Neocortical Resections
Youssef G. Comair
Paul C. Van Ness
Roukoz B. Chamoun
Carmel H. Bouclaous
Introduction
The histories of extratemporal epilepsy, epilepsy surgery, and neurosurgery are intimately related. The intractability of posttraumatic epilepsy led to the early use of trephination as a treatment modality. In the eighteenth century, Percivall Pott, a British neurosurgeon, established that the brain rather than the skull was responsible for the seizures. Posttraumatic scars were often focal and offered guidance for early neurosurgeons into the functional anatomy of the brain. The era of modern neurosurgery was ushered in by Sir Victor Horsley,46 who introduced asepsis, anesthesia, and the new science of cerebral localization. He also described the technique of subpial cortical dissection and resection, a standard technique used by epilepsy surgeons today.
The seizure outcome after surgical management of patients with temporal lobe epilepsy is excellent in most of the recently reported series,73 and a recent randomized, controlled trial comparing surgical to medical treatment showed a significantly better outcome in the surgical group.136 However, the results of surgery in extratemporal epilepsy are less encouraging. Many factors seem to account for this difference: Whereas mesial temporal sclerosis constitutes the majority of temporal lobe epilepsies, extratemporal epilepsy is a more heterogeneous group and lacks a common pathologic substrate. Furthermore, the difficulty in interpreting the semiology, the uncertainty of the localizing value of the different studies performed, and the vicinity of eloquent areas to the epileptogenic focus in many of these cases appear to decrease the chances of obtaining an excellent outcome.
In spite of the difficulties previously mentioned, recent radiologic and neurosurgical advances undoubtedly revolutionized this field: Modern anatomic and functional imaging are able to detect more-discrete lesions, and neurosurgical techniques help to optimize resections while minimizing morbidity.
Historical Perspectives
Impact of Neuroimaging
The advent of magnetic resonance imaging (MRI) and its ever-improving sensitivity in detecting cerebral abnormalities had its greatest impact on the surgical management of neocortical epilepsy. With the improvement in the anatomic details provided, more-subtle variations are being observed and a larger number of patients are being diagnosed as harboring neoplastic or developmental lesions. Nevertheless, even with these advances, MRI was unrevealing in 39% of histologically verified focal cortical dysplasia in a recent study,22 and it has been estimated that ∼25% of cases with refractory epilepsies have normal MRI.67,120
Overall, MRI is more sensitive in detecting tumors than neuronal migration disorders,47 and in general, the detection of abnormalities by MRI is known to be associated with good surgical outcome.47,69,147
Impact of Pathology and Electrophysiology
Whereas most temporal lobe epilepsy (TLE) is characterized by hippocampal pathology,12,61,62 neocortical epilepsy lacks a common pathologic substrate. A wide range of structural anomalies has been associated with chronic partial neocortical epilepsy. These anomalies can be classified into five large categories: (a) malformative, (b) tumoral, (c) ischemic, (d) traumatic, and (e) infectious. In a small number of patients, the nonspecific substrate of gliosis is found. Most of these lesions are not believed to be epileptogenic per se; rather, the epileptogenicity is due to excitability of the surrounding cortex. Numerous mechanisms have been implicated.104,105 These include neurochemical changes, pressure effect, and ischemia. In the congenital malformative diseases, intrinsic epileptogenicity has been established with recording of continuous ictal epileptogenic discharges on electrocorticography.86 Dual or multiple pathologic substrates are increasingly detected owing to advances in imaging techniques and careful pathologic studies from large surgical series. The occurrence of hippocampal volume loss in association with pathologies outside of the archipallium are examples of distant but coexistent disease.17,66,72,101 Furthermore, the coexistence of dysplastic and neoplastic disease has been established in developmental tumors, for example, gangliogliomas and dysembryoplastic neuroepithelial tumors (DNETs).50 This has important consequences for the surgical strategies, which are generally designed to resect all identified pathology for best results. In fact, the identification and resection of all focal pathology is considered a predictor of good outcome following neocortical resection.
Indications
Principal Candidates
The indications for surgery are discussed in the chapters referring to the surgically remediable syndromes (see Chapters 167,168,169). Briefly summarized, three major groups are identified.
The first group consists of lesional, nondevelopmental pathology causing partial epilepsy. A majority of these patients continue to have intractable epilepsy despite antiepileptic drugs
(AEDs). A favorable outcome following resective surgery is expected, often with lesionectomy alone. The second group consists of developmental abnormalities causing partial epilepsy and is characterized by a more diffuse pathology and difficulty in precisely localizing the ictal onset zone (Table 1). Patients in this category are considered for surgical treatment only following failure of AEDs. The third group has partial epilepsy without evidence of a lesion on MRI or metabolic imaging. This is the most difficult subgroup of patients who have less favorable results following resective surgery. These patients should be investigated in an experienced epilepsy surgery center.
