1
Nonenhancing T2 hyperintensities in basal ganglia (BG) & deep cerebellum most commonly (myelin vacuolization)
No mass effect, unlike astrocytoma, the main differential in NF1
Develops in early childhood, peaks around age 8, & usually regresses by late teens
Enlarged Perivascular Spaces
Commonly symmetric & peripheral in WM, but can be unilateral focal & deep
Inferior BG, near anterior commissure common location
Sharp margins & lentiform, follows CSF on T2/FLAIR in young patients
Often associated with gliosis in the elderly (FLAIR hyperintense)
Mucopolysaccharidoses
Dilated PVS usually with surrounding gliosis presenting in infancy
CC & periatrial WM most common
Lacunar Infarction
Usually in lenticular & caudate nuclei, thalamus, internal capsules, periventricular WM
Acute: T2 hyperintense, diffusion positive
Chronic: Focal encephalomalacia with surrounding gliosis
Chronic Hyperintensive Encephalopathy
Usually deep & periventricular WM confluent hyperintensities
Often associated with T2 hypointensities from microhemorrhage on GRE images
Acute Hypertensive Encephalopathy, PRES
Peripheral subcortical confluent hyperintensities, mild mass effect
Bilateral occipital parietal is common, but many variations including hemorrhage
Cerebral Infarct, Subacute
Embolic infarcts usually cortical, wedge-shaped with mass effect
Microembolic infarcts are usually peripheral centrum semiovale or BG
Enhancement typical
Cerebral Infarct, Chronic
Results in focal encephalomalacia & gliosis
Typically in a major vascular distribution
Hypotensive Cerebral Infarct
Watershed infarcts
Parasaggital linear “string of pearls” in the centrum semiovale
Wedge-shaped regions in the border zone between vascular distributions
Diffuse or multifocal cortical infarcts & BG
Diffusion positive acutely
Cerebral Edema, Traumatic
Cerebral swelling without T2 change early, may develop hyperintensities
Contusion & DAI commonly with hemorrhage
Cerebral Contusion
Cortical, subcortical hyperintensities with developing hemorrhage
Regions of injury: Temporal, frontal lobe, superficial brain with direct trauma
Diffuse Axonal Injury (DAI)
Shear stress deceleration injury: Gray-white, midbrain hemorrhage; diffusion positive early
Typically in older children to young adults, as there is minimal subarachnoid space & brain movement
Multiple Sclerosis
CC & peri 4th ventricular involvement characteristic
Radiating periventricular location, “Dawson fingers”
Acute tumefactive lesion: Large with T2 hypointense ring that enhances, usually little mass effect
Metastases, Parenchymal
Hyperintensities may be punctate to massive, with variable surrounding edema, mass effect
Hyperintensity, edema, & mass effect less prominent in posterior fossa, but risks higher
Lymphoma, Primary CNS
Central region nearly T2 isointense due to high nuclear to cytoplasmic ratio
Surrounding edema variable, usually crossing or around CC in immunocompetent
Immunocompromised PCNSL will have multifocal ring-like “glioblastoma” look
Radiation and Chemotherapy
Radiation leukomalacia: Confluent poorly marginated regions in the radiation field without enhancement
Radiation necrosis: Irregular ring-enhancing lesions with variable mass effect, may grow, CBV/choline low
Periventricular Leukomalacia
WM volume loss, gliosis, & focal cystic lesion in the periatrial WM
Associated with prematurity
Image Gallery
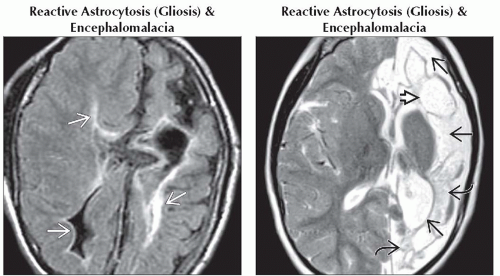 (Left) Axial FLAIR MR shows profound asymmetric periventricular white matter volume loss & hyperintensity indicative of gliosis
 , along with generalized left greater than right atrophy in this microcephalic 14 year old. (Right) Axial T2WI MR shows volume loss with enlarged subarachnoid, sylvian, & ventricular CSF spaces , along with generalized left greater than right atrophy in this microcephalic 14 year old. (Right) Axial T2WI MR shows volume loss with enlarged subarachnoid, sylvian, & ventricular CSF spaces  , CSF isointense cystic encephalomalacia , CSF isointense cystic encephalomalacia  , & mixed intensity gliotic brain , & mixed intensity gliotic brain  in this patient with chronic hemispheric infarction. in this patient with chronic hemispheric infarction.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|