(AEDs). A favorable outcome following resective surgery is expected, often with lesionectomy alone. The second group consists of developmental abnormalities causing partial epilepsy and is characterized by a more diffuse pathology and difficulty in precisely localizing the ictal onset zone (Table 1). Patients in this category are considered for surgical treatment only following failure of AEDs. The third group has partial epilepsy without evidence of a lesion on MRI or metabolic imaging. This is the most difficult subgroup of patients who have less favorable results following resective surgery. These patients should be investigated in an experienced epilepsy surgery center.
Table 1 Developmental abnormalities associated with epilepsy | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
Evaluation Criteria
The goal of the evaluation criteria is to identify the epileptogenic zone, or the area of abnormal brain tissue responsible for genesis of the seizures, and its relationship to essentially normal brain. In this respect, the stages or steps in the presurgical evaluation are essentially similar to the evaluation of temporal lobe epilepsy. These steps include neuroimaging, interictal and ictal recordings with video-electroencephalography (EEG), neuropsychological testing, and the Wada test for speech lateralization. The value of the sodium Amytal test for memory localization in neocortical epilepsy is unclear57 because in a significant number of patients a decreased memory reserve is noted without evidence of limbic disease.
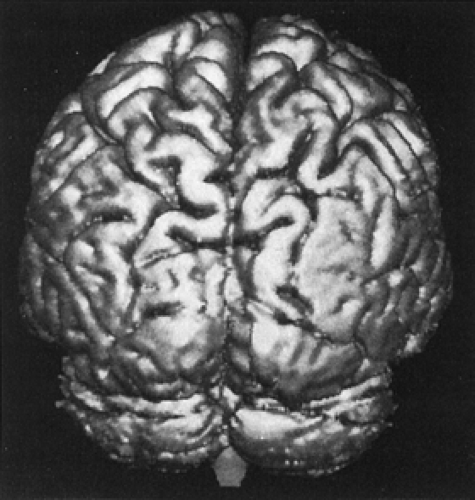
Careful anatomic imaging is essential and should be performed early in the presurgical evaluation so as to guide the electrophysiology evaluation and correlate it with the lesional pathology using magnetic resonance imaging protocols. The specific sequences are evolving and at present include (a) a coronal, high-resolution volumetric acquisition (e.g., three-dimensional [3D] spoiled gradient-echo [SPGR]) in the coronal plane to produce 2-mm contiguous slices of the entire brain (flip angle 10/TR 11/TE 4.4/TI 300/250 mm Fov/192 × 256 matrix); (b) a conventional double-echo T2-weighted sequence in the coronal or axial plane (TR 2000/TE 20, 80/230 mm Fov/192 × 256/5 mm slice/2 mm gap); and (c) a two-dimensional fast fluid-attenuated inversion recovery (FLAIR) sequence in the coronal or axial plane (TR 2000/TE 80/TI 2400/230 mm Fov/192 × 256/5 mm slice/2 mm gap). The combination of the conventional pulse sequences is used to characterize a structural abnormality using morphology, signal intensity characteristics, and, if appropriate, the degree of enhancement with gadolinium. The fast FLAIR sequence has been particularly useful in localizing structural abnormalities of the neocortex and archicortex because it is essentially a heavily T2-weighted sequence with dark cerebrospinal fluid (CSF). This contrast results in increased conspicuousness of peripheral cortical lesions or subtle underlying white matter abnormalities that may be identifiable on the conventional pulse sequences only in retrospect. The volumetric acquisition is then used to further characterize morphology, accurately localize the lesion within the brain, and precisely define its 3D spatial relationships relative to adjacent normal brain. The 3D study is also specifically designed so that the data can be reformatted along any orthogonal or oblique plane without significantly compromising image quality or subjected to alternative postprocessing algorithms (surface reconstruction, volumetric analysis). This has been proven to be especially helpful in the identification of subtle neocortical developmental anomalies121 (e.g., small focus of polymicrogyria or more subtle cortical disorganization) (Fig. 1) or very mild volume loss in the archicortex. Hippocampal volumetric data are obtained when a dual pathology is suspected.17
The role of positron emission tomography (PET) scanning in neocortical epilepsy is controversial.1,128 In patients in whom a lesion is identified on MR, the PET scanning role is superfluous because the relationship between the ictal onset zone and the hypometabolic zone, when identified, has not yet been determined. Interictal PET has been carried out mainly with fluorodeoxyglucose and flumazenil. In temporal lobe epilepsy it demonstrates hypometabolism in 60% to 90% of patients; however it is less sensitive in extratemporal epilepsy (45%–60%).42,118 Flumazenil-PET may have a higher sensitivity than fluorodeoxyglucose-PET in delineating the epileptogenic zone in extratemporal cases,75 but these findings need further study for confirmation.
Single photon emission computed tomography (SPECT) scanning performed interictally, and particularly ictally, can be of help in the localization of neocortical epilepsy. Ictal SPECT is complicated by the need to deliver the radiopharmaceutical early in the ictal phase and poor resolution leading to variable interpretation. The SPECT information should be used judiciously and carefully correlated with the electroclinical syndrome. Recent studies tried to establish its sensitivity and specificity. The following results were obtained when SPECT was compared to intracranial EEG recordings (considered as gold standard): Interictal SPECT was consistent with intracranial EEG localization in 33% of patients and was normal in 52% of
patients in whom seizures were localized by intracranial EEG. On the other hand, ictal SPECT was consistent with the intracranial localization in 74% of patients and was normal in 7% of cases in which seizures were localized by intracranial EEG. The presence or absence of a structural lesion did not appear to affect the reliability of ictal SPECT in this study.126
patients in whom seizures were localized by intracranial EEG. On the other hand, ictal SPECT was consistent with the intracranial localization in 74% of patients and was normal in 7% of cases in which seizures were localized by intracranial EEG. The presence or absence of a structural lesion did not appear to affect the reliability of ictal SPECT in this study.126
SISCOM (subtraction SPECT coregistered to MRI) refers to the subtraction of ictal and interictal SPECT scans with subsequent coregistration to MRI. This technique is clearly superior to conventional visual analysis and appears to be a better predictor of surgical outcome.78,111
Several centers have reported the use of proton MR spectroscopy in nonlesional epilepsy.76,77 The high-resolution metabolic imaging is combined with precise delineation of anatomic structures. Decreased N-acetylaspartate (NAA) and increased choline are seen interictally. Postictally, a focal increase in lactate36 appears to correlate with the ictal onset zone.
Goals of Surgery in the Ideal Candidate
The goal of the surgery is to render the patient seizure free without disturbances in cognitive function and off or with decreased antiepileptic medications. This goal can be reasonably achieved in patients with localized pathology and concordant with the electroclinical syndrome. In the less-than-ideal candidate, when a seizure-free outcome is less likely, surgery is undertaken when there are significant chances of seizure improvement and psychosocial gain.
Surgical Approaches
Reliance on the Presurgical Evaluation
History, Neurologic, and Cognitive Examination
In establishing the electroclinical syndrome, the history and physical examination are paramount, and family and friends can provide important information. The familial and prenatal histories yield clues to genetic susceptibility or early insults. Information concerning the natural evolution of the seizure pattern is gathered, particularly the presence of an aura, as well as findings of the various seizure types and response to medication for each type. The semiology of the ictal phenomenon can yield important clues to locate the generator. In some patients, subtle neurologic deficits are noted, which helps in the localization process. The cognitive deficits should be interpreted in relation to dominance established by the Wada test.133 It is essential to establish the lateralization of speech in neocortical epilepsy because there is a high incidence of unusual speech lateralization in this patient population, particularly with an early age of seizure onset.
Scalp and Invasive Electroencephalography
Scalp EEG with interictal and ictal recordings are essential in the localization process of focal epilepsy. The distribution of interictal discharges correlates better with the extent and location of the epileptogenic zone than ictal recordings. Because in neocortical epilepsy the epileptogenic zone is larger than in temporal lobe epilepsy, the interictal discharges tend to be widely distributed. In addition, the availability of several pathways of propagation results in a poor localization of the ictal discharges. False localization–lateralization occurs in 28% of occipital and 16% of parietal lobe epilepsies. Generalized ictal onsets are noted in mesial frontal and occipital lobe epilepsies. Lateral frontal and parietal lobe seizures frequently have a localized onset.
To further define the ictal onset area, several classes of invasive electrodes have been introduced.70 These consist of electrodes of intermediate invasiveness such as epidural pegs, foramen ovale, and more invasive electrodes such as depth, subdural grid, and strip electrodes. Each type offers specific advantages and disadvantages, and these are reviewed in Chapters 170 and 171. Recently, with the introduction of advanced MR techniques, there has been less reliance on invasive electrodes in the preoperative workup.
Functional Mapping
When the lesion or the epileptogenic zone involves or is adjacent to eloquent cortex, functional mapping should be performed so that a safe and complete resection is possible. Mapping is usually performed when resections are contemplated in the central area, dominant inferior frontal cortex, dominant temporal lobe posterior to the precentral sulcus, and the dominant parietal lobe and occipital lobe. A variety of mapping methods is available (see Chapters 173,174,175), and newer, noninvasive methodologies are being assessed, for example, functional MR techniques10,24,63,79 and magnetoencephalography.
Awake Craniotomy
This technique has been facilitated with the introduction of propofol anesthesia71 (refer to Chapter 174 for complete description of the method). Patient cooperation and an anesthesiologist familiar with the technique are essential.4 This technique provides continuous feedback while the patient is maintained awake during resections adjacent to language areas. An awake craniotomy is difficult to perform in children, who, therefore, may require an implanted grid and extraoperative language mapping.2
Acute Mapping Using General Anesthesia and Intubation
Cortical stimulation can be performed in the primary motor cortex with judicious use of short-acting muscular blockade agents, low concentrations of inhalation agents, and the substitution or addition of propofol, with adequate responses. This may be supplemented by somatosensory-evoked potentials to map the postcentral gyrus.143
Chronic Mapping Using Subdural Electrodes
This method offers several advantages because it allows repeated stimulation under variable intensities and with full patient cooperation. Cortical areas that are difficult to stimulate acutely, such as the dominant posterior basal temporal lobe and occipital and medial frontal lobe, can be carefully investigated using this method. The area to be stimulated and potentially resected can be thoroughly discussed with the patient preoperatively. There are several disadvantages to this technique. The functional areas seem to be wider than on acute studies,41 which would indicate that this may be due to the larger grid electrode size, the method of stimulation, and simultaneous responses from adjacent gyri and current spread. The cost of this investigation is high. Infections are a rare but serious complication.
Functional Magnetic Resonance Imaging
Functional MRI (fMRI) allows noninvasive functional mapping. The combination of echo-planar imaging (EPI), which is a fast magnetic resonance imaging technique, with the blood oxygenation level–dependent (BOLD) method allowed functional brain imaging. fMRI studies have used successfully in
identification of the primary motor and sensory cortex.40,54,97 Cortical simulation and fMRI activation were found to lie within 3 to 5 mm of each other.35 On the other hand, fMRI of language processing has focused on language lateralization and, to a lesser extent, on localization. Numerous studies showed excellent agreement of the fMRI lateralization with the intracarotid amobarbital test or electrocorticography.28,44 The value of speech localization by fMRI remains unclear.14,32
identification of the primary motor and sensory cortex.40,54,97 Cortical simulation and fMRI activation were found to lie within 3 to 5 mm of each other.35 On the other hand, fMRI of language processing has focused on language lateralization and, to a lesser extent, on localization. Numerous studies showed excellent agreement of the fMRI lateralization with the intracarotid amobarbital test or electrocorticography.28,44 The value of speech localization by fMRI remains unclear.14,32
Reliance on Preoperative Substrate
Developmental Substrate
Malformations of cortical development are frequently associated with intractable epilepsy. From 8% to 12% of patients with partial epilepsy are found to have cortical dysplasia. It is expected that, with the improvement in MRI technology, this incidence will increase as a significant number of patients with negative MRI show cortical dysplasia on surgical specimen. Recently reported surgical series show that cortical dysplasia is the leading etiology in patients subjected to epilepsy surgery.34,134,142,147
The term focal cortical dysplasia was initially used by Taylor et al. in 1971.125 Subsequently this term has been used for a wide range of abnormalities. There is a general agreement that classifications based on pathologic findings are the most useful. These have adopted a three- or four-tier classification with minor, moderate, and severe disruption of cortical structure. The Taylor type represents the most extensive disruption.
The mild dysplasia, classified also as type 1a or architectural dysplasia, consists of cortical dyslamination with or without poorly differentiated cells and occurs mostly in the temporal lobe in association with hippocampal sclerosis. MRI is frequently negative or shows focal hypoplasia and gray–white matter blurring. The moderate dysplasia, or type 1b or cytoarchitectural dysplasia, consists of disruption of cortical layering with giant neurons. MRI, when positive, shows focal hypoplasia but no significant signal alterations. PET and SPECT are important imaging methodologies in the localization of the epileptogenic zone.
The Taylor-type dysplasia, or types 2a and 2b, is characterized by the absence of cortical layering and the presence of giant dysmorphic neurons with or without balloon cells. MRI often detects these lesions as focal thickening of the cortex and blurring of the gray–white matter junction. A funnel-shaped increased signal intensity on T2 with its summit reaching the ventricle is characteristic of the Taylor-type dysplasia with balloon cells.
In general, postoperative seizure control is less favorable than with other lesions, such as tumors or vascular lesions. A seizure freedom rate ranging between 35% and 55% was reported in many series.45,85,95,144 A number of studies suggest an influence of the histopathology on the seizure outcome, with the presence of milder histologic abnormalities being a predictor of a better outcome.31 Nevertheless, the presence of balloon cells (even though a sign of a more severe abnormality) was also associated with a favorable outcome.21,124,132
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree